MOJ
eISSN: 2374-6939


Short Communication Volume 16 Issue 4
1Visiting and Honored Prof., Russian Ilizarov Scientic Centre, Russia
2Bari-Ilizarov Orthopaedic Centre; PhD resident in Tashkent scientific research institute of orthopaedics and traumatology, Uzbekistan
3Prof., Bari-BariIlizarov-Ilizarov Orthopaedic Centre, Bangladesh
Correspondence: Dr. Md. Mofakhkharul Bari, Prof. Ph.D, Chief Consultant, Bari-Ilizarov Orthopaedic Centre, Visiting and Honored Prof., Russian Ilizarov Scientific Centre, Kurga, Tel +8801819211595
Received: October 11, 2024 | Published: October 21, 2024
Citation: Bari MM, Shayan RBAM, Islam S. Pelvic support osteotomy by the Ilizarov technique: a new era in orthopaedic surgery. MOJ Orthop Rheumatol. 2024;16(4):136-140. DOI: 10.15406/mojor.2024.16.00677
Hip disorders are common in orthopaedics, like joint destruction, instability, and complications from septic hips. Indications include pain, limping, and limb length discrepancies (LLD). Pelvic support osteotomy (PSO) with Ilizarov’s modification is an effective solution to achieve a stable and functional hip while addressing LLD. This procedure combines valgus and extension subtrochanteric osteotomy with distal femoral corticotomy, allowing for better mobility and actions unlike hip replacement. In a study including 122 patients with several hip conditions, we found significant improvements, with resolution of Trendelenburg gait, no LLD, and improved functional abilities.
The pelvic support osteotomy (PSO) is a useful surgical method for treating damaged hips in adolescents and young adult patients with sequelae of neonatal septic arthritis or severe hip dysplasia, which are sometimes irreducible by arthrodesis procedures or not indicated for total-hip replacement. It is a two-level femoral osteotomy designed to correct Trendelenburg gait and limb-length discrepancy secondary to hip destruction. PSO raises the pelvis on its side of osteotomy femur so to make biomechanics better during gait. To address both frontal and sagittal planes and to treat leg-length discrepancies (LLD) combined with mechanical axis deviation, Ilizarov improved upon this principle by adding a distal femoral osteotomy.1,2
Improving abductor function will decrease joint reactive forces.
|
Abductor |
Moment |
|
|
muscles |
|
|
|
arm |
|
|
|
|
|
normal varus valgus
Goal of treatment
From 1990 to 2023, we report the outcomes of Pelvic Support Osteotomy (PSO) in patients with pelvic deformities. A total of 122 patients, including 76 men and 46 women, aged from14 to 42 years old (mean age:21.4years) were included in our series. There are two osteotomies in the PSO. Proximal osteotomies position the femur in maximum adduction at a 50-40 degree angle to the pelvis. This induces an 87° angle at the knee joint between femur and tibia, aligning them perpendicular to the pelvis before performing distal osteotomy. Then you introduce an Ilizarov fixator to lengthen the femur and get it perfectly aligned. The outcome measures for this study included changes in gait mechanics, pain relief and functional mobility following surgery.2–4
How Osteotomy Works
Osteotomies improve hip function in several different ways:
Greater contact area: They improve the congruency of the joint, which enhances stability.
More of the femoral head is covered: This helps in redistributing forces across the joint.
Normal cartilage migration: By moving healthy articular cartilage into the weight-bearing zone, they promote better load distribution.
Renewal of biomechanical advantage: This helps to reduce joint reactive forces leading to restoration of biomechanical advantage thereby improving overall function.
Modulation of cartilage repair: The procedure may encourage the healing and regeneration of cartilage.
Our analysis of results in 122 patients treated with PSO between 1990-2023 showed remarkable outcomes. This study included patients with a mean age of 21.4 years, and all the satisfaction rates were similarly high. Ultimately, significant improvements in Trendelenburg gait; limb length discrepancy corrections and pain relief but not ROM.
Pelvic Support Osteotomy (PSO) is now a well-recognized modality of orthopaedic intervention in the realm of addressing unstable hips, especially for the adolescents and young adults. Traditionally, this technique was used to provide hip stability by creating a more stable pelvic lever over the femur instead of modifying mechanics at the level of contractile structures around or within the joint itself. This is particularly important and timely since younger patients have a higher risk of developing complications with more aggressive surgical techniques.
Our results mirror the established benefits of PSO already seen in this population, especially those affected by hip damage from neonatal septic arthritis or severe developmental dysplasia. This procedural bootstrapped PSO with dual osteotomies and an Ilizarov fixator for lengthening and alignment, demonstrates encouraging results. One patient in our series presented an outcome complication of sequelae, and all 122 patients showed satisfactory results with regard to Trendelenburg gait as well limb length discrepancies; thus, PSO is a safe procedure for these complaints. The fact that the procedure was shown to be mechanically effective and improves function and quality of life provides a success tale as well.4,5 When compared directly to the kind of traditional hip arthroplasty done normally, PSO does have potential benefits for younger patients. Although hip arthroplasty is an effective option for many people, it comes with a variety of possible complications (such as nerve damage, dislocations and infections) and problems with implant stability over the course of a lifetime. Since adolescents and young adults are still growing, the risks of undergoing this procedure can have long-term consequences that may outweigh any potential benefits. In contrast to this, PSO seems a safe alternative for patients with biomechanical hip instability since it effectively addresses the de-coupling of joints without increasing risk significantly.
The biomechanical principles of PSO further support its effectiveness. PSO increases the articulating surface area of the hip joint essentially increasing femoral head coverage and moving normal cartilage into a weight-bearing zone, effectively better distributing loads across that part of hip joint. This restitution of biomechanical advantage is vital in minimizing joint reactive forces and indispensable for overall hip function. Moreover, as PSO induces cartilage repair stimulation by itself, it has an advantageous bidirectional effect; addressing immediate inability to be physically functioning while potentially offering some additional restorative effects on the joint over time.
Effective preoperative assessment is the key to success in PSO. Comprehensive radiological assessment and thoughtful preoperative consideration of limb positioning are crucial to achieve the expected clinical results. With anatomical considerations ranging in complexity, every patient demands an individual and personalized approach to help ensure the benefits are maximized while complications risks reduced at a bare minimum.
In summary, our study essentially concludes that PSO has a definitive role in the surgical armamentarium for those young patients struggling with hip dysplasia secondary to previous pathologies. It may therefore be worthwhile to pursue further evaluation of PSO as an alternative treatment option for adult hip replacement, given the favorable patient benefits we encountered in our series. As the field continues to evolve with improving techniques and knowledge of long-term consequences associated with PSO, it is vital that this approach has sounded thought as one of the primary surgical approaches for a significant number patients who fit well within these criteria.1,6,7
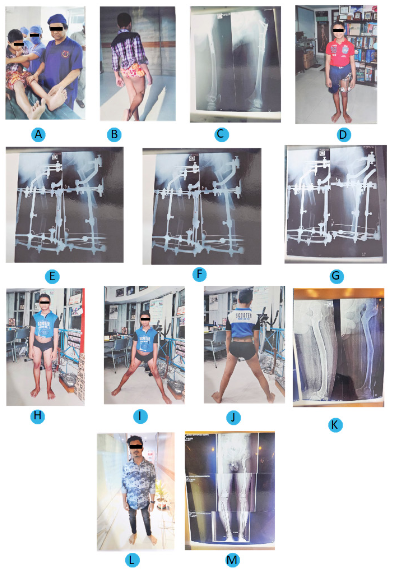
Case 1
A&B) Faild DDH with 4cm LLD, 14years old boy, Trendelenburg test positive
C)Before surgery radiograph
D)Patient with Ilizarov apparatus
E)Radiograph of patient with Ilizarov apparatus after 1 month
F)Radiograph of patient with Ilizarov apparatus after 2 months
G)Radiograph of patient with Ilizarov apparatus after 5 months
H)Clinical appearance of patient after 6 months
I & J) Abduction is normal ((Front & Back view)) Trendelenburg test negative
K)Radiographic result showing full correction after removal of frame
L)After 6 years follow up
M)Stress x-ray showing full correction
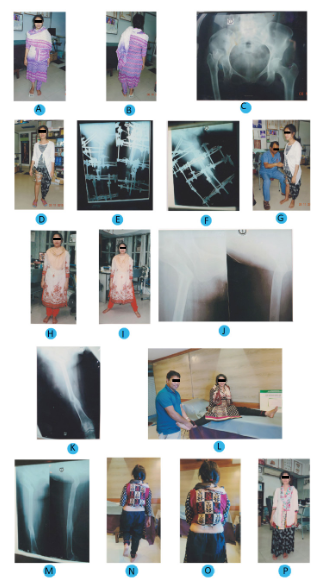
Case 2
A & B) Congenital dislocation of the hip (CDH) Rt, 25 years old girl (Front & Back view)
C)Before surgery radiograph, dislocated right hip
D)Patient with Ilizarov apparatus
E & F) Radiograph of patient with Ilizarov apparatus after 2 months
G) Doctor is checking patient’s condition and Ilizarov apparatus
H & I) Removal of the Ilizarov frame; after 4 months (Front & Back view)
J & K) Radiographic result after 5 months
L)Abduction is normal after treatment
M)X-ray showing full correction after 6 months
N, O, P) Clinical appearance of patient after 6 months, Trendelenburg gait negative
Pelvic support osteotomies greatly improve posture, walking and gait endurance among adolescents or young adults having hips damaged by neonatal sepsis all through untreated congenital dislocations. Importance of proper Preoperative evaluation, Radiographs, Limb Position for better results. Surgical intervention to correct hip instability is a promising solution that improves quality of life in patients with PSO.
None.
The authors declare that there are no conflicts of interest.

©2024 Bari, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.