Journal of
eISSN: 2379-6359


Case Report Volume 17 Issue 1
Correspondence: Dr. Apoorva Kumar Pandey (MS. ENT) Professor, Department of ENT and Head-Neck Surgery, SGRR Institute of Medical & Health Sciences, Dehradun, 248001, Uttarakhand, India., Tel 09411324477
Received: March 12, 2025 | Published: March 26, 2025
Citation: Nautiyal S, Pandey AK, Ahmed S, et al. The clinical presentation of nasolabial epidermal inclusion cyst: a case report. J Otolaryngol ENT Res. 2025;17(1):25-27. DOI: 10.15406/joentr.2025.17.00560
A naso-labial cyst is also known as a Klestadt cyst. It is also known by many names such as nasolabial cyst, nasal alveolar cyst, nasal vestibule cyst, nasal mucocele and alar cyst. It is a benign, slow-growing, non-odontogenic soft tissue lesion located in the alar region of the nose just below the nasolabial fold. The most common complaints are swelling in the nasolabial fold and nasal obstruction. These cysts are more common in females and are usually found between the ages of 40 and 50. The sub-labial approach and trans-nasal marsupialization are the preferred surgical techniques for cyst removal. There are many theories about what causes the cysts. Here, we present a 14-year-old female patient with a facial nasolabial cyst and share our experience in the diagnosis and treatment of nasolabial cysts.
Keywords: nasolabial cyst, sub-labial excision, non-odontogenic
The nasolabial cyst is a rare non-odontogenic cyst arising from facial tissues according to Allard, Zuckerkandl first described this condition in1882.1 These are rare cysts and account for 0.7% of all jaw cysts. Most of the cysts are unilateral, and bilateral presentations are rare. They are slow-growing and asymptomatic, but when symptoms occur, they can cause facial deformity and nasal obstruction.2 There are three different theories regarding the formation of Klestadt cysts. The first impression is that it is a retention cyst originating from the mucosal glands. The second view put forward by Klestadt is that it originates from the embryonic epithelium between medial nasal, lateral nasal, and the maxillary processes. The third theory was put forward by Bruggeman, who suggested that the cysts originate from the remnants of the nasolacrimal duct epithelium.3 CT and MRI are two important imaging methods that show the location of the lesion and its relationship with the surrounding structures. CT imaging is preferred because it is less expensive than MRI, but MRI provides similar tissue images without ionizing radiation. X-rays are of no importance unless there is bone erosion.4 Histopathological examination shows that the Cysts are mostly lined with pseudo-stratified columnar epithelium, but stratified squamous, cuboidal epithelium and goblet cells can also be seen. The supporting tissue is fibrous and sometimes contains skeletal muscle elements.5 The best method for treating nasolabial fold cysts is surgical resection with an intraoral sub-labial or trans-nasal endoscopic approach, which has excellent results and low costs. In a recent surgical trend, a transnasal endoscopic approach under local anesthesia was also used which reduced operative time, pain and lower complication rates but it can cause stenosis and more recurrence rates.6 Here, we present the case of a 14-year-old girl with a nasolabial fold cyst presenting as a palpable facial swelling and share our experience in the diagnosis and treatment of nasolabial fold cyst.
A 14-year-old female patient presented in OPD with a chief complaint of left-side palpable facial swelling for a month, which was painless and gradually progressive in onset. There was no history of trauma, pain, nasal obstruction, nasal bleeding, fever, and any previous surgery. On examination of the face, there was an oval localized swelling of around 2.5 x 2 cm in size on the left nasolabial region. The patient had no previous scar marks or any blood/pus discharge. On palpation, the swelling was firm, cystic, fluctuant, non-tender, mobile, compressible but non-reducible. It was extending from the floor and lateral wall of the nose to the nasolabial groove. On intraoral examination, there was a smooth, fluctuant mass lateral to the upper central incisors in the oral vestibule. The mucosal surface of maxillary vestibule was normal. Anterior rhinoscopy showed there was DNS to the left with normal nasal mucosa. The rest of the ENT and neck examination was normal (Figure 1).

Figure 1 Preoperative photographs of the patient showing obliteration of the nasolabial fold on the left side.
Non-contrast CT of the face was done and it revealed one well-defined hyper-dense lesion on the left side of the nasal ala at the nasolabial fold. The lesion measured (22x 19) mm in largest diameter. There was no evidence of bone erosion (Figure 2).
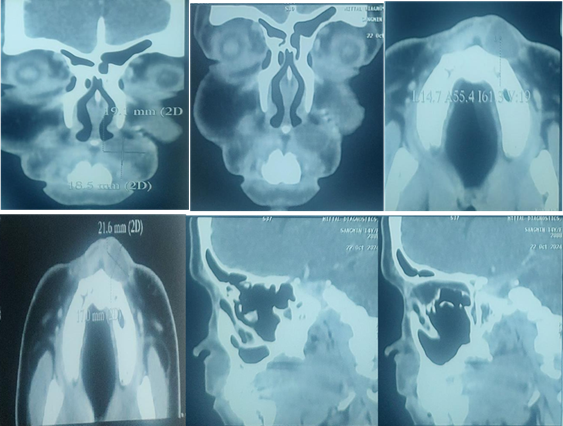
Figure 2 NCCT face (coronal, axial and sagittal cuts) showing a cyst measuring (22 x 19) mm in largest diameter.
Based on the above findings surgical planning of nasolabial cyst excision via sublabial approach under general anesthesia was done. 1:100,000 adrenaline was infiltrated in the labial mucosa. The incision was given in the upper labial mucosa extending from the lateral incisor to the second molar. Blunt dissection was done. The cyst was visualized and hemostasis was achieved. The cyst was meticulously dissected and separated from labial mucosa. Cyst was excised in toto and sent for HPE. The wound was closed in layers and the patient wasshifted to post-op under stable conditions (Figure 3). On histological analysis, it shows an inflammed epidermal inclusion cyst (Figure 4).
Klestadt cyst are known by many names but the most common being used are nasolabial cysts and nasoalveolar cysts. Nasolabial cysts account for approximately 0.7% of all facial cysts and 2.5% of non-odontogenic cysts. Nasolabial cysts are usually unilateral and less commonly occur laterally, although bilateral cysts have been reported.1 Nasolabial cysts are more common in black people. Women are more prone to the disease, with a female-to-male ratio of 4:1. Although nasolabial folds are usually asymptomatic, facial deformity and nasal obstruction may occasionally occur.2
Computed tomography (CT) may show bone resorption, but MRI is the gold standard for diagnosing Klestadt cyst. Magnetic resonance imaging can visualize the lesion's internal details and the wall structure better than CT. Other non-odontogenic cysts and odontogenic diseases should also be considered in the differential diagnosis. Benign or malignant tumors should also be kept in mind.3 Microscopic examination of the cyst revealed that edges were composed of pseudo-stratified columnar and cuboidal epithelium containing goblet cells, indicating a nasolabial cyst.4
The current management for nasolabial cysts is complete excision of the cyst. The goal of the treatment is to reduce infection, establish a proper histopathological diagnosis, and improve the cosmetic deformity. The most common excision method is a sublabial incision made in the upper lip maxillary groove. Care should be taken during surgery to not injure the cyst and it should be completely removed. Methods such as simple aspiration, injection of sclerosant, cauterization, marsupialization, needle aspiration, incision, and drainage have been described for the treatment of cysts, but these methods cause high chances of recurrence. Endoscopic marsupialization removal has also been reported.5
The most common postoperative complications are numbness of the lips or teeth; since cysts often involve the base of the nose, removal of the cyst may cause perforation of the nasal mucosa. Perforations can be left untreated when very small, but larger perforations may need to be sutured.7 As of now, in our case one month after the operation, the patient's wound has healed satisfactorily and there are no external scars, and facial symmetry is normal.
Nasolabial cysts grow slowly and may remain asymptomatic for a long time, but over time they may cause symptoms such as nasal obstruction and facial deformity. Definitive diagnosis is made by clinical, radiological, and histopathological examination. The best treatment method for nasolabial cysts is surgical excision using the intraoral sub labial approach or the Trans nasal endoscopic approach. Since it is often confused with apical disease, every physician must be familiar with the characteristics of this disease to avoid inappropriate treatment.
None.
The author declare that there are no conflicts of interest.

©2025 Nautiyal, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.