MOJ
eISSN: 2379-6383


Review Article Special Issue II Primary care services
1Federal University of Maranhão, Medicine Course, Pinheiro, Maranhão, Brazil
2Medicine, IESVAP- Instituto de Educação Superior do Vale do Parnaíba, Brazil
3Medicine, Centro Universitár io FACID Wyden, Brazil
4Medicine, State University of Maranhão, Brazil
5Federal University of Maranhão, Dentistry, Brazil
Correspondence: Consuelo Penha Castro Marques, Universidade Federal do Maranhão, Brasil, Tel (98) 99100-7752
Received: March 15, 2025 | Published: March 28, 2025
Citation: Almeida GT, Silva LF, Leite BCC, et al. Organ, tissue and cell transplants in the context of primary health care in Brazil: systematic review. MOJ Public Health. 2025;14(1):67-72. DOI: 10.15406/mojph.2025.14.00473
Introduction: This study analyzes the epidemiology of organ, tissue, and cell transplants in primary health care (PHC) in Brazil, considering the period between 2015 and 2025. Although the country has one of the largest public transplant programs in the world, challenges persist, such as family refusal, misinformation, and gaps in infrastructure, which can affect the effectiveness of actions and the quality of patient care.
Methodology: A Systematic literature review was carried out, following the PRISMA protocol, in national and international databases (PubMed, Virtual Health Library, and Google Scholar). Original articles and literature reviews published in Portuguese and English, from 2015 to 2024 that addressed the topic of organ, tissue, or cell transplants related to PHC in Brazil were selected. After applying inclusion and exclusion criteria, 13 studies with a final sample were presented.
Results: The studies analyzed converged on three major themes: (1) psychological and social aspects of organ donation and transplantation, with an emphasis on emotional support and multidisciplinary work; (2) education and knowledge about organ donation, highlighting the importance of ongoing training for community agents, general practitioners, and primary care users; and (3) factors related to family refusal, highlighting the influence of cultural, emotional, and infrastructure barriers on the decision to donate. It was found that PHC can play a fundamental role in identifying potential donors, in pre- and post-transplant monitoring, and in raising awareness among families and patients.
Conclusion: It is concluded that the effectiveness of transplants in Brazil is not limited to high complexity, but involves structured actions in primary health care, capable of reducing family refusal, promoting ongoing education, and expanding access to information. The consolidation of public policies and the strengthening of PHC, through awareness campaigns and multidisciplinary support, are essential to improve epidemiological indicators and the quality of care in the process of organ, tissue and cell donation and transplantation in Brazil.
Keywords: organ transplants, tissue transplants, cell transplants, primary health care
Organ, tissue and cell transplantation consists of the transfer of biological structures from a donor to a recipient, with the aim of restoring or improving the function of a compromised organ or tissue.1 In this sense, this procedure can involve different parts of the body, and is characterized by being a fundamental therapeutic resource for several chronic and acute diseases, which begins at an essential stage of primary care, by raising awareness among patients and their families about the power of donation to ensure the lives of sick people on the transplant waiting list, increasing the quality of life and longevity of these people.2
In the context of Primary Health Care (PHC), although transplants are performed in specialized centers of greater complexity, this level of care plays a crucial role in the process of identifying potential donors, in pre- and post-transplant monitoring, and in health education.3 In addition, Law n° 8.080/90, which regulates the Unified Health System (SUS), guarantees universal and comprehensive access to all levels of care, including the necessary support for patients who need transplants.4 Thus, PHC acts in the early identification of problems, in maintaining the health of potential donors, and in preparing recipients, especially through monitoring clinical conditions that may evolve into the need for transplants.
Even so, challenges persist related to family refusal, lack of information about donation, and the logistics of organ procurement, especially in remote areas or those with less infrastructure, which causes the loss of potential donations in the basic health system. The role of PHC, in this sense, is essential for promoting awareness campaigns, identifying potential donors and referring urgent cases to more complex services.5 Given this scenario, the objective of this study is to study the epidemiology of organ, tissue and cell transplants in primary health care in Brazil over the last 10 years.
Study design
An exploratory study was carried out on organ, tissue and cell transplants in PHC in Brazil, through a systematic review of the scientific literature, found in the main national and international databases. This type of study consists of the grouping and synthesis of relevant research results on a given theme in a structured manner, directed to a well-defined question, constructed from the steps based on the PRISMA protocol6: Identification of the theme and formulation of the research question; search and selection of scientific articles; extraction of data from the selected studies/categorization; critical evaluation of the studies included in the systematic review; synthesis of the results and presentation of the review.
Research questionThe following guiding question was developed for the study: "What is the epidemiological profile of organ, tissue and cell transplants in primary health care in Brazil in the last decade?"
Database
Searches were conducted in bibliographic databases – PubMED, Virtual Health Library and Google Scholar. Upon completion of the searches in each database, duplicate references were excluded.
Time and language limitArticles published in the last 10 years (2015-2024), written in Portuguese and English, were selected.
Inclusion and exclusion criteriaAll original articles in the period between January 1, 2015, and December 31, 2024, available in full in Portuguese and English, were included. Original articles (quantitative or qualitative) and literature reviews (systematic, integrative, and narrative) that addressed the theme of organ, tissue or cell transplants related to primary health care in Brazil were included. In addition, studies that presented epidemiological data or information on the practice of transplantation in PHC, whether at the national or regional level, were inserted. Publications that had already been selected in the search in other databases and that did not answer the research question were excluded. Articles that distanced themselves from the theme and duplicate articles in the databases, as well as letters, editorials, and congress abstracts without full texts, were excluded.
Strategy for selecting and analyzing articlesTo operationalize the search, the following strategy was used: ("transplants") AND ("primary care") AND ("Brazil"), ("transplants") AND (primary care) AND ("Brazil"), ("organ transplants") AND (primary care) AND ("Brazil"), ("tissue transplants") AND (primary care) AND ("cell transplants") AND ("primary care") AND ("Brazil").
This strategy was adapted on each basis considering its specification. In addition, the number of publications was identified, and the selection of studies was made. This selection occurred through the reading of the titles and excluded those that are not part of the selection criterion, and then the abstracts were read and those that are of interest to the research and those that are related to the objectives of the study were selected for reading in full.
Finally, the articles that were part of the study were selected. The references captured were included in a single library in the EXCEL program, from which a table was prepared contemplating the main items of the methods and results of each selected article (author, year, country of origin of the study, design, sample studied and main results), by two independent researchers and also to be exposed later through the Prism Flow Diagram (Figure 1), used as a basis for searching and selecting articles.
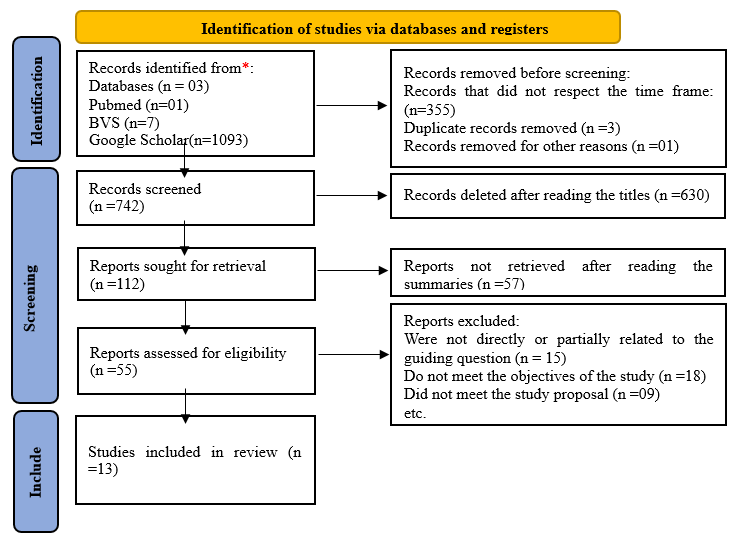
Figure 1 PRISMA Flow Diagram - Search and selection of scientific articles.
*Consider, if feasible to do so, reporting the number of records identified from each database or register searched (rather than the total number across all databases/registers). **If automation tools were used, indicate how many records were excluded by a human and how many were excluded by automation tools.This work is licensed under CC BY 4.0. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/Source: Authorship adapted from Page MJ, et al. BMJ 2021;372:n71. doi: 10.1136/bmj.n71, 2020).
Ethical aspects
The evaluation of the data was carried out in a qualitative and descriptive manner, with the objective of recognizing recurrent patterns and trends in the chosen studies, that is, the databases did not use confidential information. Therefore, submission to the Research Ethics Committee is waived due to the choice of the type of study.
The initial search resulted in 1101 publications, 7 in the BVS, 1 in PUBMED and 1093 in Google Scholar. Articles published between 2015 and 2025 were filtered and 355 samples were excluded. In addition, 3 samples were removed because they were duplicated in the databases and 1 because it was incomplete published. After reading the titles and abstracts, 55 records remained regarding eligibility. Among these, 13 articles were included in the review, since those that were not related to the guiding question were removed, did not fit the objectives or the proposal of the study. The analyzed articles are presented in Table 1, in order to facilitate the visualization and understanding of the themes of each journal. The table presents a summary of the articles with authorship and year of publication; country of origin of the study, design, and sample studied, pertinent results and observations, and main findings. It brings together 13 studies published between the years 2015 and 2025.
|
Authors/Year/Country |
Outline |
Sample |
Principal results |
|
Martins EO, et al, 2016, Brazil.7 |
Experience report |
Psychological intervention in groups in General Hospital |
Group psychological intervention can improve awareness of organ donation, potentially reducing waiting lines for transplants. |
|
Waquil EL, 2020, Brazil.8 |
Qualitative study |
Health Professionals of Transplant Teams |
It highlights the importance of the social worker in the multiprofessional team, contributing to the support of patients and families during the transplant process. |
|
Fernandes MEN, et al, 2015, Brazil.9 |
Qualitative study |
Family members of organ donors |
It identifies the feelings and challenges faced by family members after consenting to organ donation, emphasizing the need for psychological support. |
|
Pereira A, et al, 2015, Brazil.10 |
Literature review |
No applicable |
It analyzes the role of social work in the context of organ donation, emphasizing challenges and opportunities in the area. |
|
Roza BA, 2023, Brazil.11 |
Qualitative study |
Healthcare professionals and transplant patients |
It addresses good health practices and the challenges faced by professionals and transplant patients in long-term care institutions. |
|
Fagherazzi V, et al, 2018, Brazil.12 |
Experience report |
Community health workers |
The continuing education of community health agents improves knowledge about organ donation, facilitating the dissemination of correct information in the community. |
|
Silva MAH, 2022, Brazil.13 |
Cross-sectional study |
Users of primary health care units |
It reveals gaps in users' knowledge about organ donation, indicating the need for educational campaigns in primary care. |
|
Quadros Júnior WG, 2019, Brazil.14 |
Methodological study |
General practitioners |
It develops and validates an instrument to assess the knowledge of general practitioners about liver transplantation, aiming to improve continuing medical education. |
|
Souza DC, 2021, Brazil.15 |
Literature review |
No applicable |
It discusses the ethical aspects involved in organ donation, emphasizing the importance of clear guidelines and ethical education for health professionals. |
|
de Andrade DC, et al, 2024, Brazil.16 |
Cross-sectional study |
Data from potential pediatric donors |
It identifies characteristics of pediatric donors and factors that influence the effectiveness of multiorgan donation. |
|
Santos MA, et al, 2023, Brazil.17 |
Literature review |
No applicable |
It exposes the main factors that lead to family refusal to donate organs, highlighting the need for strategies to reduce these refusals. |
|
Rezende MR, et al, 2022, Brazil.18 |
Literature review |
No applicable |
It exposes the reasons for family refusal to donate organs and proposes interventions to increase consent rates. |
|
Okano CS, et al, 2023, Brazil.19 |
Descriptive study |
National transplant data |
It provides an overview of the transplant landscape in Brazil, including family refusal rates and challenges faced by the health system. |
Table 1 Main findings of the integrative literature review, including relevant methods and results
Regarding the type of methodology applied, 2 experience reports, 3 qualitative studies, 4 literature reviews, 2 cross-sectional studies, 1 methodological study and 1 descriptive study. Among the studies in the reviewed sample, prevalent themes were perceived among them. The most discussed themes were "Psychological and social aspects in organ donation and transplantation" with 5 articles addressing this topic, "Education and knowledge about organ donation and transplantation in primary care" with 4 articles that deal with it, "Factors related to family refusal in organ donation and how PA can be an incentive tool" with 4 articles that show this correlation.
Historically, the first reports of procedures similar to transplants date back to the 16th century, when there is evidence of skin grafts in experimental attempts.20 However, it was only in the 20th century that significant advances occurred due to the development of surgical techniques, the understanding of rejection mechanisms and the emergence of immunosuppressive drugs.21 In Brazil, the legal framework for organ and tissue donation and transplantation was established by Law No. 9,434/97, consolidating the regulation of collection, donation and transplantation activities at a national level. Currently, this legislation remains in force, determining that the removal of organs for transplantation depends on family authorization, and that the distribution of grafts is coordinated by the National Transplant System (SNT), ensuring priority criteria, equity and transparency in the practice of transplants.22,23
At the national level, Brazil has one of the largest public transplant programs in the world; however, it is associated with challenges such as long waiting lists, variable success rates and regional disparities in access to services.5 Furthermore, family refusal, lack of donors and infrastructure problems constitute important epidemiological obstacles, which highlight the need for awareness campaigns, logistical improvements and strengthening of health surveillance in Primary Care.
In addition, data from the World Health Organization (WHO) indicate that, globally, millions of people are waiting on the transplant waiting list, with a marked disparity between the number of donors and recipients.1 In Brazil, according to the Brazilian Association of Organ Transplants (ABTO), the country maintains one of the largest public transplant programs in the world. In 2022, 583 solid organ transplants were performed on children, a number that resembles that of 2021, which recorded 583 procedures, representing an increase of 17% compared to 2020, which had 486 pediatric transplants.2
Considering the transplant scenario in Brazil, the most prevalent themes present in the reviewed articles were the following aspects:
Psychological and social aspects of organ donation and transplantationRegarding the importance of professional intervention, Martins EO, et al7 and Waquil,8 highlight the relevance of psychological and social support for those involved in organ donation. For them, both the psychologist and the social worker are essential in raising awareness, emotional support and facilitating the understanding of the process by donors and their families, including the context of primary health care, since these professionals are included in the multidisciplinary team present at this level of care.
In addition, the issue of family members' feelings post-consent, addressed by Fernandes, et al,9 and the perceptions of social workers reported by Waquil,8 highlight the emotional burden that families face during the donation and transplantation process. The need for emotional and psychological support is a concern shared by both, highlighting the importance of interventions that consider emotions and family dynamics. Another convergent aspect is about the social aspects faced in the health area, especially in long-term care institutions and in the care of vulnerable populations. The studies by Roza,11 and Pereira, et al.,10 emphasize the search for good practices, that is, care protocols and clinical and psychosocial management strategies (continuous evaluation and monitoring, and permanent education of the multiprofessional team).
However, it is possible to observe points of divergence in the approaches presented by the articles. The focus of the intervention may change according to the professional involved: while the article by Martins, Valente and Calais7 emphasizes the individual and emotional perspective of the donor and his family, the study by Pereira, et al.,10 expands the discussion to the social context and institutional structures that influence the donation and transplantation process. This distinction can result in different interventions, as each profession tends to prioritize specific aspects in the follow-up of those involved. In addition, perceptions about the role of the social worker may differ from the role of the psychologist. In general, the social worker adopts a more communitarian approach, considering the social organization and living conditions of potential donors and recipients, while the psychologist focuses on individual emotional dynamics, helping to deal with fears, insecurities and feelings arising from the donation and transplantation process.
Rieth & Calinca24 address similar issues, highlighting the importance of psychological support in organ donation, as well as the social challenges that permeate this process. Such studies complement the discussions presented in the analyzed articles, reinforcing the need for a multidisciplinary approach that contemplates both the emotional and social aspects of organ donation and transplantation. In summary, the intersection between psychological and social practices in the processes of organ donation and transplantation outlines a highly promising field for research and intervention, requiring the collaboration of several health professionals. Therefore, only from a comprehensive and integrated understanding of these aspects will it be possible to provide better results and experiences, both for individuals and families involved in the donation and transplantation process.
Education and knowledge about organ donation and transplantation in primary careThe articles by Fagherazzi, et al.,12 Silva,13 Quadros Júnior14 and Souza,15 converge in emphasizing the relevance of knowledge and continuing education in the field of organ and tissue donation. In summary, these authors emphasize in their studies that the lack of information and the lack of awareness are obstacles that hinder the donation process, both in the context of health professionals and in the population in general.
Fagherazzi et al.,12 in their study addresses the importance of continuing education on organ/tissue donation with community health agents, since investment in training community agents promotes a more effective dissemination of information in communities, which, in turn, demystifies organ donation and facilitates family consent. This perspective dialogues with Knhis et al.,25 who highlight how maintaining informative ties and offering adequate support can reduce the cultural and emotional barriers associated with refusal.
In addition, the article by Silva13 highlights gaps in users' understanding of the donation process, pointing to the need for educational campaigns and approximation between health professionals and patients. Furthermore, this maxim converges with the proposal of Dew et al.,26 according to which the promotion of clear information and humanized reception minimize anxieties and insecurities, strengthening the willingness of family members to authorize donation.
On the other hand, Quadros Júnior,14 in Validity and reliability of an instrument for assessing the knowledge of general practitioners about liver transplantation, addresses the professional perspective, by developing and validating an instrument to assess the knowledge of general practitioners. At this point, there is a focus on technical qualification and clinical preparation, complementing previous studies that emphasize the role of community agents and users. Convergence occurs to the extent that everyone recognizes continuing education as crucial, although the article by Quadros Júnior14 highlights more specifically the need for reliable assessment instruments.
In the study by Souza,15 the discussion falls on the moral dilemmas and ethical principles surrounding donation. Unlike other studies, which emphasize the issue of knowledge and education, this article highlights the conflict between personal values, religious beliefs, and the decision to donate. At the same time, it reaffirms the importance of clear policies and professional training, corroborating the need for continuous training already mentioned by Fagherazzi et al.12 and Silva.13
Factors related to family refusal to donate organs and how PHC can be an incentive toolAmong the articles reviewed are the studies by De Andrade, et al.,16 Araujo, et al.,17 Rezende et al.18 and Okano et al.19 that converge in showing that family refusal is still one of the main obstacles to effective organ donation in Brazil, reinforcing the need for information and awareness strategies aimed at families. In summary, the articles highlight that Primary Health Care (PHC) is essential in this process, as community agents, nurses and family doctors are in direct contact with the population, which enables the construction of bonds of trust and the dissemination of knowledge about donation.
In addition, De Andrade16 focuses on the perspective of pediatric donors, given that family particularities — such as fears related to the procedure, insecurity in the face of possible complications, and cultural beliefs — can lead to denial. Similarly, Araujo et al.,17 in their literature review, show that misinformation and lack of emotional support are recurrent factors that hinder consent, suggesting that PHC can intervene by offering multiprofessional follow-up and prior clarification to the population. This idea is corroborated by Morais & Morais,27 who discuss how effective communication and awareness can positively impact the decision about organ donation, aligning with the need for interventions in PHC.
In addition, Rezende et al.,18 reinforce that family refusal is closely linked to the fragility of the moment of mourning and the absence of adequate guidance, indicating that more humanized and continuous approaches at the primary level of care can reduce refusal rates. On the other hand, Okano et al.,19 expand the discussion by analyzing the national transplant scenario and showing how the lack of consolidated public policies and regional inequalities hinder the efficiency of the system. Although there is no specific focus on family refusal, the study suggests that PHC could act as a bridge between communities and high-complexity services, helping to reduce asymmetries in access to information and post-transplant support. This perspective is reinforced by Fontenele & Cioatto,28 who discuss the relationship between public policies and efficiency in organ donation, in the scenario of unequal access to information and different levels of support received by family members.
Finally, Da Silva Costa,29 emphasize the importance of humanized approaches and psychological support during the donation process, aligning with the proposals for more continuous and sensitive interventions discussed in the reviewed texts. Thus, the evidence presented by the new authors corroborates the explicit thinking in the analyzed articles, strengthening the argument about the need for interventions in PHC to face the challenges of organ donation in Brazil.
Main limitations and future prospectsAmong the above, it is noted that the main limitation of this study was the small number of studies available within the theme analyzed. The scarcity of studies can impact the generalization of the results and limit the scope of the conclusions, making it difficult to build a more solid overview of the effectiveness and challenges of the approaches investigated.
Given these limitations, it is expected that such research will expand the evidence base on the subject, enabling the generation of more robust results that can support the formulation of more effective public policies. In this scenario, primary health care continues to prove to be a fertile ground for the development of strategies for prevention, reception, and follow-up of patients and families, especially when it comes to donation and transplantation of organs, tissues, and cells. However, for such initiatives to be effective, investments in infrastructure, training of professionals and social awareness policies become essential. Thus, the expansion of scientific evidence can support government decisions and more informed clinical practices, reinforcing the relevance of future studies aimed at filling the identified gaps and strengthening the performance of primary care in this context.
The studies analyzed show that organ, tissue and cell transplants in Brazil depend on an integrated approach that involves both clinical and socio-emotional aspects. In this scenario, transplantation is supported by the legal framework established by Law No. 9,434/97, as well as the consolidation of the National Transplant System (SNT), ensuring criteria of priority, equity, and transparency in the distribution of grafts. In this perspective, Primary Health Care (PHC) plays a key role in identifying potential donors, pre- and post-transplant follow-up, and health education, especially when considering regional disparities and long waiting lists.
However, obstacles such as family refusal, lack of donors, misinformation and insufficient infrastructure remain major challenges. Family refusal, in particular, is closely related to the lack of prior knowledge and emotional vulnerability at the time of grief, making it essential for trained professionals in PHC to provide support and information, from the care offered in primary health care. In this sense, the continuing education of community health agents and general practitioners, is important to better clarify doubts about organ donation, as well as the sensitization of users and family members, emerges as a key strategy to promote awareness and reduce cultural and emotional barriers, to highlight the relevance of this act as a second chance at life for patients who need donations and increase the number of families willing to donate organs.
Based on this evidence, it is concluded that the effectiveness of transplants in Brazil is not limited to high complexity but involves a solid structure of epidemiological surveillance of potential donors and information campaigns at the primary health care level to encourage family members to participate in the organ donation process to increase the amount of donations within the Brazilian epidemiological context. Public policies should therefore strengthen PHC based on information, disease identification and referral of potential recipients, ensuring comprehensive and humanized care for patients and family members who experience the donation and transplant process. Therefore, the family understands the relevance of this action and the reliability of the procedures of this process until the transplant is successful, believing in the greatness of this gesture to save and restore quality of life to those on the transplant waiting list.
None.
The authors declare there is no conflict of interest.
None.

©2025 Almeida, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.