MOJ
eISSN: 2374-6939


Research Article Volume 16 Issue 4
1Department of Orthopaedics and Trauma, Usmanu Danfodio University Teaching hospital, Sokoto, Nigeria
2Department of Surgery, Federal University Dutse, Jigawa, Nigeria
Correspondence: Dr. Nuradeen Altine Aliyu, Department of Orthopaedics and Trauma, Usmanu Danfodio University Teaching hospital, Sokoto, Nigeria
Received: October 01, 2024 | Published: October 17, 2024
Citation: Aliyu NA, Mohammed MM. Dynamic hip screw fixations for adult hip fractures: Our experience with 121 patients at an orthopaedic referral centre in Sokoto, North-Western Nigeria. MOJ Orthop Rheumatol. 2024;16(4):130-134. DOI: 10.15406/mojor.2024.16.00676
Introduction: Hip fracture involves fracture of the femoral neck, intertrochanteric and subtrochanteric fractures. There have been controversies in the choice for the best fixation method for the various forms of hip fractures. Among the options, dynamic hip screw (DHS) offers fast and stable fixation with acceptable complication rates. The study aimed to share our experience with using DHS as a fixation method for adult hip fractures in our centre.
Methods: This is a retrospective study of 121 adult patients who had DHS screw fixations for proximal femoral fractures from June 2015 to May 2018 at Orthopaedic Hospital Wamakko, Sokoto, North-western region of Nigeria.
Results: There were 95 (79%) males and 26 (21%) females with a mean age of 51 years (range 18 to 95 years). Right-sided fracture occurred in 67 (55%) patients and the left-sided in 54 (45%) patients. Seventy-two patients (60%) had road traffic accident (RTA), 38(31%) patients had falls, nine (7%) had sports injuries, and 2 (2%) had assaults. Seventy-two (60%) patients sustained intertrochanteric fractures, 38 (31%) femoral neck fractures, and 11 (9%) subtrochanteric fractures. The longest duration of presentation and average waiting time before surgery were 3 to 4 weeks in 11(9%) patients and 5 days respectively. Forty-three (35%) patients had open reduction and the longest surgery time was an average 2.1 hours. The average follow-up period was 2.6 years, and the subjective clinical outcomes at 6 months follow-up were 76(63%) excellent, 26 (21%) good, 11 (9%) fair, and 8 (7%) poor results. The mean Parker mobility score for the 114 patients was 6.1 before the injury and 4.3 at 1 year follow-up. Postoperative complications were 4 (3.3%) non-union, 3 (2.5%) screw cut-outs, 3 (2.5%) AVN, 3 (2.5%) Limb length discrepancy of greater than 2cm, 2 (1.7%) implant infections, 2 (1.7%) Coxa vara, and 2 (1.7%) hip osteoarthritis.
Conclusion: The use of DHS fixation devices for hip fractures in adults generally has good outcomes when appropriately indicated in patients with early presentation.
Keywords: dynamic hip screws, hip fractures, internal fixation, proximal femur fractures
Hip fracture involves fracture of the femoral neck, intertrochanteric and subtrochanteric fractures.1,2 It occurs in all ages, and the mechanism of injury largely depends on the age group affected.3 In the elderly age population, intertrochanteric hip fracture is more common following trivial falls or low-energy trauma; In the younger age group, high-energy trauma such as road traffic accidents (RTA) and falls from height are usually more common causes.3,4 The younger individuals involved in active sports do particularly sustain the femoral neck fractures.5 The proximal femoral fracture subtypes are usually classified based on the anatomical location of the fracture, fracture stability, degree of displacement and presence or absence of fracture communition.6
Most patients who sustained the fracture developed an inability to comfortably stand and bear weight on the affected limb. This may follow a simple fall on a slippery floor in the elderly with osteoporosis or following trauma in young and adult patients, and this may be associated with other fractures and regional injuries.4,7 The femoral head following neck fracture is at greater risk of avascular necrosis (AVN) and this poses a big concern to an orthopaedic surgeon given the fracture site and the age of the patient.8 For patients with intertrochanteric fractures, particularly in the elderly, prompt fixation aiming at early mobilisation is the priority. There has been controversy in the choice for the best fixation method for the various forms of hip fractures. Old and newer fixation techniques are available and still in use in different centres and by different surgeons.9 One method of fixation may not suffice to adequately address the optimal fixation requirement for the 3 fracture subtypes. Arthroplasty, especially hemiarthroplasty as an option may not be suitable in the younger active patients, so also in the elderly patients with adequate bone stock and absence of debilitating hip osteoarthritis. Thus, in this case, a total hip arthroplasty may be required. However, use of fixation methods such as cannulated screws, proximal femoral nail and plate, angled blade plate and Dynamic hip screw (DHS). DHS as a device of choice may adequately serve for the management of the aforementioned fractures because it is readily available, fast to apply, easy to handle with a speedy learning curve, and provides anatomic and stable fixation.10,11 It works on the principles of a tension band which allows the screw to slide within the barrel, thus compressing the fracture whenever the patient bears weight. In addition, it allows for early weight bearing compared to other forms of fixation devices. The study aimed to share our experience with the use of dynamic hip screw fixations for hip fractures in 121 adult patients at Orthopaedic Hospital Wamakko Sokoto in North-Western Nigeria within the 3 year study period.
This is a retrospective study of 121 adult patients who had DHS screw fixations on account of proximal femoral fractures within 3 years period (from June 2015 to May 2018). The study site was Orthopaedic Hospital Wamakko, located in Sokoto, North-western region of Nigeria. Formal ethical approval with Ref no. SMH/1580/V.IV was obtained from the Ministry of Health, Sokoto, Nigeria before embarking on the study. Patients’ records were retrieved and data was collected using a self-administered questionnaire and further information was collected during the outpatient clinic visits. The inclusion criterion was hip fractures (Cervical, Intertrochanteric and subtrochanteric) in adult patients with complete records and a minimum of 6 months follow-up. The exclusion criteria were fractures in children, open fractures, neglected fractures for more than 4 weeks, associated hip dislocation, and femoral head and acetabular fractures. There were initially 162 patients included in the study but due to incomplete records, 21 were excluded and 121 patients were included among the study subjects. The relevant demographic data, duration of fracture, injury mechanism, fracture position and type (Figure 1A & 2A), associated fractures and co-morbidities, the interval before surgery, and Parker mobility score were recorded. Descriptive statistics was employed to present our data and the outcomes of the study.
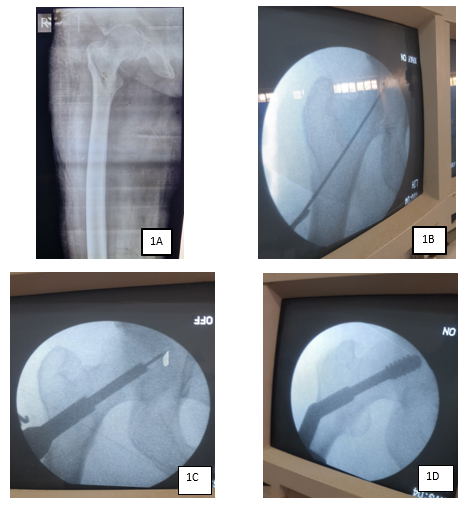
Figure 1 60 year old woman presented with 1 week history of fall, sustained right intertrochanteric fracture (1A). Intraoperative pictures showing inserted guide wire (1B), triple reaming (1C) and final DHS fixation (1D).
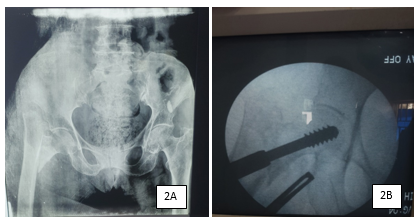
Figure 2 A) 70-year-old woman with a displaced right intertrochanteric fracture following fall 2 weeks prior to presentation. B) Intraoperative fracture reduction and fixation with DHS.
Operative procedure
The patient was positioned supine on a traction table and was given either spinal or general anaesthesia. All patients had a single injection of prophylactic 3rd generation Cephalosporin 30 minutes before skin incision as per unit protocol. The fracture was first reduced using image intensification guidance, with the use of traction and slight internal rotation. The presence of smooth medial and anterior cortical bony buttressing on the image indicates satisfactory reduction. An attempt was made to avoid varus mal-alignment of the neck-shaft angle. For patients with late presentation or fracture that could not be reduced using the closed reduction method, the fracture was reduced after opening the fracture site through a lateral approach to the proximal thigh. When the bone was reached and exposed, a guide wire was inserted parallel to the neck after making a small drilled hole which was advanced until the required position and tip-apex distance were obtained (Figure 1B). The pathway of the guide wire was drilled using a DHS triple reamer which was adjusted to the rough length of the DHS screw to be used (Figure 1C). At this stage, tapping may not be necessary, especially in osteoporotic bones. The required screw length (usually 60-95mm) was mounted on the T handle and driven to the appropriate position in the femoral head with the use of intraoperative image guidance (Figure 1D & 2B). The 1350 (4 to 8 holes) DHS side plate was fixed to the screw and a minimum of 2 cortical screws were used to hold the plate in place. Following this, the longitudinal traction was released before the final locking of the locking screw which prevents proximal fragment rotation and further reduced the fracture gap for more stability. Stability was tested by a hip range of motion followed by layered wound closure. In cases of delayed presentation and failure to achieve closed reduction, the fracture site has to be open first to release any fibrous tissue and callus to achieve desirable fracture reduction. This may cause more bleeding and prolong operation time compared to cases with early presentation.
At the immediate postoperative period, graded weight-bearing was allowed as pain was tolerated. Patients were followed up after the average 5 days of the postoperative period at 6 weeks, 12 weeks, 6 months and 1 year in the outpatient clinic. During the follow-up times, anteroposterior and lateral view radiographs of the operated areas were taken, and findings including any associated complications were noted (Figure 3). Additionally, functional outcomes were assessed and Parker's mobility scores were recorded (12). This score was assessed in all our patients both preoperatively and postoperatively and takes into account the patient’s ability to independently walk with a maximum score of 9 to the lower score with needs for support and lowest score of 0 in completely non-ambulant patients.
Table 1 shows the demography and fracture characteristics of the 121 patients in the study. There were 95 (79%) males and 26 (21%) females with the mean age of 51 years (range18 to 95 years). The right-sided fracture occurred in 67 (55%) patients and the left-sided in 54 (45%) patients. Seventy-two patients (60%) had road traffic accidents (RTA), 38(31%) patients had falls, nine (7%) had sports injuries, and 2 (2%) had assaults. Seventy-two (60%) patients sustained intertrochanteric fractures, 38 (31%) femoral neck fractures, and 11 (9%) subtrochanteric fractures. As for the fracture cause with regards to age, RTA was the cause of fracture in 78% and 82% of age ranges 18-30 and 31-50 years respectively. Fall was the cause of fracture in 62%, 97%, and 100% of age ranges 51-70, 71-90, and >90 years respectively (Table 2). Seventy (58%) male patients sustained fractures following RTA while 23 (19%) female patients aged more than 50 years had sustained fractures following fall (Table 1 and Figure 4). Table 3 summarised the duration of presentation and average time before surgery with the earliest presentation within the first 72 hours with 51 patients (42%) who had surgery within the average 26 hours interval, and the longest presentation of 3 to 4 weeks post-injury with 11(9%) patients who had surgery within the average 5 days interval (Table 3). The least average surgery time spent was 55 minutes for the patients’ group that presented within the first 72 hours of fracture, while the longest average surgery time was 2.1 hours for the patients’ group that presented 3 to 4 weeks after the fracture (Table 3). A total of Forty-three (35%) patients had open reduction with 31 (26%) patients out of the 34(28%) that presented more than 1 week of fracture had open reduction, while only 11(9%) patients out of the 87(72%) who presented less than 1 week of fracture had open reduction before the fracture fixation. The average follow-up period was 2.6 years, and the outcomes at 6 months follow-up were 76(63%) excellent, 26 (21%) good, 11 (9%) fair, and 8 (7%) poor results (Table 4). Seven (6%) patients lost to follow-up and could not be reached, and the mean Parker mobility score (Table 5) for the 114 patients was 6.1 before the injury and 4.3 at 1-year follow-up. Postoperative complications were 4 (3.3%) non-union, 3 (2.5%) screw cut-outs, 3 (2.5%) AVN, 3 (2.5%) Limb length discrepancy of greater than 2cm, 2 (1.7%) implant infections, 2 (1.7%) Coxa vara, and 2 (1.7%) hip osteoarthritis (Figure 5).
|
Variable |
Frequency (%) |
|
Age(years) |
|
|
18-30 |
21(17%) |
|
31-50 |
32(26%) |
|
51-70 |
47(39%) |
|
71-90 |
18(15%) |
|
>91 |
3(3%) |
|
Sex |
|
|
Male |
95(79%) |
|
Female |
26(21%) |
|
Sides |
|
|
Right |
62(51%) |
|
Left |
59(49%) |
|
Fracture cause |
|
|
RTA (Male 70, Female 2) |
72(60%) |
|
Fall (Male 15, Female 23) |
38(31%) |
|
Sport (Male 8, Female 1) |
9(7%) |
|
Assault (Male 2, Female 0) |
2(2%) |
|
Fracture type |
|
|
Intertrochanteric |
72(60%) |
|
Femoral neck |
38(31%) |
|
Subtrochanteric |
11(9%) |
Table 1 Demographic and fracture details (n=121)
|
Age range (years) |
Patients |
Causes of fracture |
|
18-30 |
21(17%) |
RTA (78%), Sports (15%) Assault (1%) |
|
31-50 |
32(26%) |
RTA (82%), Fall (7%) Assault (1%) |
|
51-70 |
47(39%) |
RTA (28%), Fall (62%) |
|
71-90 |
18(15%) |
Fall (97%), RTA (3%) |
|
>91 |
3(3%) |
Fall (100%) |
Table 2 Age Vs. Fracture cause
|
Patients |
Presentation time |
Average time before surgery |
Average surgery duration |
|
51(42%) |
<72hrs |
26 hours |
55mins |
|
36(30%) |
3-7 days |
2.2 days |
1.3 hrs |
|
23(19%) |
1-2 weeks |
2.8 days |
1.5hrs |
|
11(9%) |
3-4 weeks |
5 days |
2.1hrs |
Table 3 Duration of presentation, average time before surgery and surgery duration
Pre, preparation, Rx, treatment
|
Outcome |
Number (%) |
Outcomes detail |
|
Excellent |
76 (63%) |
pain-free, full ROM, No LLD, Fracture Union, No limp |
|
Good |
26 (21%) |
occasional pain, limited ROM, LLD<3cm, mild Limp |
|
Fair |
11 (9%) |
moderate pain, very limited ROM, LLD>2cm, more limp |
|
Poor |
8 (7%) |
constant pain, non-union, infected implant, OA hip |
Table 4 Outcomes at 6 months follow up
ROM, range of motion, LLD, limb length discrepancy, OA, osteoarthritis
|
Mobility all |
No difficulty |
With an aid |
With help from another person |
Not at all |
|
Able to get about the house |
3 |
2 |
1 |
0 |
|
Able to get out of the house |
3 |
2 |
1 |
0 |
|
Able to go shopping |
3 |
2 |
1 |
0 |
Table 5 Parker mobility index (12)
The treatment option for hip fractures is not limited to one type of fixation method; as many controversies still exist as to which of the fixation methods is the best for femoral neck fractures and intertrochanteric fractures particularly in relation to age, displacement, degree of bone density and associated pathology.13 Considering the anatomy and location of these fractures, more devices have been developed and the existing ones modified to optimise the outcomes of the fixation methods with a view to provide stable fixation, mobilise patients early and curtail unwanted complications accompanying the fractures and their management.14,15 Such complications include avascular necrosis, non-union, implant mal-positioning and migration, mal-union with distorted femoral neck-shaft angle, infections and in the long run, hip osteoarthritis.16 Generally, the surgical options for the treatment of proximal femoral fractures include Cannulated screws, dynamic hip screws (DHS), proximal femoral locking plate, Proximal femoral nail, Angled blade plate, and hip arthroplasties.17 Some literature strongly supported primary total hip replacement as superior to internal fixation in the treatment of mentally fit elderly patients with displaced femoral neck fractures.18,19 However, this may not be the case in the young or adult patients who the likely option for treatment in the age group will be tilted more towards internal fixation than hip replacement. Even among the elderly, good patient selection for internal fixation may offer a quick, strong and reliable fixation method which is still amenable to hip replacement as a future option following unwarranted complications.20
In this study, hip fracture was more common among the age range 51 to 70 years with 47(39%), followed by 31 to 50 years with 32(26%). This may be explained by the combined factors of RTA, fall and fragility among the older patients. The same fracture type occurring in different gender groups may result from different injury mechanisms. Predominantly, RTA was the cause of the fracture in 70 (58%) male patients meanwhile simple fall was the predominant cause in 23(19%) female patients, and this number constituted 88% of female patients in the study (Figure 3). Osteoporotic elderly women are susceptible to proximal femoral fracture especially the intertrochanteric type following trivial falls. This is the same as what has been reported by many researchers on data related to intertrochanteric fractures and elderly women.21 Although we used the DHS device on this group of patients, our selection was based on the presence of reasonable bone stock and the absence of hip osteoarthritis warranting hip arthroplasty. Subtrochanteric fractures are also amenable to surgical fixation by use of DHS device, this is usually in the form of dynamic condylar screw (DCS) fixation.22 The low number of patients with subtrochanteric fractures in our study (11/9%) was attributed to treatment of this fracture type by other fixation methods, particularly by extramedullary device as reported by Xie H et al. in their systemic review and meta-analysis of 11 studies recommended intramedullary device as treatment of choice for subtrochanteric fractures following their findings of shorter operation time, less intraoperative blood loss, shorter length of incision, length of stay and better functional outcomes in subtrochanteric fractures with intramedullary fixation than the ones with extramedullary fixations.23
Among the implant varieties currently available for internal fixation of hip fractures, DHS as an option has the advantage of being used for internal fixation of most proximal femoral fracture subtypes. It is available and has been employed over the years with various study reports on its advantages, disadvantages, device modification and recent alternatives to its use. These alternatives that include cannulated screws, angled blade plates, proximal femoral locking plates, and proximal femoral nails share both similarities and contrasting features in terms of biomechanics and approach to fracture fixation methods. In a recent study by Schuetze K et al.24 to compare the newer device femoral neck system (FNS) and the long-term established DHS system in the treatment of femoral neck fractures, they found that FNS was reliable as DHS fixation, but the only difference was risk of implant failure due to a preventable blade positioning during the procedure. Another study by Siavashi B et al.25 concluded that DHS was also found to be better than multiple cannulated screws in terms of biomechanical strength in the treatment of femoral neck fractures in young patients.25
The DHS fixation method has an average operation time of not more than 60 minutes in uncomplicated cases.26 The delay in our study from the average 60-minute operation time to a prolongation of an average of 2.1 hours in patients with an average 5 days admission days before surgery was largely attributed to and closely corresponded to delay in presentation of up to 4 weeks post-injury (Table 4). Aside from the usual preoperative preparation time, the delay in presentation usually was accompanied by patients’ comorbidities which include concomitant fractures, bed sores and joint stiffness. These added to the prolongation of preoperative time, the operation time and the postoperative complications (Figure 4). In a study by Mitchel et al. also found that delay in hip fracture surgery prolongs postoperative hospital length of stay, but did not adversely affect the postoperative outcomes.27 The delay in surgery for these patients with hip fractures especially the elderly with co-morbidities was for full optimisation before operation in the presence of bed sores, deep vein thrombosis, and urinary tract infections. Although the general guidelines for operating these patients within the recommended window period have been passed, their stabilisation helps reduce the risk of perioperative complications and improve overall postoperative outcomes. The effect of delay in operative intervention on mortality and postoperative patients’ outcomes on various hip fractures affecting different age groups remain inconclusive.28
The outcome of operative fixation can be measured by the use of certain clinical parameters to evaluate hip functions and activities of daily living (Table 5). A more valid assessment outcome measure was the use of a reliable scoring system, and in our study, we employed the Parker mobility score (12) to further evaluate the outcomes in our patients by scoring patient’s level of activities preoperatively and postoperatively at 1 year. The overall outcomes for clinical and the Parker mobility scores were generally satisfactory. Although the postoperative Parker score reduced at 1 year postoperative compared with the preoperative scores, patients were generally ambulant with or without support and this have been similar to reports by some research with overall good outcomes.11,29
Our study did not consider the use of DHS fixation devices on individual hip fracture types in a larger patient group and also compared it to other fixation devices available for surgical management of hip fractures. However, the satisfactory outcomes with fewer postoperative complications in our cases threw more on DHS as an effective fixation method. Associated pathology leading to hip fracture from trivial falls were not factored in our study despite the fact that it is a different topic for different research. This has added to the various researches available and has also stimulated more future research and investigations on the use of various surgical options in the management of hip fractures.
Our study highlighted on the use of the DHS device as a fixation technique of choice for hip fractures in adult patients with an overall satisfactory outcome. The delay in the presentation was associated with the delay in operating a patient and surgery time prolongation with a tendency to develop postoperative complications compared with an early patient’s presentation.
None.
None.
The author declares that there are no conflicts of interest

©2024 Aliyu, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.