MOJ
eISSN: 2574-9935


Research Article Volume 7 Issue 2
1Medical student, University of Ribeirão Preto, Brazil
10Medical Student, Nove de Julho University, Brazil
11Physiotherapist, Nove de Julho University, Brazil
12Physiotherapist, Universidade Paulista UNIP, Brazil
13Physiotherapist Master in Rehabilitation, Nove de Julho University, Brazil
14Bachelor of Medicine, Faculty of Medical Sciences of Paraíba- FCM/PB, Brazil
15Master in Health Sciences, Federal University of São Paulo- UNIFESP, Brazil
16Doctor in Medical Sciences, Ribeirão Preto Medical School, Brazil
2Medical student, Nove de Julho University, Brazil
3Medical student, Universidade Municipal de São Caetano does Sul (USCS), Brazil
4Medical student, Potiguar University UNP, Brazil
5Medical student, UCP- Central University of Paraguay, Paraguay
6Medical student, University of Southern Santa Catarina, Brazil
7Medical student, University of Rio Verde, Aparecida de Goiânia, Brazil
8Medical student, University of Rio Verde, Formosa, Brazil
9Bachelor of Medicine, Severino Sombra University, Brazil
Correspondence: Thiago Augusto Rochetti Bezerra, University of Ribeirão Preto, University of São Paulo, Ribeirão Preto Medical School, Brazil
Received: April 20, 2024 | Published: May 2, 2024
Citation: Bezerra TAR, Malaquias DT, Vivas AD, et al. Cardiological emergency and acute myocardial infarction: physician and physiotherapist perceptions of immediate care, use of prehospital ECGS and patient referrals. MOJ Sports Med. 2024;7(2):49-57. DOI: 10.15406/mojsm.2024.07.00162
Doctors and physiotherapists play a key role in reducing the rate of morbidity and mortality from acute myocardial infarction through well-applied care, as well as through the key point of health education, given that most of the risk factors are modifiable. This article is a literature review, which aims to explore the challenges faced by patients with acute myocardial infarction. This review shows that heart attacks are a serious problem. The study proves that this damage can be reduced or minimized with the training of medical and physiotherapy professionals in recognizing the signs and symptoms in good time, as well as the best treatment.
Keywords: myocardial infarction, rate of morbidity and mortality from acute myocardial infarction, heart attacks
Despite major improvements in the treatment of acute coronary syndrome (ACS), there is still a high risk of mortality.1 Delays in care should be kept as short as possible to reduce complications and mortality.
Large amounts of research are carried out every year with the aim of investigating how to speed up the care of patients with ACS.1
However, a substantial number of ACS patients are still not treated within the preferred timeframe of urgent and emergency care protocols.2
Pre-hospital delays are usually the longest in the chain of ACS events and it is therefore in this section that the greatest benefits in terms of time can be obtained.3
Pre-hospital delays include patient, physician and emergency medical transport (EMT) delays.4 There are several ways for a patient with suspected ACS symptoms to ask for help and be referred to the hospital. In most countries, patients with chest pain contact their primary care physician, general practitioner or go directly to the hospital.5
The family doctor may decide to refer the patient to hospital, carry out further diagnostics and treatment, or reassure the patient without referring them. In order to reduce delays in ACS patients, the European Society of Cardiology (ESC), as well as the guidelines of the American College of Cardiology Foundation and the American Heart Association (ACCF/AHA), advises against using family doctors.4,6
General practitioners have been advised to refer all patients with new or recently changed chest complaints to hospital without further delay in order to avoid missing any myocardial infarction.7
In a society that is less tolerant of missing a diagnosis, with an increasing number of lawsuits for failing to diagnose a serious illness in advance, general practitioners prefer prevention to cure.8
This low threshold for pre-hospital care has a disadvantage: up to 80% of patients are unnecessarily referred to hospital,9 which leads to crowded emergency departments and additional stress for patients.10
The key to ensuring treatment without overloading medical services with non-cardiac patients is triage.10 Over the last decade, the rate of acute non-systemic myocardial infarction has increased and exceeded the incidence of acute ST-segment elevation myocardial infarction.11
Furthermore, patients with ST-segment elevation acute myocardial infarction (STEMI) and non-ST-segment elevation acute myocardial infarction (NSTEMI) differ in terms of mortality. Patients with STEMI have higher short-term mortality rates,12 while patients with STEMI have higher long-term mortality.12,13
This has resulted in a different approach and advice regarding delays. More recent studies indicate that the Pathophysiology between patients with STEMI and STEMI is not as different as previously assumed.11
Apart from similar symptoms and essentially the same physical examination, ECGs don't always differentiate between occluded and open vessels. The left circumflex artery, for example, is notorious for showing minimal ST deviations on the ECG, even when occluded. Furthermore, occluded arteries or transmural ischemia are not exclusive to patients with STEMI.11 This knowledge has led to an adjustment in the advice on delays.
Delayed reperfusion in patients with STEMI increases mortality.14 Early reperfusion results in superior clinical outcomes, better recovery of left ventricular ejection fraction, less heart failure and fewer re-occlusions.15
The maximum delays recommended in the guidelines for patients with STEMI are rarely achieved. A system delay of 90 minutes or less is achieved in 80% of cases.13
The average system delay in European countries varies between 60 and 177 minutes, with a global average of 110 minutes before the patient can be seen.10
To carry out a descriptive review study on Cardiological Emergency and Acute Myocardial Infarction: Physician's perception of immediate care and referral of patients to the Intensive Care Unit.
This literature review will outline pre-hospital delays and the triage of patients with chest pain. We will discuss the Pathophysiology, delays in patients with ST-segment elevation and non-ST-segment elevation myocardial infarction, the incidence of chest pain, patient delays, family doctor or physician delays, triage (by ER doctors) and delays.
A descriptive review study was carried out on the medical management of emergency care for patients with heart attacks.
The studies were analyzed from February to April 2024, with a sample of 38 scientific articles. The study required a more in-depth review of the specific literature on the importance of cardiac emergencies and acute myocardial infarction and the doctor's perception of immediate care and referral of the patient to the intensive care unit.
Study participants
Medical undergraduates from various periods took part in the study.
Pain is a universally known phenomenon and is associated with various pathologies that afflict society in general, regardless of race, color, age and social class, and is the main cause of human suffering, compromising quality of life.16
In this context, it is important to conceptualize pain and understand its causes, origins, complications and diagnoses, supporting each individual and their symptoms according to the clientele who seek health services in large and small hospitals, whether public or private. Pain is a warning sign to avoid injury.16
The pain assessment process includes the patient's history and physical examination, as well as the related psychosocial and family aspects. It is also important to involve the sensory components of pain; the pattern, location, intensity and nature should be assessed, and due to the subjectivity of the symptom, self-reporting is of paramount importance in this assessment process. Thus, pain relief is a prerequisite for the patient to achieve optimal recovery and quality of life.17
In order to measure pain, there are scales that guide professionals in their diagnosis and choice of therapy, which are the scales- Unidimensional and Multidimensional which are instruments that favor assertiveness in the choice of diagnosis and treatment. One-dimensional scales are used to quantify the intensity of pain, while multidimensional instruments are used to identify the different spectrums of pain. One-dimensional scales are more commonly used in hospitals, as they are easier to use to identify pain in patients.16
The one-dimensional scale has a great advantage because it is easy to apply and is known as the Visual Analog Scale (VAS) (Figure 1), which consists of a numerical scale ranging from 0 to 10, where 0 means no pain and 10 means maximum pain according to the patient.18,19
Pain assessment will always be necessary to help diagnose and treat the patient, as it aims to promote well-being and qualify the treatment. This assessment process is important for the patient to have an adequate recovery of their health, as pain relief will be the basis of their treatment.19
One of the most frequent symptoms in the emergency room is related to chest pain. This pain is manifested by a feeling of discomfort in the chest area, which can be felt in different ways and of different intensity, such as: dizziness, dyspnea, weakness, epigastric pain, syncope and palpitation. All these causes make the body feel unwell.16
Faced with the clinical picture in which chest pain manifests itself, it is of the utmost importance to make an assertive diagnosis based on the characteristics of the pain, its location and identifying the risk factors that are associated with the patient.19
There are countless challenges in relation to public health problems that involve the population as a whole. It is important to emphasize that pain is one of the identifying signs for collecting data and directing care.20
Chest pain is the manifestation resulting from coronary artery disease (CAD) or any condition that causes myocardial ischemia through an imbalance between myocardial oxygen demand and myocardial oxygen supply.21
In order to make an accurate diagnosis, the most common tests performed are ergometric tests, echocardiography with physical or pharmacological stress, and other complementary exams needed to identify complications. All these tests must be carried out with the utmost urgency, but with responsibility and professional ethics. Doctors working in the classification need to have scientific, practical and technical knowledge, as well as knowing the signs of ACS and the situations that pose risks to patients, making quick decisions.21
Figure 2 shows a detailed diagram of chest pain, which has two origins, cardiac and non-cardiac. This explanation is fundamental for guiding patients and choosing the appropriate treatment according to the signs and symptoms.
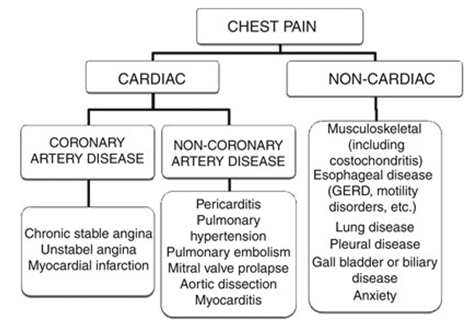
Figure 2 Cardiac and non-cardiac diseases that manifest with pain.
Source: Bassan R, et al. A Sociedade Brasileira de Cardiologia. I Guideline on chest pain in the emergency room. Arq Bras Cardiol. 2002; 76(supl II).
In cases of ACS, it is not possible to define the diagnosis by physical examination alone, since this test alone does not offer full assertiveness, and can be confused with other pathologies. However, during the physical examination, there may be changes in the 4th heart sound, or a reduction in the pulse in the lower limbs, among other factors, and it is possible to recognize indicators that favor confirmation of the diagnosis of chest pain.16
This distinction between signs and symptoms that can be confused with cardiac and non-cardiac diseases is essential for the doctor's care in the classification, since his assessment will define the waiting time and start of treatment for the patient.19
Thinking about how to care for patients with chest pain is a challenge. Due to the high risk of mortality from cardiovascular diseases, doctors must prioritize the care of these patients, which is why the use of institutional protocols is essential to speed up diagnosis.17
The use of institutional protocols aims to help with coherent and assertive identification, since the challenge of implementing the chest pain protocol is great, due to the way in which patients report their pain, which is considered to be the 5th vital sign. Pain must be taken into account along with the clinical signs that the patient may present, and in this impasse, the professional cannot anticipate or make judgments that harm the patient; all complaints must be taken into account.18
Reaffirming this need to properly classify chest pain as a "report of chest pain, which may radiate to the left arm" with these characteristics, the doctor should classify this patient with the color orange, which, according to the Manchester protocol, recommends that medical care should be provided within 10 minutes of identifying the sign.19
For the doctor to work in emergency/urgent care requires training and a great deal of skill, as well as understanding, knowledge, respect and responsibility in the objective interpretation by the professional who, in the risk classification, will analyze the complaint presented by the user in a holistic way, in order to solve it with the least possible aggravation, making quick decisions.16
A patient complaining of chest pain can lead to a diagnosis of ACS, which must be attended to quickly, since the speed between classification and specialized care is essential for diagnosing, treating and recovering this patient. The action must always be guided by technical and scientific knowledge, using the institutional protocol, where the waiting time for this patient's care to begin is 10 minutes, and performing an electrocardiogram (ECG) is essential at this stage, so that the patient can begin the appropriate therapy for their diagnosis.18
In order to facilitate the process of classifying patients, an institutional protocol was implemented, which originated from the Manchester protocol (Figure 3) that emerged at the Manchester Royal Infirmary in England in 1994, when a group of doctors and nurses met to discuss solutions to the disorganization of the service system in the United Kingdom, which is why it was named the Manchester protocol, developed by a team coordinated by Professor Kevin Mackway-Jones.21
As a result, a consensus was established between nurses and doctors in the emergency department to provide standardized care. This system began to be implemented in several countries at the end of the 1990s (Graph 1). In Brazil, it was used for the first time in 2007 (Figure 3), with the aim of organizing the flow of patients, and on this occasion the person responsible for disseminating the protocol in Brazil emerged.8,19,20
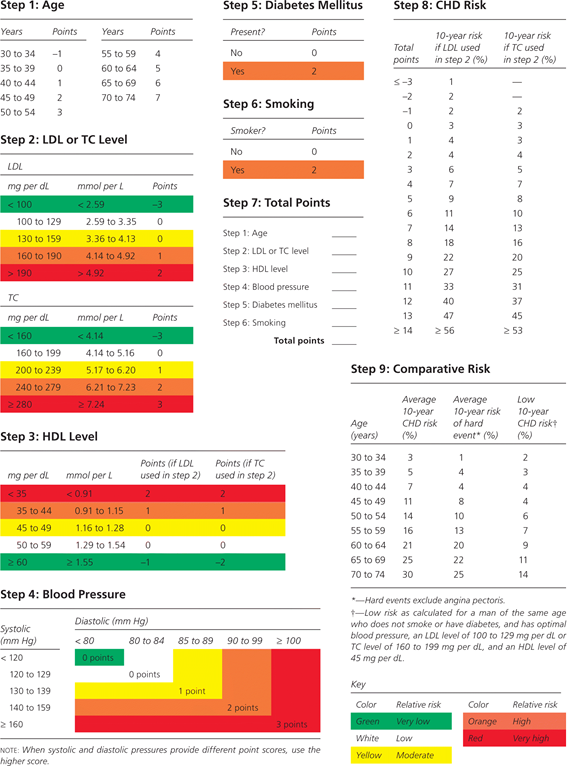
Graph 1 Estimated risk of coronary heart disease (CHD) in men (HDL = high-density lipoprotein; LDL = low-density lipoprotein; TC = total cholesterol)
Source: Adapted with permission from Wilson PW, D'Agostino RB, Levy D, et al. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–1847..
The overall risk of CHD is the absolute risk of a coronary heart disease-related event during a specific period, usually 10 years. The event can be "hard" (e.g. myocardial infarction [MI], sudden cardiac death) or "soft" (e.g. chest pain).
The risk estimate is based on major risk factors and is calculated using an empirical equation (Figure 3). In contrast, the conventional clinical approach to the primary prevention of cardiovascular disease relies on identifying and treating individual risk factors, such as hypertension and hyperlipidemia.
The system classifies patients by color, after an evaluation based on symptoms, each color represents the degree of severity and the waiting time for medical care for each patient, the system is divided into 5 colors: red, orange, yellow, green and blue, each color has its waiting time based on the degree of priority of this patient, the red color being an emergency case where care must be immediate; the orange color refers to the cases of very urgent patients who have up to 10 minutes for care; already yellow signaled urgent cases that can take 60 minutes for care; patients classified with green have little urgency and can be attended in up to 120 minutes and, the blue color which is for non-urgent cases that can take 240 minutes to be attended, as presented (Figure 4).
Each hospital is based on a system and processes according to its needs and preferences for patient care. The hospital analyzed in this research uses the institutional chest pain protocol during the care of patients with chest pain, which aims to systematize care and reduce the risk of possible complications, promoting agility and priority for patients with chest pain, since its approach becomes a challenge due to the wide variety of related diagnoses, which can vary from low to high risk of morbidity and mortality.10
During classification, the doctor needs to prioritize care, since the protocol is open to all patients admitted to the emergency department with complaints of chest pain. Once the protocol has been opened, the patient undergoes an ECG test, which is considered to be of the utmost importance in this initial care, which should be carried out within the first 10 minutes of opening the patient's chart, in order to reduce the time between arrival and the start of the necessary treatment for the patient.17
The main purpose of the chest pain protocol is to classify which patients should have priority for immediate care, based on their clinical priority, so that patients in extremely serious condition have priority for specialized care (Figure 4).18–20
The institutional protocol begins with an ECG test, which should be carried out within the first 10 minutes. After the test, the cardiologist will evaluate the ECG and report it. Once the protocol has been opened, the patient will receive a dose of ASA and will undergo laboratory tests to assess CK-MB, MASS and troponin. According to the I Guidelines of the Brazilian Society of Cardiology, CK-MB and/or troponin are the biochemical markers of choice for the definitive diagnosis of myocardial necrosis in this patients.19,21,22
Acute coronary syndrome (ACS) is a general term for conditions caused by a sudden blockage of the blood supply to the heart. A range is established from a potentially reversible phase of unstable angina (UA) to irreversible cell death from myocardial infarction (MI) - either a non-ST-segment elevation myocardial infarction (NSTEMI) or an ST-segment elevation myocardial infarction (STEMI) (Figure 5).19
Pre-hospital ECGs
A survey revealed that 90% of the systems serving the 200 largest cities in the United States had 12-lead ECG equipment in their ambulance systems.16
Providers can quickly obtain diagnostic-quality pre-hospital ECGs, with an average increase of 5 to 6 minutes in on-site time.18,19
To obtain diagnostic-quality pre-hospital ECGs, a valuable strategy is to educate providers about the importance of careful patient positioning and electrode placement. Motion artifacts, incorrect electrode placement and poor skin contact can result in poor quality tracings that can be misinterpreted by algorithms.18,19
One study, which used data from the National Myocardial Infarction Registry between 2018 and 2021, concluded that patients with a pre-hospital ECG had 20-minute longer time intervals from symptom onset to hospital arrival.10,12
However, this conclusion was difficult to interpret, since there was no measure of the duration of the pre-hospital ECG and a potential selection bias in who received a pre-hospital ECG. For example, patients who had a longer transport distance may have received a higher rate of pre-hospital ECGs compared to those with a shorter transport distance.
Several studies have examined the feasibility of Emergency Aid providers identifying IAMCSST using pre-hospital ECGs with or without wireless transmission.18,20
The pros and cons of computer algorithm interpretation, paramedic interpretation and wireless transmission for medical interpretation of pre-hospital ECGs. There is no data comparing the effectiveness of these different approaches in terms of diagnostic accuracy or the quality of reperfusion therapy administered to patients with STEMI. The choice of which option to use may also be limited by the specific resources available in the community or its local geography.23
Studies have also shown that paramedics with specific ECG training can reliably interpret pre-hospital ECGs without passing them on to a hospital or doctor.24
Trained paramedics can identify STEMI with sensitivity ranging from 71% to 97% and specificity ranging from 91% to 100%, and with good agreement between paramedics and emergency department doctors (κ ranging from 0.59 to 0.73).25
The sensitivity (97%) and specificity (91%) of paramedics trained to interpret pre-hospital ECGs and diagnose STEMI was particularly high in one study, which included a 2-day training seminar.8
A study on this issue, carried out in the United States with 151 transported patients with suspected acute myocardial infarction, concluded that trained paramedics had a sensitivity of 80% and a specificity of 97% in diagnosing STEMI with pre-hospital ECGs, with good agreement between paramedics and emergency physicians (κ=0.73).5
Alternatively, pre-hospital ECGs can be transmitted by the doctor for interpretation to guide decision-making, but this approach has been limited by the technological requirements for fast and reliable transmission of pre-hospital ECGs.23
Two pilot studies have shown that wireless transmission of pre-hospital ECGs is reliable. In the Timely Intervention in Myocardial Emergency-Northeast Experience (TIME-NE) carried out in Concord (USA), 24 STEMI patients had a successful wireless transmission of pre-hospital ECGs to a hospital reception station and to the smartphone of the cardiologist on duty. The on-call cardiologist then decided whether to activate the cath lab based on the pre-hospital ECG.2
The median door-to-balloon time decreased in this study to 50 minutes, compared to 101 minutes for historical controls; however, there were 19 STEMI patients who experienced wireless transmission failures. In the ST-Segment Analysis Using Wireless Technology in Acute Myocardial Infarction (STAT-MI) study, carried out in Newark (USA), 80 patients underwent pre-hospital ECGs transmitted via a wireless cell phone network to a secure central server in the hospital and to the smartphone of the cardiologist on duty.25
This model had no transmission failures; the average time from pre-hospital ECG acquisition to availability on the remote server was 2 minutes and on the smartphone was 4 minutes. The door-to-balloon time was 80 minutes with the use of pre-hospital ECGs, compared to 146 minutes for historical controls without the use of pre-hospital ECGs.26
In geographical regions with poor wireless network coverage, the transmission of pre-hospital ECGs for medical interpretation may fail to transmit or experience significant delays in up to 20% to 44% of cases, and as a result of wireless "dead zones" in a moving ambulance or in rural areas with poor coverage.4
These systems acquire the pre-hospital ECG and automatically transmit the data via the Bluetooth protocol to a nearby cell phone. The cell phone acts as a router to transmit the data to a central receiving station and to Smartphones via a wireless cellular network or a wireless local area network.7
A cell phone with a camera takes a digital image of the paper printout of the pre-hospital ECG and transmits it to an email account, and the ECG image can be viewed on any device compatible with multimedia messaging, such as a computer or a smartphone. This approach could be a simple, low-cost and innovative technology for communicating diagnostic imaging data and deserves further study as to its feasibility in real-world practices.9
Hospitals must organize efficient systems of care for patients with STEMI, from the pre-hospital phase of care to hospital arrival and reperfusion therapy in the hospital phase of care.24
The current typical process for emergency cardiac care initiated by a 9-1-1 call is contrasted with the far from ideal process in most cities around the world.27
Historically, emergency medical service providers have been trained to follow the following steps in assessing patients with chest pain: (1) assess the airway, breathing, circulation and vital signs; (2) obtain a focused history and examination; (3) assess the heart rhythm; (4) initiate treatment with oxygen, aspirin, nitroglycerin and morphine and insert an intravenous line; (5) recommended: acquire a pre-hospital 12-lead ECG at the scene, after the patient is transferred to the ambulance or while en route to the hospital. Since the 12-lead ECG represents critical data for diagnosis and decision-making in chest patients (Figure 6).5
Information from a pre-hospital ECG and advanced notification should lead to efficient action on the part of hospital care systems to provide immediate reperfusion therapy, including preparing to receive and assess the patient, activating the cath lab while the patient is en route, or bypassing the emergency department and transporting the patient directly to the cath lab.28
If patients are assessed in the emergency department, the assessment should be simplified by having a doctor and the necessary resources (e.g. translators, nurses) ready before the patient arrives, following a standard protocol for treatment and minimizing physical movement, such as transferring between stretchers.22
Although avoiding the emergency department may be intuitively faster, concerns have been raised about the processes of obtaining informed consent, patient safety and consideration of alternative diagnoses (e.g. aortic dissection, intracranial hemorrhage) or other false positives that can explain ST-segment elevation on the ECG in up to 10% to 15% of patients.21
In addition, during off hours, the catheterization team may not have arrived at the hospital before the ambulance, and the patient will have to be observed in an intensive care environment until the catheterization laboratory is ready to receive the patient.20
Patients with STEMI who require inter-hospital transfer experience substantial delays, with an average door-to-balloon time from the first hospital of 180 minutes.23
In the United States, regional hospital networks and systems of care have been implemented and evaluated to improve reperfusion therapy time for patients presenting initially to a community hospital without on-site PCI capability.19
Similar but broader systems for optimizing reperfusion therapy across populations have also been in place in Europe for several years.6
European systems generally have a doctor in the ambulance, a central dispatch center for ambulances and highly organized regional pre-hospital care, which contrasts with the disorganized and competitive environment in the United States.22
Pre-hospital ECGs can play an important role in triaging patients in a regional network of hospitals, and the two models proposed include pre-hospital triage versus inter-hospital transfer.21
The pre-hospital triage model transports patients with STEMI to the nearest PCI center and avoids hospitals without PCI capacity. The inter-hospital transfer model focuses on advanced notification and efficient transfer of patients from non-PCI hospitals to PCI centers.29
Several key factors, including distance, urban or rural location, collaborative or competitive relationships between hospitals, and variability of EMS providers, influence which model is best suited to specific regional populations.
An analysis of the U.S. Census Survey and the American Hospital Association Annual Survey showed that 80% of the adult population lives within 60 minutes of a PCI-capable hospital and only 5% live more than 90 minutes from a hospital.2
However, there are still 20% of the adult population and large geographical areas that do not meet this standard. One model of regionalized care does not exclude the other. Both can coexist in a single network and are often driven by specific resources available in a community and local geography.30
There is no data comparing the models, and possible unintended consequences, such as unusually long delays to reperfusion, should be monitored.31
Boston's EMS program, one of the first in the US, involves municipal paramedics trained to interpret and classify pre-hospital ECGs as definite STEMI, possible STEMI or non-diagnostic.
Patients with definite STEMI or possible STEMI are triaged to the nearest PCI hospital, with the former being taken directly to the cath lab and the latter being evaluated in the emergency department.
For the most part, current measures for assessing the use and timeliness of reperfusion therapy in STEMI (e.g. door-to-balloon time) are hospital-based and therefore inadequate for assessing the effectiveness of pre-hospital ECGs. To assess the incremental benefit of this technology, current hospital-based measures (door-to-balloon time) would have to evolve into patient-centered measures, such as first medical contact until reperfusion or onset of symptoms until reperfusion.29
The current STEMI guidelines recommend that the relevant metric for the quality of reperfusion therapy should be first medical contact to balloon <90 minutes and first medical contact to drug <30 minutes. In addition, it is necessary to assess patient responsiveness after symptom onset, appropriate utilization and responsiveness, scene time to obtain pre-hospital ECGs, and effective communication of this data to destination hospitals and its use in reperfusion therapy decision-making.29
It is necessary to carry out a careful analysis of the denominator or eligible population that should have received a pre-hospital ECG compared to those who actually received a pre-hospital ECG. For service providers to adopt the technology, a better understanding of how the potential gains in terms of rapid reperfusion translate into better clinical outcomes would be ideal, as well as an understanding of the frequency of false alarms and other unintended consequences.23
Real-world examples are particularly useful in this regard, given the comprehensive approaches that different types of healthcare systems - for example, urban or rural - may require. These examples would also be important for assessing the overall value of this technology in relation to the financial investment in equipment, training.
The American Heart Association's national guidelines, as well as other consensus and scientific statements, recommend that emergency medical services (EMS) acquire and use pre-hospital ECGs to evaluate patients with suspected acute coronary syndrome.22
Despite these recommendations, pre-hospital ECGs are used in less than 10% of patients with ST-segment elevation myocardial infarction (STEMI) and this rate has not changed substantially since mid-2020.32
Furthermore, even when a pre-hospital ECG is acquired, the information is often not effectively translated into action and coordinated with hospital care systems to reduce delays in reperfusion therapy.30
Role of the physiotherapist in AMI
Physiotherapy in phase I of cardiovascular rehabilitation (CVRT) can be started 12 to 24 hours after acute myocardial infarction (AMI), however, prolonged bed rest is common due to the fear of in stabilizing the patient.33
The infracted patient chosen for cardiac rehabilitation goes through several phases, which are divided into 3 or 4 phases, depending on the author: Phase I corresponds to the period of the patient's stay in hospital (in-hospital phase), beginning with the patient's admission. Phase II corresponds to the period after hospitalization, immediately after discharge, and can take place on an outpatient basis or at home. Phase III does not have a defined duration, it is the phase following phase II, aimed at supervised, long-term maintenance of the patient's condition, taking place on an outpatient basis or in the community. Phase IV, as described by some authors, denotes a long-term maintenance program that does not necessarily need to be supervised, and can take the form of regular sports or physical exercise.34
Phase III begins, on average, between the 6th and 12th weeks or more after a coronary event such as AMI. The patient doesn't necessarily have to have gone through the previous phases, and they must be clinically stable; this phase provides continuity in increasing physical capacity and well-being.35
The main objective in phase III is to improve physical fitness, but the need to promote well-being (improved quality of life) should also be considered. This phase will provide a higher level of physical, mental and social function, and the treatment emphasizes distance goals rather than speed, with moderate effort intensities, so that the patient can obtain all the benefits of the program without running unnecessary risks.36
Physical exercise is characterized by a situation that removes the body from its homeostasis, as it implies an instantaneous increase in the energy demand of the exercised muscles and, consequently, of the body as a whole. Physical exercise can be divided into two basic categories: dynamic or aerobic exercise and static or resistance exercise.37
Among the physiological effects promoted by aerobic exercise that benefit cardiovascular rehabilitation patients are: increased venous return and stroke volume; optimization of myocardial contractility; reduction in myocardial demand for oxygen at submaximal levels of exercise; optimization of oxygen extraction (arteriovenous oxygen difference); improved utilization of oxygen to generate more work (mechanical efficiency); increased perfusion and coronary collateral circulation; regression of atherosclerotic plaques; improved exercise limitation due to endothelial dysfunction; improved muscle oxidative capacity (increased number of oxidative enzymes); improved muscle perfusion; higher VO2 Max values (maximum O2 consumption); higher work rates obtained without ischemia; reduced heart rate; reduced blood lactate; lower blood pressure levels; improved lipid profile (lower LDL) (low density lipoprotein); lower resting systolic blood pressure; increased glucose tolerance; lower triglycerides; reduced anxiety and depression; lower peripheral vascular resistance (prolonged peripheral vasodilation).38
Pre-hospital ECG programs have the potential to improve the way care is provided to STEMI patients worldwide. Current American Heart Association guidelines recommend that paramedics perform and evaluate a routine pre-hospital ECG in patients with chest pain with suspected STEMI (Class IIa, Level of Evidence B).
The main challenge for healthcare providers is not simply to perform a pre-hospital ECG, but to use and integrate the diagnostic information from a pre-hospital ECG into care systems.
The potential reductions in time from first medical contact to reperfusion therapy through the integration of pre-hospital ECGs with hospital care systems are considerable and clinically relevant. However, the gaps between use in ideal circumstances and routine practice remain substantial.
There are many logistical barriers, including the need to increase patient use of EMS; increase EMS capacity; improve training and quality assurance of EMS providers; improve collaboration between EMS, emergency departments and cardiology; improve the organization of hospital systems and providers; and improve coordination of regional hospital networks to provide optimal patient care, rather than optimizing market share.
It is also clear that several financial barriers, including reimbursement and the cost-effectiveness of this diagnostic technology, will have to be overcome for pre-hospital ECGs to gain widespread support from payers, providers and healthcare systems. But these barriers are not insurmountable and can be overcome with dedicated efforts to improve care systems. Future research and policy measures are needed to encourage emergency medical services, hospitals and healthcare systems to adopt and maximize the full potential of this technology, as well as to monitor unintended consequences.
None.
The author declares that there are no conflicts of interest.

©2024 Bezerra, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.