MOJ
eISSN: 2574-9935


Research Article Volume 8 Issue 2
1Head Department of Critical Care Medicine Hospital Angeles Metropolitano, Mexico
2Department Anestesiology (retired) Hospital de Ortopedia “Victorio de la Fuente Narvaez”, Instituto Mexicano del Seguro Social, Mexico
3Department of Critical Care Medicine Hospital General “Dr. Darío Fernández Fierro”, Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado, Department of Critical Care Medicine Hospital Angeles Metropolitano, retired, Mexico
Correspondence: Manzo Palacios Ervin, Head of Department Critical Care Medicine Hospital Angeles Metropolitano, Mexico City, Mexico Tlacotalpan 59, Roma Sur, Mexico City, ZIP code 06760
Received: June 22, 2025 | Published: July 10, 2025
Citation: Ervin MP, Miranda GGM, José DCL. The value of the prognostic scales acute physiology and chronic health evaluation APACHE II and Simplified Acute Physiology Score SAPS III, in the cost-benefit of patients admitted to the Intensive Care Unit. MOJ Sports Med. 2025;8(2):42‒45. DOI: 10.15406/mojsm.2025.08.00181
Background: The objective of intensive care units is to modify mortality caused by the onset of acute failure of one or more organ systems. However, in practice, diverse criteria are used, such as ethical and moral factors, bed availability, lack of intermediate monitoring areas, and various reasons that lead to high hospital costs. Disease severity indices such as the MPM (Mortality Probability Models) and APACHE (Acute Physiology and Chronic Health Evaluation) scores should be useful in the pre-admission stage and during the patient's stay in the ICU in order to rationalize therapeutic interventions. It must be acknowledged, however, that they are impractical when we are called upon to determine ICU admission.
Methods: All patients admitted to the Intensive Care Unit of the Angeles Metropolitano Hospital, of septic and non-septic origin, were studied. The APACHE II (Acute Physiology and Chronic Health Evaluation) scores and SAPS III (Simplified Acute Physiology Score) variables were determined. The determination is made through the intervals, which include APACHE> 30 points, APACHE: 20-30 points, and APACHE <30 points and concomitantly; the SAPS III was calculated for each group, the mortality percentage was determined and through the accounts department, the daily cost per department and segment assigned to the patients was obtained to define the unit cost. The APACHE II and SAPS III determination was performed upon admission and 48 hours later, data collection was done in a format specially designed for the study.
Results: A total of 48 patients were admitted during the study period, 47.91% were male. The mean age was 55.79 ± 18.5 years. APACHE scores were determined with intervals: + 30 points: 5 patients, 20-30 points: 11 patients, and -20 points: 32 patients. The number of deaths according to the APACHE intervals: > 30 points: 4 patients, 20-30: 5 patients, <20: 2 patients. The overall mortality was 22.91%. Days of stay for APACHE intervals:> 30: 2 ± 2.2 days/patient, 20-30: 10 ± 12.9 days/patient and <20: 5.70 ± 4.8 days/patient, costs according to APACHE upon admission: >30 points = Total = $41,911.92 USD (cost/day: $8,382.39 ± 10,829.11 USD), 20-30 points: $147,017.87 USD (cost day: $12,966.24 ± 9,629.25 USD), <20 points: $409,875.09 USD (cost/day $12,809.76 ± 11,120.14 USD). APACHE <20: SAPS III 47.5313 ± 11.21 points, mortality 20.0938 ± 14.074%. APACHE 20-30: SAPS III 61.66 ± 18.31 points, mortality 48.6333 ± 23.3274%. APACHE > 30: SAPS III 78.00 ± 15.18223 points, mortality 65.0 ± 20.78461%.
Conclusions: It is observed that the highest cost is in patients with an APACHE < 20 points, but with a greater number of days of stay and with a greater survival rate, and it is expected that the highest number of deaths can be observed with APACHE score levels > 30 points, as well as in the range of 20-30 points.
The primary objective of Intensive Care Units (ICUs) is to reduce mortality resulting from the onset of acute failure in one or more organ systems. However, in clinical practice, a variety of criteria are employed, including ethical and moral considerations, bed availability, the absence of intermediate monitoring areas, and other factors that contribute to elevated hospital costs. Severity of illness indices, such as the Mortality Probability Models (MPM) and the Acute Physiology and Chronic Health Evaluation (APACHE), should be useful during both the pre-admission phase and the patient's stay in the ICU, in order to rationalize therapeutic interventions. It must be acknowledged, however, that these tools are of limited practicality when clinicians are called upon to determine ICU admission.
Predictive models have become valuable tools in the care of critically ill patients, provided that their use is guided by clinical judgment and the experience of physicians. They serve as support for ethical and legal actions and are important elements to consider when withholding or initiating therapeutic measures. As with all decisions that impact patient care, the medical director must weigh the totality of available medical knowledge, the wishes of patients, families, and physicians, as well as the likelihood that intensive care will benefit the patient. Sometimes, these decisions will rely solely on medical judgment; at other times, the choice will reflect an ethical, legal, or philosophical perspective.
Objective
To report the value of the APACHE II (Acute Physiology and Chronic Health Evaluation II) scores and SAPS III (Simplified Acute Physiology Score) in the cost-benefit analysis of patients in a polyvalent Intensive Care Unit of a private general hospital.
Inclusion criteria
All patients admitted to the Intensive Care Unit of Hospital Angeles Metropolitano, both septic and non-septic, were studied. The variables measured included the APACHE II and SAPS III scores. Patients were stratified according to APACHE II intervals: >30 points, 20–30 points, and <20 points. For each group, the SAPS III score was also calculated, as well as the mortality percentage. The daily cost per department and segment assigned to each patient was obtained from the accounts department to determine the unit cost. APACHE II and SAPS III were determined at admission and at 48 hours. Data collection was performed using a form specifically designed for this study.
Patients and methods
Design: Cohort. Data Collection: Prospective. Setting: 7-bed ICU. Period: 6 months. Number Patients: 48. Sample: Convenience sample. Variables: APACHE, SAPS, length of stay, costs.
Statistics: Descriptive. Statistical software: SPSS® v.14.
Statistical analysis
Descriptive statistics were used. Statistical analysis was performed using SPSS® v.14. Given that the sample size was greater than 30, statistical analysis was conducted using a normal distribution and the one-tailed non-parametric Fisher test, with statistical significance set at p < 0.05 and one degree of freedom. Results were considered significant when the Fisher experimental value exceeded the critical Fisher value. For the analysis of predictive system intervals and considering that the number of patients in each interval could be less than 30, the Student’s t-test was used. The correlation between variables was determined with the Pearson correlation index.
A total of 48 patients were admitted during the study period, of whom 47.91% were male. The mean age was 55.79 ± 18.5 years. APACHE II scores were distributed as follows: >30 points: 5 patients; 20–30 points: 11 patients; <20 points: 32 patients. The number of deaths by APACHE II interval was: >30 points: 4 patients, 20–30 points: 5 patients, <20 points: 2 patients. The overall mortality rate was 22.91%. Length of stay by APACHE II interval was: >30 points: 2 ± 2.2 days/patient, p <0.05; 20–30 points: 10 ± 12.9 days/patient, p<0.05; <20 points: 5.70 ± 4.8 days/patient. Costs by APACHE II interval at admission were: >30 points: Total = $41,911.92 USD (cost/day: $8,382.39 ± 10,829.11 USD), 20–30 points: $147,017.87 USD (cost/day: $12,966.24 ± 9,629.25 USD), <20 points: $409,875.09 USD (cost/day: $12,809.76 ± 11,120.14 USD).
APACHE II <20: SAPS III 47.53 ± 11.21 points, mortality 20.09 ± 14.07%.
APACHE II 20–30: SAPS III 61.66 ± 18.31 points, mortality 48.63 ± 23.33%.
APACHE II >30: SAPS III 78.00 ± 15.18 points, mortality 65.00 ± 20.78%. The correlation of the variables is correlated between variables such as APACHE, SAPS III, Mortality, but is not correlated between the variables of the days of stay and fundamentally the mortality and the APACHE, SAPS III score, the total costs, the negative correlation is important in APACHE II < 20 points, SAPS III 20,093 points, considering that mortality is lower but total costs are high, there being little difference with respect to daily costs, and the explanation is that the days of stay are higher in this group, APACHE II < 20 points, SAPS III 47.53 points (Table 1) (Graphs 1-3).
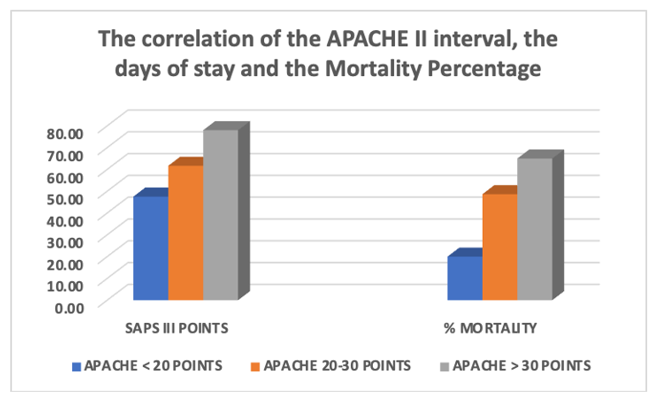
Graph 2 The correlation of the APACHE interval, the days of stay and the Mortality Percentage, observing that in patients with APACHE > 30 points, the number of days of stay was lower, also presenting a high mortality percentage, the highest number of days of stay is observed with APACHE between 20-30 points and those with less than 20 points.
|
Apache |
Total costs* |
Day costs* |
Saps iii |
Mortality |
Days of stay |
|
>30 POINTS |
$ 41,911.92 USD, |
$8,382.39 ± 10,829.11 USD |
78.00 ± 15.18223 points, |
65.0 ± 20.78461 % |
2.0±2.2 days/patients, |
|
r = -.504 p< 0.05 |
r = -.504 p < 0.05 |
r = -.330 < 0.05 |
r = -.330 p< 0.05. |
r =-.330 p< 0.05 |
|
|
20-30 POINTS |
$ 147,017.87 USD, |
$12,966.24 ± 9,629.25 USD, |
61.66 ± 18.31 points, |
48.6333 ± 23.3274 %, |
10 ± 12.9 days/patients, |
|
r =.416 p <0.05 |
r = .461 p < 0.05 |
r = 0.655 p< 0.01 |
r = .938 p <0.01 |
r = 1.000 p< 0.01 |
|
|
< 20 POINTS |
$409,875.09 USD |
$12,809.76±11,120.14 USD, |
47.5313±11.21 points, |
20.0938±14.074 %. |
5.70±4.8 days/patients, |
|
r = -.330 p < 0.05 |
r = -.330 p < 0.05 |
r = .422 p< 0.01 |
r = -.330 p< 0.05. |
r = .938 p<0.01 |
Table 1 Shows the summary of the variables analyzed and their interrelations
*Estimated Costs.
In many departments, the number of beds in intensive care units (ICUs) for critically ill patients is limited, and patients arriving with varying degrees of morbidity are frequently compared to determine which ones can best be treated in these wards. All predictive scales used in intensive care are nothing more than systems of numerical values to describe the possible evolution of a patient's illness. The first model to survive criticism and see the light of medical publication was the one proposed by William Knaus in 1981; this consisted of a set of models generically called Acute Physiology and Chronic Health Evaluation, known by the acronym APACHE, and has been designed and updated by Knaus and others since the late 1970s.
The first studies designed to validate predictive models began in the 1980s. Lemeshow and Hosmer published several studies on the most commonly used models at that time, and found that they had similar calibration and discrimination performance. In 1990, Schafer et al.1 compared the predictive capacity of the APACHE II model with the initial versions of the Simplified Acute Physiology Score (SAPS I) and the Mortality Probability Models (MPM) on admission and obtained results similar to those of Lemeshow1-5 years earlier. In the present study, the APACHE II model was chosen because of its demonstrated predictive power and thus obtained validation despite the sample size, which turned out to be small compared to other studies.
Regarding the precedent found in the literature regarding the use of the APACHE II predictive index as a dynamic score, Biot1et al.6–8 in 1988, demonstrated in 128 patients that the longitudinal use of a variant of the APACHE II, the Sickness Scoring System, was the best predictor of outcome. Also in that year, Shuster et al.1 proposed the use of the APACHE II corrected for the number of organs or systems in failure for individual patient prognosis. Subsequently, in 1994, Douglas Wager et al.9 members of the same APACHE II team, sequentially used this model and suggested that its use beyond 24 hours could provide a refinement of its mortality predictions. From previous studies10–13 it is known that using a 50% cutoff point, virtually all proposed predictive models will have at least a 10% to 15% false classification rate. This has been interpreted by some authors5–8 as meaning that all predictive systems are approximately equivalent and none is good enough for individual prediction. This eminently mathematical statement, although it holds true, at least in theory, it cannot be viewed absolutely, as the individual prediction criterion of a model is based on the refinement it achieves in its longitudinal evolution, the size of the sample used, and the ability of the variables to adjust to the environment in which it is developed.
Other authors share our criteria. Knaus et al.14 in 1986, based on a sample of 210 patients, correctly classified 84.3% of patients with APACHE II with a specificity of 95.5%, also considering a cutoff point of 50%. In another study, Castella et al.15 in 1995, correctly classified 68.3% of 593 polyvalent patients with APACHE II with a specificity of 74.9% at the same cutoff point. Finally, Wagner et al.9 in 1994, correctly classified 83.4% of 332 patients with APACHE II, with a specificity of 95.4%.16–20
The greatest impact of the Cost benefit can be observed with an APACHE II (Acute Physiology and Chronic Health Evaluation II) scores, less than 20 points, SAPS III (Simplified Acute Physiology) Score 47.53 points, the cost is higher, but with high days of stay, but mortality is the lowest, considering that costs rise at the expense of the days of hospitalization increased, so a paradigm that can be created is that the Intensive Care Units, the admission criteria must change given the possibility that their function must be more preventive than curative, and that the APACHE II score of 20-30 points or greater than 30 points, with SAPS of 61.6 and 78.0 points leads to high mortality. Despite the sample size, it should be taken into account for future studies.
None.
There are no conflicts of interest or sources of support.

©2025 Ervin, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.