MOJ
eISSN: 2379-6383


Research Article Volume 11 Issue 2
University of Louisville, School of Public Health and Information Sciences, Department of Health Management and Systems Sciences, Louisville, KY, US, USA
Correspondence: Naiya Patel, University of Louisville, School of Public Health and Information Sciences, Department of Health Management and Systems Sciences, Louisville, KY, U.S, USA
Received: October 20, 2021 | Published: May 27, 2022
Citation: Patel N. Building a culture of health in Kentucky to address racism a public health crisis. MOJ Public Health. 2022;11(2):75-81. DOI: 10.15406/mojph.2022.11.00379
Importance: Health disparities are the leading underlying cause for disproportionate pandemic effect. A sustainable solution must inculcate and address key community stake holders needs to implement strategies. Racism is recently identified as a public health crisis and in order to address it a sustainable multidisciplinary strategy calls for action. Clearly existing solutions are not sustainable and effective and is evident through the case study of Kentucky in the current research. The elimination of health disparities is a multidisciplinary and cross sector approach which the RWJF action framework inculcates.
Observations: Kentucky State has the Gini and Social Index Score that needs urgent attention. Racial segregation is prominent among the black versus white compared to other racial minorities. Income inequality is highest among the blacks than the other minorities and white in Kentucky. Infant mortality rate, premature deaths, preventable hospitalizations, and unhealthy behavior is highest among the black community members compared to their white counterparts.
Conclusions and Relevance: The identified sustainable strategy and entry points for key Kentucky stakeholders can help address the racism. The stakeholder analysis matrix of the research can help implement proposed strategy feasibly and effectively. The action framework itself is structured in a way that the issues framed utilizing the model can help disseminate and implement the strategy sustainably.
Keywords: racism, culture of health, RWJF framework, public health
A nation’s asset is the health of its citizen because if the citizens are not well, the nation's economy and families struggle while the national security is at stake.1 Health inequity in the United States has led to a 4-year gap in life expectancy among different racial and ethnic groups.1 Although access to affordable and needed health care is not the only solution, one must also consider social determinants of health to narrow the gap.1 Hence, health equity could be defined as the perfect state in which individuals can achieve their full health potential without any barriers to achieving it.2,3 The opportunity to attain that full potential for well-being depends on the living and working conditions and other resources enabling people to achieve that potential to be healthy.4
Health Disparities serve as metrics for assessing progress towards health equity; hence, both concepts are interrelated.4 Poverty is not just about an individual's low income but about the combined effect of three cores like economic success, power and autonomy, and being valued in the community.5 To rise from poverty, i.e., mobility from poverty, all three areas mentioned must be measured and acted upon as ignoring one of these might leave the individual at struggle.5 Gini Index is one measure to determine income distribution equality among the population of a community.6 Social Capital Index measures a community’s social stability and well-being, both perceived and actual.7
Community-based solutions like an action, program, policy, or law that is driven by community-based organizations, faith-based organizations, “employers, healthcare systems and providers, public health agencies, policymakers, and others” have the potentials to improve health equity by influencing health and factors affecting inequities.2,8
The vital steps for achieving health equity includes identification of essential health disparities concerning affected stakeholders, changing law, environment, and practices to eliminate inequities, evaluating the short and long term efforts and outcomes, and finally reassessing those existing strategies to plan the next steps.4 Policies impact health factors, affecting health outcomes like length and quality of life.9 The elimination of health disparities is a multidisciplinary and cross sector approach which the RWJF action framework inculcates. Hence the objective of current review is to evaluate, frame and devise solution surrounding racism and health equity in Kentucky state utilizing RWJF action framework. To frame and devise solution the review first performs Kentucky state descriptive analysis by dividing raw data into categorizes (I-VI). After determining the assets, resources as well as health equity status at county level the RWJF action framework is utilized to frame and devise solution (Table 12) keeping in mind the status quo.
The data for the Kentucky state has been analyzed in STATA SE 16 for the descriptive analysis, the data utilized is collected from two data sources: Kentucky 2020 County Health Rankings10 and the opportunity insights website.11 The raw publicly available data was in csv format which was uploaded in STATA for cleaning and refinement. The data is categorized at the following levels to understand Kentucky demographics that might influence health disparity:
Health outcomes
The overall life expectancy in the Kentucky State is about 74 years lower than the national average, as depicted in Table 510 of the Appendix. By stratifying the life expectancy through the different races, Blacks have the lowest life expectancy years compared to other races, while the data for AIAN was missing in the file. The premature mortality is highest (about 582 deaths) among the blacks in Kentucky as of 2020, as depicted in Table 6 of Appendix. The Child Mortality among black seems to be the highest (about 111deaths per 100,000 population) among all races and the state average as depicted in Table 7 of Appendix. The infant mortality also appears to be disproportionately higher (14 deaths per 1000 live births) among Blacks than other available race data in the dataset, as depicted in Table 8.
Behavior
As depicted in Table 9, about 15% of the Kentucky population lacks adequate food access, while 4% of the population are low-income groups who do not live near a grocery store. The percentage of adults who report fewer than seven hours of sleep in Kentucky is high, making about 39% of the state's population. For emotional, physical, and mental well-being, it's essential to have sufficient sleep daily (about 7 hours).10
Preventive and healthcare services outcome
As depicted in Table 11, the average number of physically unhealthy days is higher than the national average for Kentucky (5.03). The percentage of low-birth-weight babies among Black and American Indian/Native Alaskan is the highest (about 16%) than state and national average. The rate of adults with obesity is higher than the national average (35%) in Kentucky. The reason might be a lower physical activity (31%) and limited access to exercise opportunities (56%), lower than the national average. The preventable hospitalizations among the blacks are the highest (9072) compared to other races in the Kentucky state, while the state is above (6648) the national average. About 5% of the population below age 65 are uninsured in Kentucky (Figure 2). The total number of households with at least one disabled family member is 571,016 in Kentucky (Figure 1). The total population above 65 years of age is 778,913 (Figure 1).
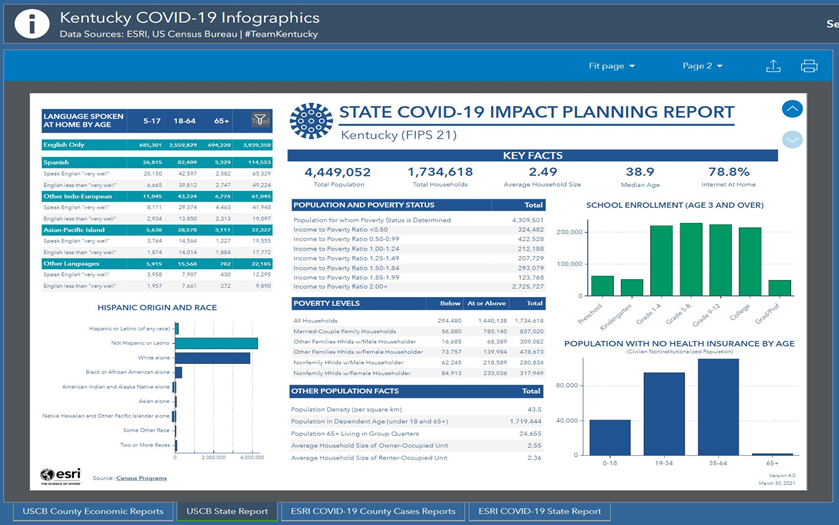
Figure 2 Kentucky State demographic snapshot.19

Figure 3 Proportion of business and employer sectors in KY where dots represent comparison to United States.
Educational and income outcomes
As per Table 4 of Appendix, the School expenditure per student seems to be low in Kentucky State than at the national level.11 The test score percentile is very low (-1.44), indicating other factors that might have impacted the lower scores. Only 0.5% of college students graduated college as of 2014 in Kentucky on an average. The median household income was the lowest ($45,279) in Kentucky compared to the national average, as depicted in Table 10. Among the racial income inequity, blacks have the most insufficient median household income ($34,503) than their counterparts, making it lower than the state average median household income. As depicted in Figure 1, 78.8% of the household has internet access.
Social and environmental outcomes
It is evident from Table 2 that there persist a problem of both racial segregation (5%) and higher poverty rates (19%) than at the national level in Kentucky.11 The Social Capital index is on an average negative (-0.5) which is not a good indication of Kentucky’s social stability and well-being. The Gini index is high (40%), indicating income inequality from the data. The local government expenditure seems to be relatively low on the local community welfare activities ($1393) in the Kentucky state as of 2014 (Table 4). The percentage of teens 16-19 years who are neither in school nor working in Kentucky in 2020 was high, making about 11% of the age group (Table 9). Among the racial residential segregation, the most significant segregation is among black and white races scoring the highest among all racial segregation (47.6). As depicted in Table 10, the proportion of the population living in the rural area is highest in the state of Kentucky (71%), meaning limited healthcare and other needed resources.12 The highest proportion of racial group comprising of Kentucky state population is black (about 4%) compared to other races.
Occupational and commute/work conditions
It is evident from Table 3 that a higher proportion of commuters (33%) commute to work for more than 15 minutes one way residing in Kentucky State.11 The diversity in terms of nonnative residents of Kentucky is low (1%), which could mean culturally less diverse. Finally, the inflow and outflow migration rate is slow (2%) in the state of Kentucky as of 2014, indicating fewer opportunities or interest for those who might be considering relocation for one or the other reason. Figure 1 reflects the total number of Kentucky households with cars and internet service.
The presence of racism at the individual and structural level impacts the ability to land good opportunities and results in overall poor physical and mental health.13 People of color, especially the black community, are more prone to bear the burden of disproportional health (Race, Racism and Health, n.d.), as evident in the Kentucky State data analysis. The black racial population tends to suffer from disproportional life expectancy, premature deaths, infant mortality, racial segregation of housing opportunity, and risks of chronic diseases/conditions compared to their White counterparts.13, 14 This health inequity exists partly from “the stress of being ignored, silenced or oppressed”.13,15 Health disparities tend to worsen among racial and ethnic minorities due to microaggression, stigma, racism, discrimination, conscious and implicit bias, ultimately contributing to poor health outcomes.16 It is also established that health inequities are closely related to historical and contemporary injustices like racism.15 Racism harms one’s educational attainment, ability to gain/seek employment and diminishing potential wages.15 Racial segregation is associated with higher deaths, exposure to environmental toxins, lower tax bases, fewer job opportunities, and fewer services like healthcare and others.15 Health inequities would decline significantly if racism is addressed/eradicated through a culture of health.15 The Robert Wood Johnson Foundation action framework helps frame such issues by identifying ways to create a culture of health.15 Individual’s, State’s, Businesses, and Community’s pathways to progress are framed through racial equity, diversity, and inclusion.17
Potential solutions to eradicate racism at all levels includes the involvement of stakeholders of the particular state/county. Grassroots organizations and community members of any state serve as the heart of civil rights activities15. In the past, community and grassroots level activities have solved issues of local racial segregation.15
The key stakeholders of Kentucky State can be divided as described in Table 12. The group categorization has been informed by Economic tracker18 and Esri databases for Kentucky19data. The proposed entry points and actions for each stakeholder with Government above all seem appealing, as depicted in Table 12 of Appendix. The decision matrix guides the reasons being informed by the level of interest, influence, and impact. The impact and interest being the significant decision-maker for the reasons behind the agreement to implement the devised strategy. At the same time, the level of influence acts as a facilitator for implementing the devised strategy proposed for stakeholders.
Recently, businesses tend to adapt the stakeholder capitalism model where businesses and corporates care about consumers and the planet and their profits.20 The several ways in which racism is bad for any business is: it reduces creativity, encourages toxic work culture, causes higher health issues and absenteeism among vulnerable employees, tarnishes reputations of the business, and lose its customer who intends to discontinue giving business to those without anti-racist approach in their business model.20 Hence it is obvious that businesses cannot afford to lose their economic profits, which partially depends on their market reputation, thriving work culture, and efficient employees.20 It is also evident through a pandemic situation that a sustainable solution to address the business inequities needs to be implemented for inclusive growth and improved economic growth.21
As proposed prior in this paper, building a culture of health can help address racism and health inequities associated with it. The stakeholder needs have been identified, and Table 12 in Appendix has been made, including the following constructs. Each construct of the action framework has been identified as entry points for identified stakeholders of Kentucky. The following section identifies guided determinants, root causes of health inequity associated with racism and proposes potential informed recommendations to address each root cause by devising informed strategies in Kentucky.
Variable |
Obs |
Mean |
Std.Dev |
Min |
Max |
High School Graduation Rate |
121 |
94.54382 |
3.34823 |
84.0796 |
100 |
Unemployment Rate |
121 |
5.189599 |
1.508778 |
3.089299 |
13.23993 |
Children in Poverty % |
121 |
26.75124 |
9.049274 |
5.1 |
47.8 |
Income Inequality Ratio |
121 |
4.992088 |
0.788185 |
3.418552 |
8.689388 |
% Single Parent Household |
121 |
32.16366 |
6.735583 |
16.60583 |
59.37962 |
Social Association Rate |
121 |
9.324993 |
4.763207 |
0 |
21.39249 |
Violent Crime Rate |
121 |
96.99403 |
76.79928 |
0 |
611.9961 |
Injury Death Rate |
121 |
52.52026 |
9.772699 |
28.17746 |
76.62735 |
Table 1 Descriptive Statistics of Kentucky County Health Ranking 2020 Data analyzed in STATA SE 16
Variable |
Obs |
Mean |
Std. Dev. |
Min |
Max |
Income Segregation |
120 |
0.018153 |
0.023173 |
-0.01336 |
0.122421 |
Poverty Segregation |
120 |
0.016597 |
0.022584 |
-0.0195 |
0.111999 |
Affluent Segregation |
120 |
0.017671 |
0.024328 |
-0.00023 |
0.133435 |
Racial Segregations |
120 |
0.054975 |
0.049676 |
0 |
0.314367 |
Gini Index |
119 |
0.395363 |
0.073873 |
0.256237 |
0.667314 |
Poverty Rate |
120 |
0.189644 |
0.081844 |
0.040617 |
0.453801 |
Social Capital Index |
120 |
-0.50087 |
0.943469 |
-2.81523 |
2.296285 |
Total Crime Rate |
111 |
0.00486 |
0.003034 |
0.000557 |
0.014219 |
Table 2 Descriptive Statistics of Kentucky in terms of segregation, social capital and criminal rates 2001-2014 data obtained from opportunity insights data11
Variable |
Obs |
Mean |
Std. Dev. |
Min |
Max |
Percent Foreign Born |
120 |
1.03499 |
0.948933 |
0.024123 |
5.929861 |
Migration Inflow Rate |
120 |
0.026091 |
0.016796 |
0 |
0.087285 |
Migration Outflow Rate |
120 |
0.024942 |
0.013259 |
0.005352 |
0.096035 |
Fraction with commute <15 min |
120 |
0.326861 |
0.081253 |
0.131928 |
0.520546 |
Table 3 Diversity, Work Commute and Migration rate in Kentucky11
Variable |
Obs |
Mean |
Std. Dev. |
Min |
Max |
School Expenditure per Student |
120 |
6.027548 |
0.980357 |
4.542789 |
11.69031 |
Student Teacher Ratio |
120 |
16.43781 |
1.587526 |
13.23408 |
23.48847 |
Test Score Percentile |
120 |
-1.44589 |
6.588962 |
-16.3302 |
17.73723 |
High School Drop Out Rate |
119 |
0.000446 |
0.016195 |
-0.03697 |
0.06976 |
College Tuition |
38 |
5103.171 |
4400.208 |
760 |
16900 |
Percent College Grads |
38 |
0.0054 |
0.166465 |
-0.23421 |
0.493859 |
Local Government Expenditures |
120 |
1393.42 |
483.3133 |
773.7278 |
4035.796 |
Table 4 Schooling and Community expenditure Factors11
Variable |
Obs |
Mean |
Std. Dev. |
Min |
Max |
Life Expectancy by County |
121 |
74.44711 |
2.191061 |
69.01621 |
79.68335 |
Life Expectancy AIAN |
0 |
||||
Life Expectancy Asian |
7 |
86.08179 |
4.157813 |
79.79357 |
91.63269 |
Life Expectancy Black |
27 |
74.9775 |
3.604984 |
70.09911 |
86.30023 |
Life Expectancy Hispanic |
14 |
92.79797 |
6.084781 |
84.78469 |
105.5274 |
Life Expectancy White |
28 |
76.33139 |
1.457072 |
73.52878 |
79.34388 |
Table 5 Additional Measures (Life Expectancy) of County Health Ranking 2020 Kentucky Data10
Variable |
Obs |
Mean |
Std. Dev. |
Min |
Max |
Number of Premature Deaths |
121 |
1228.083 |
6795.902 |
46 |
74299 |
AIAN Premature mortality |
0 |
||||
Asian Premature mortality |
4 |
208.9392 |
96.01848 |
112.7282 |
326.7715 |
Black Premature mortality |
36 |
582.124 |
162.1248 |
282.478 |
1012.808 |
Hispanic Premature mortality |
5 |
219.4172 |
26.38932 |
185.7101 |
258.5937 |
White Premature mortality |
36 |
461.0584 |
80.76389 |
289.3517 |
725.9396 |
Table 6 Premature Death and mortality as per Kentucky County Rankings Data 202010
Variable |
Obs |
Mean |
Std. Dev. |
Min |
Max |
Child Mortality Rate |
72 |
65.43214 |
19.11389 |
30.92242 |
114.8954 |
Child Mortality AIAN |
0 |
||||
Child Mortality Asian |
1 |
48.98359 |
. |
48.98359 |
48.98359 |
Child Mortality Black |
5 |
111.4401 |
43.67059 |
73.23944 |
163.4715 |
Child Mortality Hispanic |
2 |
57.4164 |
3.305798 |
55.07885 |
59.75395 |
Child Mortality White |
5 |
55.44347 |
15.37643 |
35.74641 |
73.11615 |
Table 7 Child Mortality in Kentucky and by race as per Kentucky 2020 county ranking data
Variable |
Obs |
Mean |
Sd |
Min |
Max |
Infant Mortality Rate |
30 |
7.130549 |
1.632914 |
4.685917 |
10.09009 |
Infant Mortality Rate AIAN |
0 |
||||
Infant Mortality Rate Asian |
0 |
||||
Infant Mortality Rate Black |
4 |
13.60842 |
3.569996 |
10.32702 |
18.28154 |
Infant Mortality Rate Hispanic |
2 |
5.493827 |
0.087297 |
5.432099 |
5.555556 |
Infant Mortality Rate White |
4 |
6.510473 |
2.423547 |
4.219409 |
9.651239 |
Table 8 Infant Mortality in Kentucky and by race as per Kentucky 2020 county ranking
Variable |
Obs |
Mean |
Std. Dev. |
Min |
Max |
Frequent Physical Distress (%) |
121 |
15.51022 |
1.904002 |
10.79672 |
20.97173 |
Frequent Mental Distress (%) |
121 |
15.593 |
1.586537 |
11.53725 |
19.99661 |
Adults with Diabetes (%) |
121 |
13.72231 |
3.309896 |
7.5 |
24.7 |
HIV Prevalence rate (%) |
17 |
159.9882 |
101.2132 |
35 |
431.3 |
Percent Food Insecure |
121 |
15.42479 |
2.846117 |
7.6 |
22.5 |
Limited Access to Healthy Food (%) |
118 |
4.781071 |
4.692959 |
0 |
35.17923 |
Insufficient Sleep (%) |
121 |
38.69624 |
2.263514 |
30.74122 |
45.27671 |
Disconnected Youth (%) |
40 |
10.74516 |
5.404002 |
2.111267 |
25.05285 |
Segregation index black/white |
82 |
47.60081 |
13.97617 |
18.36352 |
88.64501 |
Segregation index non-white/white |
109 |
34.5095 |
12.53157 |
5.615755 |
65.6262 |
Severe Housing Cost burden (%) |
121 |
11.31339 |
2.545547 |
6.135511 |
20.25247 |
Percent Homeowners |
121 |
71.51902 |
6.441346 |
46.90834 |
85.02012 |
Table 9 Kentucky 2020 General community profile
Variable |
Obs |
Mean |
Std. Dev. |
Min |
Max |
Median Household Income |
121 |
45279.43 |
11843.9 |
26278 |
102136 |
Median Household Income AIAN |
18 |
48146.17 |
21881.17 |
11823 |
94688 |
Median Household Income Asian |
25 |
71812.44 |
37812.8 |
21250 |
183661 |
Median Household Income Black |
76 |
34503.46 |
10919.63 |
13056 |
72045 |
Median Household Income Hispanic |
61 |
45558.28 |
21981.95 |
17431 |
133389 |
Median Household Income White |
90 |
47040.73 |
11994.28 |
25201 |
99695 |
Percent Black |
121 |
3.736202 |
4.220934 |
0.23459 |
23.83987 |
Percent AIAN |
121 |
0.329734 |
0.122453 |
0.133557 |
0.763359 |
Percent Native Hawaiian/oth PI |
121 |
0.664836 |
0.718751 |
0.052802 |
4.587701 |
Percent Hispanic |
121 |
0.067152 |
0.080369 |
0 |
0.419765 |
Percent Non-Hispanic White |
121 |
2.643442 |
1.706549 |
0.792034 |
9.988046 |
Percent Proficient in English |
121 |
0.499671 |
0.605748 |
0 |
2.852676 |
Female |
121 |
50.25458 |
1.576835 |
42.84751 |
52.86134 |
Percent Rural |
121 |
71.39901 |
27.90377 |
1.373101 |
100 |
Table 10 Median Household Income
Variable |
Obs |
Mean |
Std. Dev. |
Min |
Max |
Average # of Physically Unhealthy days |
121 |
5.032718 |
0.523298 |
3.668336 |
6.401534 |
Average # of Mentally Unhealthy days |
121 |
4.964295 |
0.396525 |
3.937529 |
5.903129 |
% Low birth Weight |
121 |
8.909034 |
1.237462 |
5.960265 |
11.95241 |
% Low birth Weight AIAN |
1 |
16.34615 |
. |
16.34615 |
16.34615 |
% Low birth Weight Asian |
9 |
8.251192 |
1.206448 |
6.27907 |
10.09464 |
% Low birth Weight Black |
37 |
16.02849 |
4.928407 |
8.333333 |
28.94737 |
% Low birth Weight Hispanic |
23 |
7.729874 |
1.442941 |
5.783582 |
11.18012 |
% Low birth Weight White |
40 |
8.281533 |
1.00553 |
6.892684 |
10.8229 |
% Smokers |
121 |
22.31011 |
2.71156 |
15.98312 |
31.8777 |
% Adults with obesity |
121 |
35.23967 |
4.242454 |
21.6 |
46.3 |
% Physically Inactive |
121 |
31.65702 |
4.721437 |
20.2 |
40.3 |
Food Environment Index |
118 |
7.373729 |
0.65456 |
4.3 |
8.6 |
% with access to exercise opportunity |
121 |
55.57868 |
25.92602 |
0 |
100 |
% Excessive drinking |
121 |
15.68306 |
1.870427 |
12.67322 |
24.16173 |
Teen Birth Rate |
120 |
41.65585 |
12.1327 |
8.728474 |
70.05189 |
Chlamydia Cases |
121 |
301.9017 |
161.2173 |
35.8 |
1056.7 |
Primary Care Physician Ratio |
0 |
||||
Mental Health Provider Ratio |
0 |
||||
Preventable hospitalizations |
121 |
6648.182 |
2497.551 |
2891 |
15420 |
Preventable hospitalization Asian |
5 |
3287.6 |
872.0601 |
2201 |
4283 |
Preventable hospitalization Black |
54 |
9072.852 |
10181.12 |
829 |
63636 |
Preventable hospitalization Hispanic |
8 |
5960.375 |
4151.787 |
1519 |
12532 |
Preventable hospitalization White |
54 |
6365.315 |
2696.022 |
3325 |
15215 |
% with annual mammogram |
121 |
36.4876 |
6.452539 |
19 |
50 |
% with annual mammogram Asian |
9 |
31.33333 |
8.558621 |
19 |
41 |
% with annual mammogram Black |
55 |
41.78182 |
10.25542 |
20 |
73 |
% with annual mammogram Hispanic |
11 |
34.45455 |
13.08712 |
20 |
61 |
% with annual mammogram White |
55 |
39.65455 |
5.686951 |
26 |
50 |
% Vaccinated |
121 |
40.99174 |
8.390963 |
14 |
55 |
Table 11 Kentucky 2020 health profile
Stakeholders of Kentucky |
Predominant ccupations in KY counties 2018 by Esri* |
Leisure and hospitality* |
Education/Health* |
Professional and Business* |
Retail and transport* |
|||||||||||||||
Construction |
Office/Admin |
Production |
Management |
Sales |
Transportation |
Employer Perspective (Derived from Economic tracker data: trackerrecovery.com) |
||||||||||||||
Role |
Building infrastructure |
Conducting processes and procedures |
Producing output demanded |
Managing the process and services demanded by KY population |
Selling the products generated to generate revenue |
Facilitate activities in and out of state |
Generate revenue/product to serve KY populations need/demand |
Educate the population, serve the healthcare needs of KY population |
Generate revenue/product to serve KY populations need/demand |
Generate revenue/product to serve KY populations need/demand |
||||||||||
Level of Interest |
Moderate given the low social association rate |
High |
||||||||||||||||||
Level of Influence |
Moderate |
High given the predominance of occupations in the state |
||||||||||||||||||
Perspective/Need |
Earn and live healthy life |
Earn and live healthy life |
Earn and live healthy life |
Earn and live healthy life |
Earn and live healthy life |
Earn and live healthy life |
Profit maximization |
Depends on their mission/vision |
Profit maximization |
Profit maximization |
||||||||||
Level of Impact of racism |
High to community of color (black more), Low to White |
|||||||||||||||||||
As described in the literature if the institution is not implementing anti-racism approach it might impacts its profits, turnovers or sustainability, absenteeism of employees, loss of creativity etc. |
||||||||||||||||||||
Entry points from the constructs of Action Framework |
1- Making Health a Shared Value for the reason as described in text |
1- Making Health a Shared Value for the reason as described in text |
||||||||||||||||||
2- Education Stakeholder- Creating Healthier, More Equitable Communities |
||||||||||||||||||||
3- Health Stakeholders- Strengthening Integration of health services and systems |
||||||||||||||||||||
What potential actions can they implement? |
1- Civil rights activities, supporting black owned business |
1- Evaluating barriers to black owned business, improving workforce diversity, talent pipeline expansion etc |
||||||||||||||||||
2- Educational Stakeholders- diversifying teaching workforce and expansion of dual enrollment |
||||||||||||||||||||
3- Health Stakeholders- Provider Patient congruence and better transportation service |
||||||||||||||||||||
Would it appeal to each stakeholder to implement proposed entry points and actions? |
Yes or Maybe given the moderate influence and interest but higher impact to black community members of KY |
Yes given higher interest, influence, and impact |
||||||||||||||||||
Table 12 Decision Maker Stakeholder Analysis Matrix to decide the level of influence and role each stakeholder play. The content is derived from Figures 3-7 in Appendix19
It is evident through our understanding of Health equity and factors affecting it in this paper that for any effort to be effective and sustainable, a multifactorial approach involving multiple stakeholders is necessary. The first step to any need assessment for implementing an effective strategy is determining the community's key stakeholders and needs. Through community profiling, once it is determined what they need, it becomes feasible to strategize the policies and actions evolving around the needs. If the needs of the stakeholders, factors impacting their needs aren’t addressed, feasibility for strategy implementation might go in vain. Utilizing the RWJF action framework after determining the community's needs, its existing status for that component affecting racism and health equity, determining key entry points of stakeholders helps us develop a sustainable solution for acting stakeholders. We are identifying the underlying cause of issue to solve it and framing the issue in the context of the needs and feasibility of the proposed actions in the RWJF action framework. The framework allows determining where the community stands in terms of each construct affecting population health, where the root causes of racism stand in terms of development or sustainability for devised actions, and the key stakeholders that could serve as implementers of proposed actions entry points. There are several limitations to this existing review including granularity of data as well as missingness of data values for some county. Future studies might want to utilize social determinants of health data from area health resource files to determine health care infrasturure in framing solutions.
None.

©2022 Patel. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.