MOJ
eISSN: 2374-6939


Case Report Volume 16 Issue 5
Department of Pediatric Orthopedics, Naval Medical Center, Mexico
Correspondence: Julio Javier Castro Salas, Department of Pediatric Orthopedics, Secretariat of the Navy - Mexican Navy, Naval University, School of Postgraduate Studies in Naval Health, Naval Medical Center, Mexico City, Tel +52 5510677925; +52 7121063378
Received: November 25, 2024 | Published: December 9, 2024
Citation: Salas JJC, Piña IN, Medel RAM, et al. Surgical management of unilateral radioulnar synostosis: a case report. MOJ Orthop Rheumatol. 2024;16(5):160-162. DOI: 10.15406/mojor.2024.16.00682
Background: Radioulnar synostosis is a rare congenital condition characterized by abnormal fusion of the radius and ulna, leading to restricted forearm rotation and limitations in daily activities. Early diagnosis and appropriate surgical intervention are crucial for improving functional outcomes, yet the optimal treatment approach remains controversial due to limited evidence. This study aims to present a unilateral proximal radioulnar synostosis case in an 8-year-old patient, detailing the surgical management and postoperative results to contribute to the existing literature on effective treatment strategies.
Case presentation: An 8-year-old patient presented with unilateral proximal radioulnar synostosis diagnosed at the age of two. The patient exhibited significant limitations in daily activities, scoring 6 points (poor) on the Failla functional scale and classified as grade III according to the Cleary and Omer radiological classification. Surgical resection of the synostosis via osteotomy was performed, followed by immobilization with a cast for six weeks. Rehabilitation commenced after cast removal, focusing on improving supination and overall limb function. The postoperative evaluation showed marked improvement, with the patient achieving 12 points (good) on the Failla scale and increased range of supination.
Conclusion: This case highlights the importance of timely diagnosis and intervention in radioulnar synostosis. Adequate physical examination and imaging studies enable early treatment, which can significantly improve the functional prognosis in affected patients. The successful outcome in this patient suggests that surgical resection combined with rehabilitation is an effective treatment modality for this rare condition.
Keywords: radioulnar synostosis, cleary and omer classification, failla scale, surgical treatment, case report, unilateral, mexico
Radioulnar synostosis is a rare condition characterized by heterotopic ossification of the interosseous membrane of the forearm, leading to blocked rotational movements and limiting basic daily activities.1 It presents in two forms: congenital, which is more common, and post-traumatic (acquired).2 This congenital anomaly results from a failure of prenatal longitudinal segmentation of the radius and ulna, resulting in a bony bridge formation around the seventh week of gestation. It may be associated with chromosomal aberrations, autosomal dominant inheritance patterns, and other congenital anomalies such as congenital hip dislocation, polydactyly, syndactyly, and urinary or cardiac tract anomalies,3 as well as syndromes like Pfeiffer, Poland, Holt-Oram,4 and Nager, where conservative treatment is often recommended.5
First described by Sandifort in 1793, radioulnar synostosis is the most common congenital elbow disorder, with an average age at diagnosis of six years. However, it can be detected from six months to 22 years.6 It is bilateral in 60% to 80% of cases, with no significant difference between males and females; only 9% have a family history, while the rest are idiopathic.7 This condition is often underestimated globally, partly because daily activities in some Eastern regions require less pronounced pronation-supination movements.8
Clinically, patients present with limited pronation-supination without pain in the early stages; pain may occur if radial head dislocation is present.3 Imaging studies, mainly bilateral anteroposterior and lateral radiographs of the forearm, are essential for diagnosis and classification, with the Cleary and Omer system describing four types of synostosis.6. Functional assessment using the Failla scale is crucial before surgical intervention.4 A Failla score of less than ten and fixed pronation greater than 55 degrees are indications for surgical treatment.9 The optimal timing of surgery is controversial; however, some authors recommend operating between 4 and 9 years of age.10
There is no consensus on the most effective surgical treatment, and while derotational osteotomy has been performed since 1992, various other procedures have been developed.11 This lack of standardized therapy highlights the need for further studies. We present the case of an 8-year-old patient with unilateral proximal radioulnar synostosis to emphasize the importance of early diagnosis and individualized surgical management in improving functional outcomes.
An 8-year-old previously healthy male was referred to our pediatric orthopedic outpatient clinic at the Naval Medical Center in Mexico due to significant limitations in left wrist mobility that interfered with his daily activities. He had been diagnosed with proximal radioulnar synostosis at the age of two.
On physical examination, the right upper limb was normal. The left upper limb exhibited complete elbow flexion with extension limited to –10°, wrist pronation of 70°, and supination of –20°. Given these findings, plain anteroposterior and lateral radiographs of the left elbow were obtained, confirming the diagnosis of radioulnar synostosis (Figure 1). According to the Cleary and Omer classification, the synostosis was grade III (severe). The patient scored 6 points on the Failla functional scale, indicating severe impairment. Based on these assessments, we decided to proceed with surgical resection of the synostosis via a posterior approach.
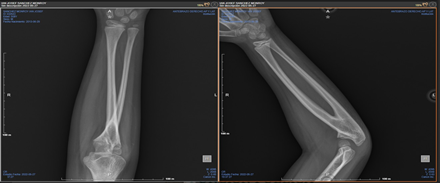
Figure 1 Preoperative anteroposterior and lateral radiographs of the right forearm.
Caption: Radiographs showing proximal radioulnar synostosis before surgical intervention.
A 5 cm incision was made over the proximal forearm. Careful dissection was performed to identify and protect the posterior interosseous nerve. An osteotomy of the radial diaphysis was conducted, followed by diaphysectomy with smoothing of the bone edges. Bone wax was applied to the osteotomy site to prevent new bone formation. Intraoperative assessment confirmed an increased range of pronation-supination. A brachio-palmar cast was used in a neutral position for six weeks (Figure 2).

Figure 2 Immediate postoperative anteroposterior and lateral radiographs of the right forearm
Caption: Radiographs demonstrating the right forearm immediately after osteotomy and resection of the synostosis.
During clinical and radiographic follow-up, the patient demonstrated significant range of motion improvement, with supination increasing to +20° and pronation maintained at +70°. The Failla scale score improved to 12 points, indicating good function. Follow-up radiographs showed no recurrence of synostosis at 12 months (Figure 3). The patient is undergoing rehabilitation therapy to maintain and enhance his range of motion.
The surgical resection of radioulnar synostosis is a subject of debate; however, this case highlights the significant functional improvement that can be achieved through early surgical intervention in patients with severe limitations. When pronation exceeds 60 degrees, surgical treatment becomes an absolute indication.5 With marked functional impairment and a Failla score of 6, our patient benefited from surgical resection, resulting in an improved range of motion and daily functioning.
Multiple treatment options have been proposed for radioulnar synostosis. Isolated resection of the synostosis often has a high recurrence rate, leading to the development of interposition techniques using artificial materials like silicone or bone wax, as well as soft tissues such as free fat grafts or vascularized tissue from muscles like the anconeus, brachioradialis, or flexor carpi ulnaris.1 Sandeep Kumar et al. (2022) noted insufficient studies to determine the most appropriate surgical technique. Options range from double-level osteotomy, as described by Sever and Gibson—which involves osteotomy of both bones through incisions along the subcutaneous border of the proximal ulna distal to the synostosis site—to the Green and Mital technique, which uses a single incision along the subcutaneous border of the ulna, and single-bone osteotomy procedures.12
Derotational osteotomy with plate fixation of the radius and ulna is another viable treatment option. It is considered safe and feasible and has a low complication rate.9,10,13 Hung et al. recommend performing the osteotomy at the level of the radius and distal to the ulnar diaphysis.11 In our case, we performed an osteotomy of the radial diaphysis with favorable outcomes, supporting the effectiveness of this approach.
A study by Fan Bai et al. evaluated patients who underwent surgery using a free vascularized fascia lata graft as an interposition material over a two-year follow-up. They concluded that this technique prevents re-ankylosis and improves forearm rotation.14. While promising, this procedure's complexity and resource requirements may limit its widespread adoption.
The optimal position after derotation osteotomy is also a topic of discussion. Some authors recommend 30 to 45 degrees of supination for bilateral cases and 10 to 20 degrees for unilateral cases.10 In our patient, we aimed for a neutral position to maximize functional use, which proved beneficial during rehabilitation.
For patients with minimal functional limitations, conservative management with occupational therapy and modifications of daily activities should be considered.2 However, given our patient's significant impairment, surgical intervention was necessary. The Failla classification system, designed by Morrey et al.,4 is reliable for evaluating preoperative and postoperative function in children over two years old and was instrumental in assessing our patient's improvement.15
Early surgical intervention is generally recommended to improve prognosis. Some authors, like Jia Y. et al., suggest delaying surgery until seven years of age to avoid epiphyseal injury and adverse effects on bone union, noting that older patients may adhere better to postoperative rehabilitation.16 However, insufficient studies evaluate surgery and follow-up in patients under six years old. Our patient's positive outcome at eight years old supports the feasibility and benefits of surgery at this age.
Radioulnar synostosis is a rare congenital condition that can significantly impair upper limb function, and its diagnosis may often be delayed due to a lack of awareness, especially at the primary care level. This case highlights the critical importance of early diagnosis through thorough physical examination and conventional radiography to facilitate prompt treatment. Individualized surgical intervention, such as resection via osteotomy, combined with dedicated rehabilitation support, can lead to substantial improvements in range of motion and quality of life, as evidenced by our patient's significant postoperative progress. While early surgical treatment is crucial for optimizing functional outcomes, ongoing long-term follow-up is essential to assess the sustained impact into adulthood and to address any future challenges that may affect the patient's quality of life over time.
We sincerely thank the patient and his parents for granting permission to publish this case study. We also thank the Pediatric Orthopedics Department of our hospital for their support and assistance in preparing this study.
None.

©2024 Salas, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.