MOJ
eISSN: 2379-6383


Research Article Special Issue II Primary care services
1Federal University of Maranhão, Medicine Course, Pinheiro, Maranhão, Brazil
2Medicine, IESVAP- Instituto de Educação Superior do Vale do Parnaíba, Brazil
3Medicine, Centro Universitár io FACID Wyden, Brazil
4Federal University of Maranhão, Dentistry, Brazil
Correspondence: Consuelo Penha Castro Marques, Universidade Federal do Maranhão, Brasil, Tel (98) 99100-7752
Received: March 23, 2025 | Published: April 10, 2025
Citation: Silva LF, Almeida GT, Leite BCC, et al. Diagnosis and emergency outpatient care in psychiatry in primary care in Brazil: 2015 to 2024. MOJ Public Health. 2025;14(1):89-94. DOI: 10.15406/mojph.2025.14.00476
Introduction: Psychiatric emergency care in Primary Health Care (PHC) in Brazil faces challenges such as lack of professional training and standardized protocols. PHC is essential in the Psychosocial Care Network (RAPS), but work overload and stigma associated with mental disorders impact the quality of care. This study analyzes the profile of emergency outpatient psychiatric care in PHC in Brazil (2015-2024).
Methodology: Integrative and descriptive literature review. Data collection in the SCIELO, PubMed, LILACS and Google Scholar databases, using descriptors such as "Primary Health Care", "Psychiatric Emergency", "Mental Health Services", "Professional Training". Inclusion criteria: articles in Portuguese and English, published from 2015 to 2024, related to emergency outpatient psychiatric care in PHC.
Results: The initial search resulted in 261 publications, with 13 articles included in the review. The prevalent themes were: "Profile and Characteristics of Emergency Outpatient Care in Psychiatry", "Challenges of PHC in Managing Psychiatric Emergency Demands" and "Potential and Strategies for Comprehensiveness and Quality of Mental Health Care". The studies point to the presence of mood disorders and substance use, the need for family support, the lack of professional training and the importance of networking.
Final considerations: PHC has the potential to deal with psychiatric emergencies, but it faces structural and organizational challenges. It is essential to invest in professional training, standardized protocols and integrated public policies to improve the comprehensiveness and quality of mental health care. Future studies should expand the evidence base and investigate different socioeconomic realities.
Keywords: primary health care, psychiatric emergency, mental health services, professional training, mental health, primary care
Psychiatric emergency care in Primary Health Care (PHC) represents a challenge in Brazilian medical practice, requiring adequate capacity for the identification and initial management of mental health crises. In this context, PHC plays a fundamental role in organizing the flow of people, classifying risk, and making appropriate referrals, since it is the gateway for receiving these patients.1 Thus, the Psychosocial Care Network was created with the aim of expanding access to mental health for the population, ensuring humanized and effective service for all.2
However, it is noted that the lack of training of professionals and the availability of standardized protocols are a current problem for health services, resulting in excessive referrals to specialized services that contribute to the overload of more complex units. It is therefore evident that ongoing training of PHC professionals is necessary to qualify mental health care and attention. According to De Paula et al.,3 nursing professionals are the group with the greatest contact with patients in crisis, being responsible for welcoming the patient and classifying the care. However, in the same study, the same professionals report speeches of technical unpreparedness, feelings of stigmatization towards patients, and feelings of anguish and fear at the time of care.3
Other studies also suggest that work overload (in addition to insufficient specific training) generates insecurity in the proper management of cases. Thus, many professionals report difficulties in differentiating situations that require emergency intervention from those that can be monitored routinely.4 In addition, other challenges still stand out, such as the stigma associated with mental disorders, the impact of which is demonstrated both by patients' adherence to treatment and by professionals' willingness to deal with these conditions.
This scenario shows how mental health services and PHC still face structural and organizational barriers, which directly impact the continuity of care and the effectiveness of treatment at the time of a psychiatric emergency. In this sense, it becomes the duty of Primary Care to guarantee actions for health promotion, prevention, protection, diagnosis, treatment and rehabilitation also for psychiatric patients.2 These actions are developed mainly with ongoing education, which trains this multidisciplinary team not only in the immediate control of the crisis pharmacologically, but also in ensuring adequate and safe management in a psychiatric crisis.1
Given this reality, this study aims to study the profile of emergency outpatient psychiatric care in primary care in Brazil, from 2015 to 2024. The aim is to understand the characteristics of the patients treated, as well as the challenges and potential of PHC in managing these demands, aiming to improve the comprehensiveness and quality of mental health care.
This work is a literature review with an integrative and descriptive approach, whose objective is to gather and analyze data related to emergency outpatient psychiatric care in primary health care in Brazil, between 2015 and 2024. Data collection was carried out in the following databases: Scientific Electronic Library Online (SCIELO), PubMed, Latin American and Caribbean Literature in Health Sciences (LILACS) and Google Scholar. For the selection of articles, the following descriptors and their combinations were determined in Portuguese and English: "Primary Health Care"; "Primary Health Care"; "Psychiatric Emergency"; "Mental Health Services"; "Professional Training", using the Boolean operator “AND” or “OR” (in cases of search expansion).
As inclusion criteria for the study, articles published in Portuguese and English that addressed the topic of the review (directly related to outpatient psychiatric care in PHC) and that had been published and indexed in the respective databases between 2015 and 2024 were selected. As for the exclusion criteria, duplicate articles and articles that were not made available in full were excluded. After searching for articles, those that were directly related to the topic analyzed were selected, respecting the inclusion and exclusion criteria, and analyzing them first according to the title, followed by the abstract and, finally, the full text.
The entire process followed the data flow diagram by Page et al.,5 as shown in Figure 1 in the appendix. Subsequently, the articles that were selected and analyzed were made available in a table containing the main information provided. Thus, their data were conducted in a descriptive manner, allowing the authors to observe, classify, and present them. As this is a literature review based on secondary data in the public domain, this study does not require approval by a Research Ethics Committee, in accordance with Resolution 466/12 of the National Health Council.
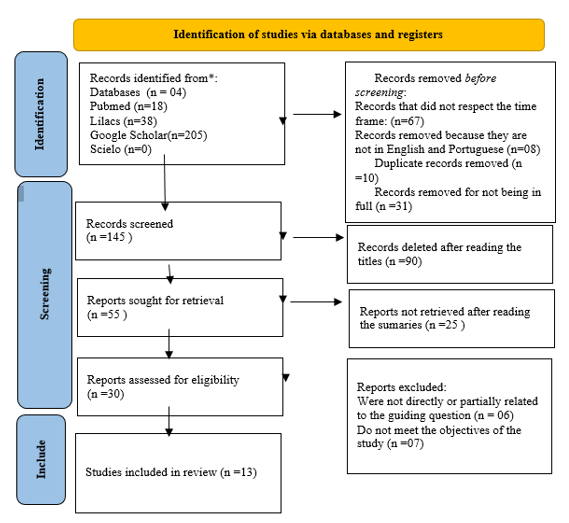
Figure 1 PRISMA Flow Diagram - Search and selection of scientific articles.
*Consider, if feasible to do so, reporting the number of records identified from each database or register searched (rather than the total number across all databases/registers).
**If automation tools were used, indicate how many records were excluded by a human and how many were excluded by automation tools.
This work is licensed under CC BY 4.0. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/
Source: Authorship adapted from Page MJ et al.5
The initial search resulted in 261 publications, 38 in Lilacs, 18 in PUBMED, 0 in Scielo and 205 in Google Scholar. Articles published between 2015 and 2024 were filtered and 67 samples were excluded. Furthermore, 10 samples were removed because they were duplicated in the databases, 8 because they were not in Portuguese or English and 31 because they were incompletely published. After reading the titles and abstracts, 30 records remained as eligible. Of these, 13 articles were included in the review, since those that were not related to the guiding question, did not fit the objectives or the proposal of the study were removed. The articles analyzed are presented in Table 1, in order to facilitate the visualization and understanding of the themes of each journal. The table presents a summary of the articles with authorship and year of publication; country of origin of the study, design, sample studied and main results. It brings together 13 studies published between 2015 and 2024.
|
Article |
Author(s) |
Year |
Country Origin |
Design |
Sample Studied |
Main Results |
|
Difficulties in providing psychiatric urgent and emergency care in the mobile emergency care service |
Oliveira et al.,8 |
2018 |
Brazil |
Descriptive, exploratory and qualitative research |
34 professionals from the nursing team at SAMU in Mossoró/RN |
Nursing care for users in psychiatric emergencies is inadequate, mainly due to the lack of a structured and effective mental health service network. |
|
Reflections on the support network of users of a mental health reference center in belo horizonte based on the experience of the Gam group |
Santos MAB et al,.21 |
2021 |
Brazil |
Experience report |
Participants of a GAM group at a Mental Health Reference Center in Belo Horizonte |
The GAM strategy proved to be a tool capable of bringing workers and users together into a collective space for the production of care, despite difficulties such as low adherence. |
|
Psychosocial rehabilitation in the western network of the municipality of São Paulo: potential and challenges |
Nóbrega MPSS et al.,20 |
2018 |
Brazil |
Qualitative and descriptive study |
123 higher education professionals in the health area out of the 263 working in the network that were listed in the National Registry of Health Establishments in Brazil. |
The lack of trained professionals, the lack of integration between services and the importance of family support for the success of psychosocial rehabilitation were identified. Difficulties in the articulation of the network were pointed out, although there is potential in multidisciplinary and community involvement. |
|
Feelings of family members of patients admitted to psychiatric emergency services: a look at the family |
Carla et al.18 |
2016 |
Brazil |
Descriptive-exploratory with a qualitative approach |
Twenty family members of people with mental disorders treated at the Psychiatric Emergency Department of a Public Hospital in the interior of the State of São Paulo participated. |
Family members reported anguish, fear and insecurity, highlighting the need for multidisciplinary support and care. The importance of care strategies that consider emotions and family dynamics was highlighted, as well as the creation of bonds between staff and family to facilitate the hospitalization and post-discharge process. |
|
Mental health nursing consultation in primary health care |
Bolsoni EB et al.12 |
2015 |
Brazil |
Qualitative study |
Seven nurses who make up the Family Health Strategy Team, linked to a Health Center |
Nurses emphasized the importance of nursing consultation in the early identification of mental health problems, as well as in creating a bond with the user. It was concluded that mental health training in PHC contributes to timely referral and continuity of care. |
|
The labyrinth and the minotaur: mental health in primary health care |
Hirdes A and Scarparo HBK.14 |
2015 |
Brazil |
Literature review |
Not applicable |
The fragmentation of mental health care in PHC and the need for integrative public policies were identified. The authors discuss the metaphor of the “labyrinth” as a reference to the difficulties of the user in navigating the care network, suggesting strategies for articulation between levels of care. |
|
Psychosocial support in times of COVID-19: experiences of new management strategies and mutual aid in southern Bahia, Brazil |
Cruz et al.,15 |
2020 |
Brazil |
Experience report |
Professionals and users of services from the Psychosocial Care Network (RAPS), in the municipalities of Ilhéus and Itabuna |
The use of digital technologies and mutual aid groups has proven effective in ensuring the continuity of mental health care during the pandemic, despite limited access and connectivity difficulties. The importance of innovation and networking to address the restrictions imposed by COVID-19 is highlighted. |
|
Who lives here?: reflections on primary health care teams’ understanding of therapeutic residences |
França AB,9 |
2023 |
Brazil |
Qualitative study |
Primary Health Care Professionals |
Little knowledge was identified among professionals about the dynamics of therapeutic residences and difficulties in articulating with the Psychosocial Care Network. The need for training and ongoing education to strengthen comprehensive mental health care is highlighted. |
|
“Mental Health Observatory” as a permanent education device in primary health care |
Figueiredo et al.,2 |
2022 |
Brazil |
Experience report |
|
The “Mental Health Observatory” functioned as a space for exchange and continued training, promoting reflections on care practices and strengthening integration among professionals. It was found that continuing education initiatives can improve the quality of care for psychiatric emergencies at the primary level. |
|
Mental health care network: view of the coordinators of the family health strategy |
Eslabão et al.,10 |
2017 |
Brazil |
Qualitative study |
Six ESF coordinators, four nurses, one doctor and one social worker |
The coordinators pointed out weaknesses in the articulation between primary care and mental health services, highlighting the need for integrated actions to ensure continuity of care and the acceptance of psychiatric demands. |
|
Profile of psychiatric emergency care in an emergency health service |
Carrijo et al.,7 |
2022 |
Brazil |
Cross-sectional study |
Patients treated in the emergency department of a public hospital located in the Araguaia Valley |
Most of the cases involved mood disorders and substance use, with a high rate of recidivism. It was concluded that coordination with primary care and the provision of post-discharge follow-up could reduce readmissions and improve patients' prognosis. |
|
Attendance to psychiatric urgencies and emergencies in primary care: challenges involved in caring |
Leocádio et al.,1 |
2022 |
Brazil |
Qualitative study |
Professionals working in primary care in psychiatric emergencies and urgent care |
Professionals reported insecurity and lack of training to manage psychiatric emergencies, indicating a lack of specific protocols and specialized support. Regular training and partnerships with mental health services are suggested. |
|
Pharmaceutical assistance and public policies in mental health in the municipality of Pinhais – Paraná |
Boeira FO and Andrade CA.6 |
2017 |
Brazil |
Literature review |
Not applicable |
Weaknesses were found in the supply of psychotropic medications and in the implementation of public mental health policies. The article emphasizes the need for integration between the different levels of care and strengthening of pharmaceutical assistance actions in PHC to ensure access and continuity of treatment. |
Table 1 Main findings of the integrative literature review, including relevant methods and results
Source: Prepared by the authors, 2025.
Regarding the type of methodology applied, 3 experience reports, 4 qualitative studies, 2 literature reviews, 1 cross-sectional study, 2 descriptive-exploratory and qualitative studies and 1 qualitative and descriptive study. Among the studies in the reviewed sample, prevalent themes were noted among them. The most addressed themes were “Profile and Characteristics of Emergency Outpatient Care in Psychiatry” with 2 articles addressing this theme, “Challenges of PHC in Managing Psychiatric Emergency Demands” with 4 articles addressing this theme and “Potentials and Strategies for Comprehensiveness and Quality of Mental Health Care” with 7 articles showing this correlation, with the country of origin being entirely Brazil.
Among the most prevalent themes present in the reviewed articles, the following aspects were addressed:
Profile and characteristics of emergency outpatient care in psychiatry
Regarding the profile of emergency outpatient psychiatric care, the studies analyzed,6,7 highlight the marked presence of mood disorders and substance use, evidencing the complexity of the cases that reach emergency services. In particular, the article by Boeira and Andrade6 emphasizes the perspective of family members, revealing the emotional overload and the need for support in the face of psychiatric hospitalization. At the same time, Carrijo et al.7 reinforce the importance of effective coordination with Primary Health Care (PHC), in order to offer continuity of care and early monitoring of risk factors for relapses.
Therefore, it is observed that these studies converge in highlighting the need for management protocols that consider both the clinical condition of patients and the experience of family members. While Boeira and Andrade6 focus on welcoming and understanding family dynamics, Carrijo et al.7 highlight the epidemiological profile and main demands related to mental disorders in emergencies. Despite the differences in focus, both advocate the adoption of integrated strategies, in which PHC can play a role in screening and monitoring patients and family members, reducing the impact of crises and promoting more resolute and humanized care.
Challenges of PHC in managing psychiatric emergency demands
Within the scope of the challenges faced by PHC in the management of psychiatric emergencies, the articles by Oliveira et al.,8 Leocádio et al.,1 França9 and Eslabão et al.,10 present an overview of the structural, formative and organizational limitations that hinder comprehensive care. Furthermore, Oliveira et al.8 point out the lack of a structured and resolute service network as one of the main factors that compromise the adequate management of psychiatric emergencies in SAMU, while Leocádio et al.,1 highlight the insecurity of professionals in primary care, who report a lack of specific protocols and specialized support.
On the other hand, Amanda Barbetta França (2023) discusses the understanding of PHC teams regarding therapeutic residences, highlighting knowledge gaps and difficulties in integrating them with the mental health network. In this sense, Eslabão et al.10 corroborate the idea that the weak articulation between PHC and specialized services affects the continuity of care and the resolution of psychiatric emergencies. This fragmentation of the network, associated with insufficient training, is in line with the reflections of Facchini et al.,11 who emphasize the need for continuous training and clear protocols to face the complexity of psychiatric crises. In short, these studies converge in defending the relevance of PHC as a gateway and monitoring of mental health cases, but they diverge in the way they address specific aspects, such as the participation of SAMU or the understanding of therapeutic residences.
Potentials and strategies for comprehensive and quality mental health care
Regarding the perspectives for action and the potential of Primary Health Care (PHC) to deal with psychiatric emergencies, the reviewed articles point to promising paths, although still incipient in many contexts. Studies such as that of Bolsoni et al.,12 for example, highlight the importance of nursing consultation in mental health, showing that early detection of mental health problems in PHC can prevent crises and reduce hospitalizations. This preventive and continuous approach reinforces the ideas of Mendes,13 who advocates the adoption of specific protocols and training for the multidisciplinary team, ensuring safer and more humanized care.
Furthermore, Hirdes and Scarparo,14 when discussing the metaphor of the “labyrinth and the minotaur” in mental health, emphasize the need for integrated public policies that consider PHC as the articulating axis of the psychosocial care network. This concept is echoed by Cruz et al.,15 whose report of experience in psychosocial support during the COVID-19 pandemic highlights the capacity for innovation and adaptation of PHC, especially when implementing digital technologies and mutual aid strategies. Such initiatives, although challenging, show that the proximity of PHC to the community can be a differential for the support of users in vulnerable situations, including in crisis scenarios.
On the other hand, Figueiredo et al.,2 propose the “Mental Health Observatory” as a permanent education device in PHC, suggesting that the continuous qualification of professionals can substantially improve the management of psychiatric emergencies. At this point, the reflections of Cordeiro et al.,16 and Peduzzi17 reinforce the relevance of training and discussion spaces that promote the exchange of knowledge between teams and the development of evidence-based practices. Thus, PHC not only fulfills its role of first contact and longitudinality, but also strengthens itself as a strategic instance for the comprehensiveness of mental health care.
In summary, there is a consensus regarding the potential of PHC to act as a link between the community and highly complex services, preventing the worsening of psychiatric crises and ensuring closer and more humanized support. However, for these initiatives to be consolidated, it is essential to coordinate public policies, provide ongoing training for teams, and implement protocols that unify conduct and facilitate decision-making. In this way, PHC actions, supported by a well-structured support network, can effectively improve the comprehensiveness and quality of care for patients in psychiatric emergencies.18–21
Main limitations and future perspectives
Among the above, it is noted that the main limitation of this study was the reduced number of studies available within the analyzed theme. The scarcity of studies can impact the generalization of the results and limit the scope of the conclusions, making it difficult to build a more solid overview of the effectiveness and challenges of the investigated approaches.
Given these limitations, it is expected that such research will expand the evidence base on the topic, enabling the generation of more robust results that can support the formulation of more effective public policies. In this sense, it is recommended that multicenter studies be carried out, encompassing different regions and socioeconomic realities, in order to contemplate the diversity of scenarios found in primary care. In addition, investigations that combine quantitative and qualitative methods can deepen the analysis of the factors that influence the profile of patients, the challenges of network integration and possible innovations for mental health care. Thus, based on a broader and more diverse sample, it will be possible to strengthen the debate about the effectiveness of the approaches analyzed and propose structural changes that meet the needs of users, family members and PHC professionals, thus promoting more comprehensive and effective care in psychiatry.
Thus, this study demonstrated that Primary Health Care professionals face significant challenges in managing psychiatric emergencies and urgencies, often resulting from gaps in training and continuing education in mental health, which leads to the reassignment of patients to other levels of care, such as secondary and tertiary care. In addition, this can be seen in the city of Fortaleza-CE, where only 23% of mental health care occurs in primary care and 37% of initial care is already provided in high complexity care, which overloads the health system and compromises the principle of hierarchy proposed in the SUS.22 In addition, the lack of clear protocols and the difficulty in articulating with the Psychosocial Care Network compromise the quality of care provided. To improve care, it is essential to invest in the continuing education of health teams, develop specific educational materials, and strengthen the referral and reception flows for these patients. Such measures can promote more humanized and effective care, in line with the principles of the Unified Health System.
None.
The authors declare there is no conflict of interest.
None.

©2025 Silva, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.