eISSN: 2377-4304


Case Report Volume 16 Issue 1
Department of Obstetrics and Gynecology, Iwate Medical University School of Medicine, Iwate, Japan
Correspondence: Tsukasa Baba, Department of Obstetrics and Gynecology, Iwate Medical University School of Medicine, Iwate, Japan, Tel +81-91-613-7111, Fax +81-91-622-1900
Received: February 01, 2025 | Published: February 13, 2025
Citation: Kaido Y, Jonai N, Oshikiri M, et al. Laparoscopic repair of obturator nerve injury during pelvic lymphadenectomy: a case report. Obstet Gynecol Int J. 2025;16(1):29-30. DOI: 10.15406/ogij.2025.16.00783
Obturator nerve injury is a rare complication of pelvic lymphadenectomy in gynecologic oncology. We report a case of intraoperative obturator nerve transection and its successful laparoscopic repair. A 73-year-old woman with stage IB1 cervical cancer underwent laparoscopic radical hysterectomy with pelvic lymphadenectomy. The right obturator nerve was inadvertently transected but successfully repaired laparoscopically using 4-0 polyglactin sutures. Postoperatively, she had mild thigh adduction weakness but recovered nearly fully within three months. At 45 months, she remained recurrence-free with no neurological sequelae. Careful nerve identification is crucial during lymphadenectomy to prevent injury. If transection occurs, immediate laparoscopic repair with tension-free and end-to-end suturing is feasible and effective, ensuring favorable functional outcomes.
Keywords: obturator nerve injury, laparoscopic repair, pelvic lymphadenectomy, gynecologic oncology, nerve anastomosis
Obturator nerve injury is a rare but significant complication of pelvic lymphadenectomy for cervical and endometrial cancer. A study of 1,584 gynecologic cancer surgeries reported an incidence of only 0.2%.1 While transient sensory or motor disturbances due to nerve compression or stretching often resolve without intervention, complete nerve transection can cause substantial functional impairment, affecting patients' quality of life. Therefore, both prevention and effective management strategies are crucial.
With advancements in minimally invasive surgery, laparoscopic pelvic lymphadenectomy has become widely adopted. However, reports on intraoperative obturator nerve injury and its laparoscopic repair remain scarce. Here, we present a case of obturator nerve transection during laparoscopic pelvic lymphadenectomy for a malignant uterine tumor. The nerve was successfully repaired intraoperatively using a laparoscopic approach, and the patient recovered without significant neurological sequelae.
A 73-year-old Japanese woman (gravida 2, para 2) was diagnosed with squamous cell carcinoma (SCC) based on cervical cytology and was initially referred to another hospital. A cervical biopsy suggested microinvasive carcinoma, prompting conization. Postoperative histology confirmed SCC, stage IB1, with positive surgical margins. She was then referred to our hospital for definitive treatment. MRI showed no distinct cervical lesions, and contrast-enhanced chest-to-pelvis CT revealed no lymph node enlargement or distant metastases.
Laparoscopic radical hysterectomy with bilateral salpingo-oophorectomy and pelvic lymphadenectomy was planned. During lymph node dissection in the right obturator region, the right obturator nerve was inadvertently transected. A postoperative review of the surgical video confirmed that the transection occurred due to a power device. After completing the lymphadenectomy, we confirmed that the severed nerve ends could be approximated (Figure 1). Laparoscopic repair was performed using three sutures with 4-0 polyglactin (Figure 2), with vascular tape used to retract the external iliac vessels and expand the obturator space (Figure 3).
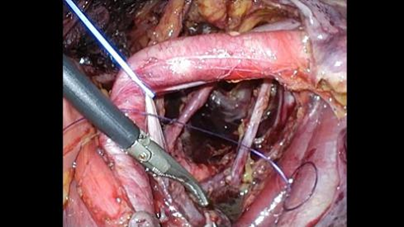
Figure 3 Laparoscopic view showing retraction of the external iliac vessels using a vessel tape to the opposite side, allowing expansion of the obturator space for suturing.
The total surgical time was 402 minutes, with 61 mL of blood loss. The nerve repair took approximately 18 minutes. A total of 35 lymph nodes were removed, and no residual lesions were found in the uterus.
Postoperatively, the patient exhibited mild weakness in right lower limb flexion and adduction but was able to walk independently without assistive devices. Initial ambulation was supervised as a precaution, but she was discharged on schedule. Three months postoperatively, her symptoms had completely resolved. At the latest follow-up, 45 months postoperatively, she remained recurrence-free with no neurological sequelae.
The obturator nerve, originating from L2–L4, plays a crucial role in both motor and sensory functions, innervating the adductor muscles and providing sensation to the medial thigh. Although direct trauma to the obturator nerve is rare, it can occur during pelvic lymphadenectomy in gynecologic and urologic surgeries. A study of 1,584 gynecologic cancer surgeries reported an incidence of only 0.2%.1
In this case, incomplete identification of the obturator nerve’s full course, particularly its proximal segment, led to inadvertent transection during lymph node dissection. Notably, 80% of obturator nerve injuries occur proximally.2 The magnified view provided by laparoscopic surgery can aid in preventing such injuries, underscoring the importance of thorough nerve identification throughout the lymphadenectomy field.
When transection occurs, immediate end-to-end nerve repair is essential, with tension-free suturing being critical for optimal recovery. Although reports on the laparoscopic or robot-assisted repair of completely transected obturator nerves in gynecologic malignancies are limited, successful outcomes have been documented.3–5 These repairs, typically performed using fine sutures (4-0 to 6-0), have been associated with minimal postoperative functional impairment (Table 1).
|
Reference number |
Age |
Disease |
Surgical approach |
Suture material |
Neurological outcome |
|
Our case |
73 |
Cervical cancer |
Laparoscopic surgery |
4-0 polyglactin |
Fully recovered |
|
3 |
63 |
Endometrial cancer |
Laparoscopic surgery |
4-0 polypropylene |
Fully recovered |
|
4 |
76 |
Endometrial cancer |
Robot-assisted surgery |
4-0 polyglactin |
Fully recovered |
|
5 |
44 |
Cervical cancer |
Laparoscopic surgery |
6-0 polypropylene |
Fully recovered |
Table 1 Reports on intraoperative end-to-end suturing of a completely transected obturator nerve during laparoscopic surgery for gynecologic malignancies
In this case, laparoscopic repair using three 4-0 polyglactin sutures resulted in a favorable outcome. Although braided sutures carry a risk of infection due to fluid absorption, they are also rapidly absorbed. While the absorption rate is important for nerve regeneration, Monocryl is also considered to reduce the risk of infection.
If primary anastomosis is not feasible due to excessive tension, nerve grafting should be considered. Nevertheless, with regard to long-term neurological outcomes, end-to-side anastomosis and nerve grafting are equivalent, but end-to-side anastomosis has been reported to have superior postoperative muscle strength and a tendency towards faster functional recovery.6 Given these benefits, tension-free end-to-end anastomosis should be the preferred approach whenever possible, as it can significantly improve postoperative quality of life.
Preventing obturator nerve injury requires meticulous identification of the nerve throughout the lymphadenectomy field, particularly its proximal segment. In cases of transection, immediate intraoperative repair with tension-free end-to-end anastomosis is essential for optimal functional recovery. Laparoscopic nerve repair by gynecologic surgeons is both technically feasible and effective. Early recognition and prompt repair can minimize long-term neurological deficits, contributing to favorable patient outcomes.
None.
None.
The authors declare that they have no competing interests.

©2025 Kaido, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.