MOJ
eISSN: 2576-4519


Clinical Paper Volume 9 Issue 1
1Department of Biomedical Engineering, Tel Aviv University, Israel
2School of Human Movement and Sport Sciences Department, Lewninskey Wingate Campus, Israel
Correspondence: Shai Greenberg, School of Human Movement and Sport Sciences Department, The Academic College Levinsky-Wingate (Wingate Campus), Netanya, Israel, Tel 97252373503
Received: May 21, 2025 | Published: June 4, 2025
Citation: Buchman A, Kazakevich E, Greenberg S, et al. In vitro analysis of stabilization forces applied through a dynamic spring ACL brace compared to a static one, examined through a range of knee tests. MOJ App Bio Biomech. 2025;9(1):51-57. DOI: 10.15406/mojabb.2025.09.00225
Introduction: Anterior circuit ligament (ACL) tears are one of the most serious injuries in sport, yet regular bracing may not reduce risk of injury. The purpose of the present study is to compare the stabilization forces applied to knee joint between a novel dynamic spring ACL brace and a traditional static one.
Methods: Nine healthy males (mean age=23.4±3.4yrs; height=1.8±0.3m; body-mass= 81.1±6.3kg) underwent two sets of seven tests, once wearing the dynamic brace and once with a traditional one. Tests included Lachman (LT); pivot shift test (PST); single-leg squat (SLS), Thessaly (TT); drop jump (DJ), crossover hop test (CH); and 90° rotational hop (RH). During all tests, force measurement sensors were placed under the brace: three under the upper femoral strap and three under the lower tibia strap. Measurements included peak changes in stabilization forces (total and posterior), knee joint internal rotation (IR) and knee joint external rotation (ER), and time-to-peak force.
Results: Total peak force was significantly higher in the dynamic brace (LT=69±5, PVT=154±8; SLS=140±8; TT=138±6; DJ=120±5; CH=136±8; and RH=128±4 g/cm2; and LT=15±3; PVT51±7; SLS14±2; TT =13±4; DJ18±4; CO=15±3; and RH16±3 g/cm2, respectively, p<0.001). And higher posterior forces measured in the dynamic brace than in the static one (LT=31±4g/cm; PS=30±2g/cm; SLS=65±6g/cm; TT=52+3; DJ=55±5; CH=50±4; RH=67±5g/cm; and LT=4.7±2; PS=5±3; SLS=3±1.8; TT=8±3; DJ=5±3; CH=7±3g/cm2, respectively, P<.001) Additionally, in some tests (IR) stabilization forces was significantly higher in the l dynamic brace than in the static one (PS=82±5; TT=44±3; DJ=39±5; CH=57±3; RH=50±6g/cm2; and PS=30±3; TT=4±1; DJ=6±3; CH=3±1; RH=4±2g/cm2, respectively, P<.001). Time-to-peak force was significantly shorter in the dynamic spring brace than in the static one for three functional tests (DJ=330±6; CH=26O±5; RH=290±5 ms) compared to the standing SLS test (77O±8 ms p<0.01).
Conclusion: These finding demonstrate that the novel dynamic ACL brace presented in this research applies greater stabilization forces than traditional static
Anterior cruciate ligament (ACL) tears are a common injury in sport, with more than 250,000 tears occurring in the United States each year.1 A 22% increase was seen from 2004 to 2014 in such injuries among young athletes aged 13–17 years.2 In most cases, reconstruction surgery is performed followed by a 9-month rehabilitation period. While about 80% of athletes who incur such injuries will return to competing at the same level as before their injury, only 50% will regain the same level of performance seen through their reduce playing time and statistics.3 Moreover, with younger athletes, about 30% will suffer from an additional tear, in the same or the ipsilateral knee – within a three-year period.4,5 The combination of the increasing rates of such injuries, the decreasing age at which they occur, the high re-injury risk, and the post-recovery performance deficit have led to increased research attention, with an emphasis on injury-prevention strategies.
One common preventive strategy is bracing. About 55–65% of orthopedic physicians from the National Football League and the National Collegiate Athletic Association recommend using braces after isolated ACL tears.6,7
Yet the biomechanical and long-term clinical effects of bracing have shown mixed results. For example, some studies show that bracing may restrict knee valgus during landing8 reduce knee-joint impact9 and improve knee-proprioception.10 On the other hand, other studies indicate that bracing increases knee rotation.11 Moreover, epidemical studies on high-school football athletes found that the prophylactic use of bracing mainly reduces medial collateral ligament injuries, not ACL ones.12,13
There are several reasons why bracing only has a limited positive effect. First, the ACL injury mechanism is a complex one that involves several planes of movement, including anterior tibia translation, and valgus and knee-joint rotation. Moreover, the tibia rotates externally yet the hip rotates internally.14 While some studies show restricted valgus and rotation,15 others present increased rotation.14 Additionally, ACL loads increase when the knee joint is flexed to about 30°, yet bracing has been found to only apply a modest degree of support during knee flexion.16 Finally, this type of injury occurs during high velocity movements, such as changing direction or landing. Video analysis studies17 show that ACL tears occur during a tibia rotation of 300mil/sec, yet a bracing support of a solid material cannot rapidly respond to restricted knee motions.18 In recent years, more dynamic braces have been developed, such as the Ossur Rebound, a dynamic brace that applies constant pressure for posteriorly pushing the tibia.19,22
In light of the disadvantages of current bracing solutions, we propose a novel bracing concept – a dynamic spring brace. This brace uses knee-flexion motions during landing or change of direction – in order to produce a force that posteriorly pulls the tibia while restricting rotation. Using such athletic motions enables the brace to generate rapid and significant stabilization force during early knee flexion.
The aim of this in vitro study is to compare the force capabilities of a proposed dynamic spring brace with those of a traditional static brace across a range of common clinical maneuvers, including knee passive stabilization tests, functional assessments, and explosive athletic performance tests.
We hypothesize that the mechanical properties of the dynamic brace will provide a significant increase in stabilization force compared to the static brace during multidirectional knee joint motion.
This study was approved by the Tel Aviv Medical Center Helsinki Committee. After receiving an explanation of the research aims and procedures, the participants signed an informed consent form. Complete confidentiality was assured.
A total of nine healthy male adults participated in this study (mean age =23.2±2.4yrs; height =1.76±0.1m; body-mass =78±3kg). The participants had no prior knee injuries, had not undergone surgery on their lower extremities, and had no musculoskeletal or neurological conditions that could inhibit their ability to perform the required physical tasks. The participants were recruited through acquaintances with the researchers.
Tests protocolThe tests were supervised by a professional sports physiotherapist with more than 15 years’ experience in the field of sports injuries. The participants were fitted with a knee brace, as per the manufacturer’s recommendations. For each physical task, they were allowed unlimited practice. Each test was repeated three times. The tests were recorded using a 2D video camera. To measure knee sagittal joint maximal flexion angle,23 two sets of the following seven tests were performed by each participant – one set for each type of brace (Table 1)
Two passive tests: (1) Lachman test (LT). The participant lay in the supine position, knee placed at about 20–30° flexion. The examiner placed one hand behind the tibia and the other on the patient’s thigh, and pulled the tibia anteriorly; and Pivot shift test (PS). The participant lay supine. The examiner applied axial and valgus force while moving the knee into flexion from an extended position.24
Two standing functional tests were also performed: (3) Single-leg squat test (SLS). The participant stood on one leg, with the other leg raised forward and flexed to approximately 90°. Arms were held straight out in front, hands clasped together. From this position, the participant was asked to squat down to about 60° knee flexion and then return to the starting position;25 and Thessaly test (TT). The participant stood on the left leg and rotated his body and knee twice, from side-to-side, internally and externally, keeping the knee flexed at 20–30°.26
Three functional dynamic landing tests were performed: (5) Drop jump (DJ). The participant stood on a 31cm high box, dropped down to the floor, and immediately performed a maximal vertical jump. The participant was instructed to maintain his arms in the “stop position,” with shoulders at 45° and elbows flexed at 90°, to reduce momentum from the arm swing;27 (6) Single-leg crossover hop test (CH). For this test, the participant stood on his left leg, perpendicular to a line that was marked on the floor. He was then asked to perform a maximal forwards-and-sideways hop over the line (as far forwards as possible), and then immediately perform an additional hop back over the starting line (again as far forwards as possible);28 and (7) Single-leg 90° rotational hop (RH). The subject stood on his left leg, with the medial side of the foot perpendicular to the direction of the hop. He then performed a maximal jump, landing on the same leg, as far ahead as possible in the direction of a standard tape measure that was placed on the floor (medial direction of the stance leg). The direction of the foot was to remain perpendicular to the hop direction at all times.28
For the latter three tests, an attempt was considered successful if the participant was able to perform the entire test while continuously standing on one leg; the CH test was considered unsuccessful if the participant touched the floor with his contra-lateral lower or upper extremities, lost balance, or needed to perform an additional short hop after the initial landing. After a failed trial, the participant was reminded of the requirement to maintain balance for at least two seconds upon landing, and was allowed to perform the test again. Between attempts of the same functional test, the participants rested for 30sec; a 2min resting period was allowed between the different types of functional tests.29 (Table 1)
|
Test |
Type |
Clinical significance |
Force direction |
Sensor numbers |
Knee joint maximal flexion angle |
|
Lachman |
Passive |
ACL |
Anterior |
3 |
20°±4 |
|
Pivot shift |
Passive |
ACL |
internal rotation |
1±2 |
80°±3 |
|
Single leg squat |
Standing functional |
ACL, meniscus |
Anterior |
3 |
80°±5 |
|
Thessaly |
Standing functional |
Meniscus |
Internal external rotation: |
1+2 4+5 |
30°±5 |
|
Drop jump |
Functional dynamic landing: vertical |
Dynamic joint stabilization |
Anterior internal rotation |
3 1+2 |
85°±6 |
|
Cross over hop test |
Functional dynamic landing: horizontal + change of direction |
Dynamic joint stabilization |
Anterior internal rotation |
3 1+2 |
45°±3 |
|
90° jump |
Functional dynamic landing: vertical rotational |
Dynamic joint stabilization |
Anterior internal rotation |
3 1+2 |
63°±5 |
Table 1 Test specifications and biomechanical variables
Each participant performed the set of seven tests twice, once wearing a commercial static-force ACL brace (ACL Everyday Knee Brace by DJO) and once wearing a non-commercial dynamic spring brace (OnCourt R Israel) (Figure 1).
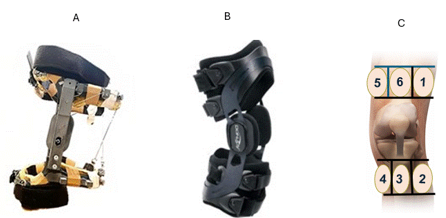
Figure 1 A: Novel dynamic spring brace used in the experiment; B: Dojo ACL brace; C: Schematic presentation of the sensors locations under both braces.
ACL dynamic brace: The novel dynamic brace has a superior strap that is attached to the athlete’s femur, and a lower strap that is attached at the level of their tibial tuberosity. The brace is also equipped with two customized springs (Nordia Springs, Israel). The spring is calibrated so that 1cm of elongation produces a tension force of 20N. Arranged in a cross shape at the posterior part of the brace, the springs are connected to two wires that pass through a pulley, arriving at the tension mechanisms that are located in the brace axis, on the lateral and medial sides. When the participant performs a knee flexion, the motion in the brace axis and in the tension mechanism that pulls the wires cause the springs to elongate. In turn, this produces a stabilization force, with the tibia being pulled posteriorly and with opposing rotation.
Sensor locations: The knee-brace pressure sampling technique30 for functional braces was applied in this study. The system, which was calibrated to the pressure of six sensors (FlexiForce A201 sensors; Antratek Electronics, the Netherlands), was 190.5mm long and 9.7mm diameter. The sensors were used to quantify the forces applied by each brace and were attached to the brace with elastic straps (Figure 1C). The upper and lower straps were divided into three zones: Zone 1, the anterior zone, which measured the posterior force. This was located at the anterior part of the femur and the tibia (8cm long and 4cm wide), with sensor no. 3 attached to the lower strap and sensor no. 6 attached to the upper strap; Zone 2, the medial joint zone, measured the stabilization force of knee joint internal rotation (IR), including the tibia external rotation and the femur internal rotation (4cm long and 4cm wide), with sensor no. 4 attached to the lower strap and sensor no. 5 attached to the upper strap; and Zone 3, the lateral joint zone, which measured the knee joint external rotation stabilization force, including the tibia internal rotation and femur external rotation (4cm long and 4cm wide), with sensor no. 2 attached to the lower strap and sensor no. 1 attached to the upper strap.
Data collection
The data was collected via the Arduino Uno WiFi Rev2 to the LabView system (National Instruments). The software presented the force overtime after initial processing (averaging). The LabView system used the force sensing resistors, as per the manufacturer’s guidelines, converting the measured resistance into the applied forces.
Statistical analysisData were analyzed using SPSS (IBM, Inc.) v.26 The following parameters were calculated and compared for each participant and test: (1) maximal force and time-to-peak force; (2) total force (TF); (3) posterior force (PF) opposing tibia anterior translation; (4) maximal knee-joint rotation force while opposing knee Internal Rotation (IR) (5) maximal knee-joint rotation force while opposing the knee External Rotation (ER)
Time-to-peak force was calculated from the time the subjects stared the test until maximal force was reached.
A paired t-test was conducted for each parameter to compare the two types of braces.
A power analysis, based on Cohen's method, was conducted to calculate the required sample size. A minimum effect size of 1.06 (Cohen's d) was used, with a target statistical power of 0.8 and a significance level of 0.05.
This chapter presents the research findings by test. Data are presented in Table 2.
|
Force |
Total |
P |
Posterior |
P |
IR |
P |
ER |
p |
||||
|
Brace type test |
d |
s |
|
d |
s |
|
d |
s |
|
d |
s |
|
|
Lachman |
69±5 |
15±4 |
<0.01 |
31±4 |
4.7±2 |
<0.02 |
20±4 |
5±4 |
NS |
18±4 |
5±4 |
NS |
|
Pivot shift |
154±8 |
51±7 |
<0.01 |
30±2 |
5±3 |
<0.01 |
82±5 |
30±2 |
<0.01 |
36±6 |
15±2 |
NS |
|
SLS |
140±8 |
14±2 |
<0.01 |
65±6 |
5±3 |
<0.01 |
39±5 |
6±3 |
<0.01 |
41±4 |
2±1 |
<0.01 |
|
Thessaly in |
96±5 |
13±4 |
<0.01 |
52±3 |
3±1 |
<0.01 |
44±3 |
5±2 |
<0.01 |
15±4 |
5±2 |
NS |
|
Thessaly ex |
99±4 |
6±2 |
<0.01 |
55±4 |
3±1 |
<0.01 |
18±4 |
3±1 |
NS |
45±4 |
3±1 |
<0.01 |
|
Drop jump |
120±5 |
18±4 |
<0.01 |
55±5 |
8±3 |
<0.01 |
39±5 |
6±3 |
<0.01 |
26±4 |
4±2 |
<0.05 |
|
CH |
136±5 |
18±3 |
<0.01 |
50±5 |
8±3 |
<0.01 |
57±6 |
5±3 |
<0.01 |
29±4 |
±36 |
NS |
|
RH |
128±4 |
16±4 |
<0.01 |
55±5 |
5±3 |
<0.01 |
50±6 |
6±4 |
<0.01 |
23±4 |
4±3 |
NS |
Table 2 Force results (gr/ cm2)
d, dynamic brace; s, static brace
Passive stabilization test: During the two passive tests the LT and PS wearing the novel dynamic spring brace resulted in a significant increase in posterior stabilization force. Significantly (p<0.01) compared to static. While during the PS test wearing the dynamic brace result significant increase (p<0.01) in IR force compared to static (Figure 2).
Functional standing tests: During the two active tests, SLS and TT. Both the total and the posterior force were significantly higher with the dynamic brace than with the static brace; (p<0.01). According to test specification the peak IR and ER force were also significantly wearing the dynamic brace compared to the static brace. In the SLS both ER and IR force were significantly increased (p<0.01). In the TT a rotational test, significantly greater stabilization force (p<0.01) was measured wearing the dynamic brace compared to the static one according to subjects maneuver direction. During the internal rotation (TTi), the IR peak force was significantly increased. During the external hip rotation maneuver (TTe), the ER force was significantly increased (Figure 3).
Explosive landing tests: Performing those three landing tests DJ, CO, RH using the dynamic brace resulted in significantly higher total and posterior peak force compared to the static brace ( p<0.01). Furthermore in accordance to test specification in the DJ both ER and IR force were significant increased (p<0.01) using the dynamic brace, compared to static brace. While in both the CO and the RH tests that induces more internal rotation movement. Wearing the dynamic brace significantly increased IR peak force compared to static brace (p<0.01) (Figure 4).
Time -to-peak force (Data are presented in Table 3).
|
|
Posterior |
IR |
||||
|
Brace type test |
d |
s |
p |
d |
s |
p |
|
PS |
770±8 |
780±30 |
NS |
750±8 |
790±20 |
NS |
|
SLS |
710±8 |
680±25 |
NS |
720±8 |
760±18 |
NS |
|
Thessaly |
550±5 |
755±24 |
NS |
520±5 |
717±10 |
NS |
|
Drop jump |
330±6 |
550±11 |
<0.01 |
270±3 |
591±12 |
<0.01 |
|
CH |
260±5 |
580±13 |
<0.01 |
170±3 |
576±9 |
<0.01 |
|
RH |
290±5 |
590±15 |
<0.01 |
130±3 |
582±11 |
<0.01 |
Table 3 Results: time to peak force (ms)
d, dynamic brace; s, static brace
Both peak posterior force and IR force (Figure 5) were significantly shorter wearing the dynamic brace compared to the static brace across all three landing tests (p < 0.01) However, no significant differences were observed between the braces during standing functional or passive tests.
The aim of this study was to examine the stabilization forces that are applied to the knee joint using a novel spring ACL brace. This dynamic aide could assist in preventing ACL tear injuries in athletes. One of the most notable findings was the high stabilization forces applied to the knee joint through the distal tibia and the proximal femur straps of the dynamic spring brace. This was the result of the higher speed and load knee-joint movements, which included rapid knee flexion and/or knee valgus/tibia and femur rotations. These movements have been found to be consistent with increased physiological ACL and meniscus loads, and increased injury risk.14 The results of this study confirmed our research hypothesis, whereby forces that are applied to the knee by the static-force brace remain constant, regardless of flexion angle and rotation. While in contract the dynamic spring brace increases stabilization force according to knee flexion angle and in response to common multi plantar knee joint motion that occurs when performing athletic activity such as landing or change in direction.
Traditional static braces are commonly used in ACL-deficient individuals and for prophylactic use6,7 despite studies showing conflicting results. For example, some studies that use cadaver models show that such braces have a restrictive effect on tibial anterior translation.18,31 This effect was also seen in in-vitro studies during passive tests.32 On the other hand, benefits of such braces have been seen in kinematic studies that analyze tibia motion during low-load/daily activities in early rehabilitation following reconstructive surgery.33–35
Additionally, examining the effect of the brace during high-load physical tasks, such as DJ or change of direction, highlights two main effects of the brace. First, it restricts the knee valgus, thereby unloading the mechanical stress on the medial collateral ligament.36 Moreover, the brace has been found to improve the individual’s subjective feeling of stabilization, through modulated muscle activity and proprioception mechanisms.37 Yet on the other hand, kinematic studies on joint functioning during dynamic tests show that the static brace has a limited stabilization effect, even increasing knee rotation11 and joint shear stress.16 These results are probably due to changes in muscle activation patterns rather than a real mechanical effect.37,38
Finally, several observational studies on athletes and army recruits show that while continuously wearing a static brace may reduce risk of injuries related to the medial collateral ligament, it has no clinically beneficial effect in preventing ACL tears or meniscus-tissue injuries.1,16
This lack of significant clinical effect emphasized the need for developing a new bracing technology, as presented in this study – to enable the applying of stabilizing forces on the knee joint during movement. This rationale has also been applied for dynamic braces such as the Rebound (by Ossur) and the spring-based brace and has led to a higher effect on protecting the knee from injury compared to the static brace, as seen in some studies20–23 yet only during daily activities and based on cadaver models. Yet in such studies, the use of dynamic braces was limited to the early stages of rehabilitation following a knee injury. This was mainly due to the relatively large size of the brace, limited range-of-motion, and the constant force applied to the knee, regardless of the knee-joint position.
Such limitations highlight the need for more dynamic braces that can be adjusted to the specific type of sports activity, especially those that entail higher risk of ACL tears and other injuries, and in individuals with deficient ACL – as a means for increasing their stabilization capability. On the other hand, the novel dynamic spring brace presented in this study has several advantages, as the spring force is only applied during flexion and it leverages the individual’s knee flexion for producing stabilization force – thereby enabling the development of a smaller, more comfortable brace. Furthermore the spring brace can produce a rapid stabilization force, that when delivered posteriorly to the tibia gives mechanical momentum for applying posterior and rotational stabilization forces. The following sections address the findings of this study based on the type of test performed: passive stabilization tests, standing functional tests, and functional dynamic landing tests.
Passive stabilization tests
Performing this type of test, where the muscles are relaxed, challenges the functioning of the ligaments and the passive stabilization of the joint.24 In ACL-deficient individuals, the static brace may restrict anterior tibia translation.32 In the present study in healthy knees, the static brace did not apply significant force, probably due to the small translation motion. With the dynamic spring brace, on the other hand, the knee was positioned 20–30° in the LT, putting tension on the spring; as a result, by anteriorly pulling the tibia, significant posterior force was applied. This indicates the prophylactic capabilities of the spring brace, as well as the potential of restricting anterior tibial translation in ACL-deficient individuals.
In the PVT, where passive knee-joint rotatory stability is challenged, the knee is tested with combined passive maximal stress, via the valgus and tibial rotation during passive knee flexion. As expected, using the spring brace in this test produced the largest stabilization force. Positioning the knee joint in an increased knee-flexion position of approximately 80°, combined with external tibia rotation, resulted in a significant increase in the stabilization forces in the posterior direction and the IR. These simultaneously increased forces in both directions indicates the multi-directional stabilization potential of the dynamic spring brace.
Functional standing tests
The two functional standing tests applied in this study were selected to measure the forces applied by the braces while performing controlled, self-paced weight bearing movements. Such tests are well established for clinically assessing the dynamic stabilization of the knee-joint and meniscus tissue, as well as overall joint functioning. The SLS test, which induces sagittal knee-joint movements with high-intensity quadricep activation, also requires good balance;25 The TT requires both active and passive rotational stabilization and balance.26 Our findings demonstrate that the static brace does not apply significant stabilization forces during the sagittal and rotational movements exhibited during the SLS and TT tests, compared to the dynamic spring. During the SLS test, a significant increase in the posterior stabilization forces was seen, compared to other tests, due to the increased knee-flexion angle of about 60° that is required when performing SLS.
During the TT, the knee-flexion angle, which was consistently at 30°, entailed less posterior force; however, here too, greater force was seen when wearing the dynamic brace compared to the static one. Moreover, when performing the knee-joint rotation, the stabilization rotatory force increased according to movement direction for the IR and the ER. The increased stabilization during the TT, with the knee at about 30° flexion – when exposed to highest mechanical loads – indicates the unloading effect of the dynamic spring brace. This is also relevant to the meniscus tissue, which is especially vulnerable during rotation movements.
Dynamic landing functional tests
The dynamic tests that were applied in the present study are widely used in the clinical field, as a means for assessing the individual’s return-to-play status. The tests require rapid and high intensity muscle activity and dynamic balance to maintain knee and body stabilization. The DJ, which is often used in motion analysis studies, mainly demands sagittal control of the knee-joint motion, while controlling the knee valgus or varus and rotation movements.28 In the present study, the dynamic spring brace exhibited significantly higher posterior forces following excessive knee flexion. Due to the nature of the DJ test, the dynamic spring brace applied significant stabilization forces in both directions, i.e., the IR and the ER; no such changes were seen in the static brace.
The CH test requires a horizontal change of direction that is similar to athletic pivoting activities. During landing, the knee joint is in a mild flexion position of about 47°, while the hip internally rotates and the tibia externally rotates – similar to ACL injury mechanisms.14 The present results indicate that the dynamic spring brace provides significantly higher posterior force and IR, as per the given knee-joint movement. This indicates a potential protective effect of the dynamic spring brace during pivoting activities. Such results were also seen in the TT.
The RH was selected, since differences in performance have been seen between individuals following reconstruction surgery, probably due to the high stability demands that this test requires.29 The test combines a knee-joint flexion of 70° and excessive internal hip-rotation movements. In the current study, the dynamic spring brace resulted in significantly higher posterior forces due to the knee flexion, and in line with the physical demands of the test, analysis of the findings also resulted in significantly higher stabilization in the IR direction.
One major limitation of existing braces is their ability to dramatically increase the forces that are applied to the knee. Video analysis shows that on average, injury trimming mechanisms are 300msec17 – thereby requiring the brace’s protective force to respond in a rapid manner. In the present study, the dynamic spring brace was found to be capable of increasing forces in relation to the physical tasks, from the passive tests to the dynamic ones. The dynamic brace was found to apply significantly higher stabilization forces when performing short functional tasks. For example, the measured posterior force was <300msec and the rotational force was about one-third shorter.
The results of this study highlight the potential protective effect of dynamic bracing systems that convert athletic motion into rapid and significant stabilizing forces. These findings support the further development the next stage of dynamic knee braces designed to activate only within high-risk flexion angles—specifically between 15° and 30° where ACL is most vulnerable. Such braces may provide joint protection without restricting the full range of motion, particularly during deep flexion phases that are critical for athletic performance and functional mobility.
This study offers important contributions to the theoretical and practical prevention of ACL-tear injuries. However, a number of research limitations should be addressed. First, the relatively small number of participants may hinder generalization capabilities of the findings – especially as they were all healthy individuals with no prior knee-joint stabilization deficits. Future research could benefit from including a larger sample, with and without ACL-deficient knees. Moreover, while the force applied by the brace was measured, related changes in knee motion were not. Future studies should therefore also measure the direct effect of the dynamic brace on the wearer’s knee rotation.
In summary, the dynamic spring brace presented in this study delivered superior stabilization force than the static one, as seen in measurements of various maneuvers and physical demands that required a range of knee-flexion angles. Moreover, as the stabilization forces were delivered in a specific direction and at specific timing, this could indicate the potential of the dynamic brace for ACL and meniscal unloading and for knee-joint injury prevention.
None.
This research project was partially or fully sponsored by (Israel innovation authority) with grant number (84323).
The authors declare that there is no conflicts of interest.

©2025 Buchman, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.