Journal of
eISSN: 2574-8114


Case Study Volume 11 Issue 4
1Healables Digital Health, Miami, FL, USA
2Healables R&D Labs, Jerusalem, Israel
3Tactical Data Group, Stafford VA; Mind Genomics Associates, Inc., White Plains, NY, USA
Correspondence: Moshe Lebowitz, Healables Digital Health, USA
Received: August 22, 2025 | Published: August 14, 2025
Citation: Lebowitz M, Halevi G, Lowell G, et al. The convergence of smart E-textiles, wearables and AI: revolutionizing sports performance, health and offering promise for PTSD. J Textile Eng Fashion Technol. 2025;11(4):187-192. DOI: 10.15406/jteft.2025.11.00421
The integration of smart electronic textiles (e-textiles) with wearable technology and AI is transforming healthcare and sports performance by enabling seamless, real-time monitoring and therapeutic interventions. The case studies brought here are meant to serve as practical examples and beacons that guide us to understanding the expanding role smart textiles will contribute as this synergistic convergence begins to generate transformational value. Smart e-textiles, which embed sensors and conductive materials into fabrics, offer enhanced comfort and functionality compared to traditional wearables. This review explores their convergence, focusing on applications in health monitoring, rehabilitation, injury prevention, and performance optimization. Innovations such as Dexmat’s Galvorn conductive yarn and Healables’ ElectroGear, which delivers microcurrent electrotherapy, exemplify the potential of these technologies. We also discuss the role of electroceuticals in managing inflammation-related conditions, including diabetic neuropathy, long-COVID, and PTSD, supported by insights from Moshe Lebowitz’s Human Brain Expo talk. Health Secretary Robert F. Kennedy Jr.’s vision for universal wearable adoption within four years underscores their societal impact. However, challenges like data privacy, regulation, reimbursement and device durability remain. This article synthesizes current research and industry developments to highlight the transformative impact generated by the synergy of smart e-textiles, wearables and AI.
Keywords: smart e-textiles, wearables, AI, health monitoring, sports performance, rehabilitation, electroceuticals, conductive yarn, microcurrent, inflammation, PTSD, MSK
CNT, carbon nanotube; EKG, electrocardiogram; EMG, electromyography; HHS, health and human services; IoT, internet of things; MSK, musculoskeletal; PTSD, post-traumatic stress disorder; ROM, range of motion; SNS, sympathetic nervous system; PNS, parasympathetic nervous system
AI-driven wearable technology has become a cornerstone of modern healthcare and sports, providing real-time data on physiological parameters such as heart rate, glucose levels, and movement patterns. The global market for wearables is projected to exceed 929 million connected devices in 2025, reflecting their widespread adoption.1 However, traditional wearables, such as smartwatches and fitness trackers, are often limited by their rigid form factor and limited coverage area. Smart electronic textiles (e-textiles), which integrate electronic components into fabrics, offer a solution by combining comfort, flexibility, and advanced functionality.
Smart e-textiles enable seamless integration into clothing, making them ideal for continuous health monitoring and therapeutic applications. For instance, they can monitor vital signs, deliver electrotherapy, or track biomechanical data, enhancing both preventive healthcare and athletic performance.
Health Secretary Robert F. Kennedy Jr. has championed the adoption of wearables, stating in July 2025, “My vision is every American is wearing a wearable within four years.” Indeed, wearables, and the regulatory environment to advance their adoption is a significant part of his “Make America Healthy Again” agenda to combat chronic diseases.2 This vision underscores the potential of wearables to empower individuals to take control of their health.
This review examines the convergence of smart e-textiles, wearables and AI, focusing on their applications in health and sports. Specifically, the role of novel materials like conductive yarns, and the promise of electroceuticals for conditions like PTSD, as discussed by Moshe Lebowitz at the Human Brain Expo 20243 serve as indications for the advancement of the smart e-textile and wearable industry. We also address challenges and future directions, drawing on recent research and industry developments from companies like Healables, Dexmat, and Wearable Tech Ventures.
Smart E-textiles: definition and technologies
Smart e-textiles are fabrics embedded with electronic components, such as sensors, actuators, and conductive materials, enabling them to interact with the environment or the wearer.4 Unlike traditional wearables, which are typically rigid devices, e-textiles are flexible, washable, and can cover large areas of the body, making them ideal for continuous monitoring and therapeutic applications.
A key enabler of smart e-textiles is the development of conductive materials, such as Dexmat’s Galvorn, a carbon nanotube (CNT) yarn optimized for conductivity and compatibility with textile manufacturing.5 Galvorn offers superior conductivity, flexibility, and durability compared to traditional conductive yarns, making it suitable for applications like wearable electrodes and sensors.6 Organizations like Wearable Tech Ventures support the development of such innovations by connecting startups with funding and industry partners, aiming to assist 100 wearable startups by 2030.7 Platforms like Fashinnovation promote the integration of technology into fashion, highlighting smart textiles as a trend that combines style and functionality.8 These advancements are driving the creation of e-textiles that can monitor health metrics, deliver therapeutic interventions, and enhance user experience.
We further see the convergence of AI and wearables at the upcoming WT | Wearable Technologies Conference 2025 USA in September 2025. This conference will bring together a highly curated group of innovators, decision-makers, and thought leaders from across wearables, AI, and digital health. Key topics include AI & the Wearable Ecosystem, Enabling the Future of Healthcare with AI and Longevity & Preventive Health Powered by AI.9
Applications in health and sports
Smart e-textiles and wearables have transformative applications in healthcare and sports, driven by their ability to collect and analyze real-time data. In healthcare, they enable continuous monitoring of vital signs, such as heart rate, blood pressure, and glucose levels, facilitating early detection of conditions like arrhythmias or diabetic neuropathy.10 For example, e-textiles with embedded electrodes can perform electrocardiograms (EKGs) or electromyography (EMG), providing non-invasive diagnostic tools.11
In sports, wearables and e-textiles enhance performance by tracking biomechanical data, such as muscle activity and movement patterns, to optimize training and prevent injuries.12 Healables’ ElectroGear, a smart textile sleeve that delivers microcurrent electrotherapy, exemplifies this application. By docking with a smartphone-controlled device, ElectroGear accelerates recovery for athletes, reducing downtime and improving performance (Figure 1).13
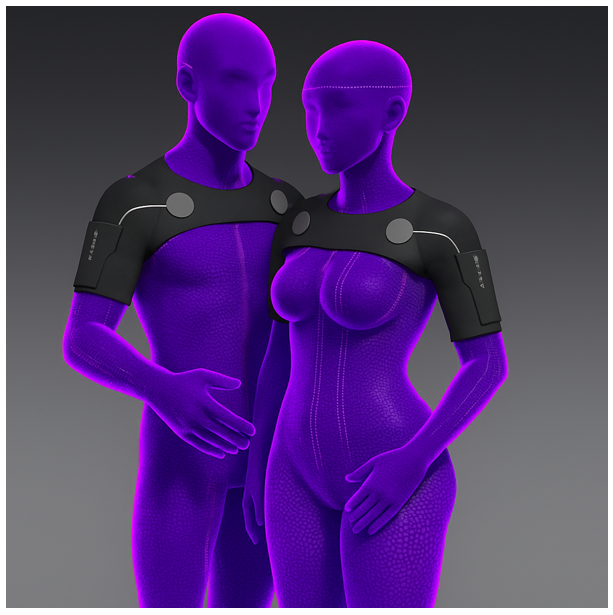
Figure 1 The Healables ElectroGear Double Shoulder Sleeve 2.0 accelerates recovery for athletes, reducing downtime and improving performance by delivering microcurrent to the shoulder through conductive elastic pathways and embedded dry electrodes.
This technology is also used in defense and digital health, supporting soldiers’ health in the field and aiding rehabilitation (Table 1).
|
S. No |
Application |
Example technology |
Results |
|
1 |
Continuous vital sign monitoring |
E-textile EKG electrodes |
Early detection of anomalies |
|
2 |
Chronic disease management |
Glucose-monitoring wearables |
Improved diabetes control |
|
3 |
Performance optimization |
Biomechanical sensors |
Enhanced training efficiency |
|
4 |
Injury prevention |
Muscle activity trackers |
Reduced injury rates |
|
5 |
Accelerated recovery |
Healables’ ElectroGear |
38% strength improvement in 24h |
Table 1 Applications of smart E-textiles and wearables in health and sports
Electroceuticals and wearable therapeutics
Electroceuticals, devices that use electrical impulses to treat medical conditions, are a promising frontier in wearable technology. When integrated into smart e-textiles, they offer non-invasive, drug-free solutions for pain relief and inflammation management.14,15 Healables for example, uses microcurrent electrotherapy to reduce inflammation and accelerate recovery, making it a leader in biohacking and sports rehabilitation (Figure 2).13
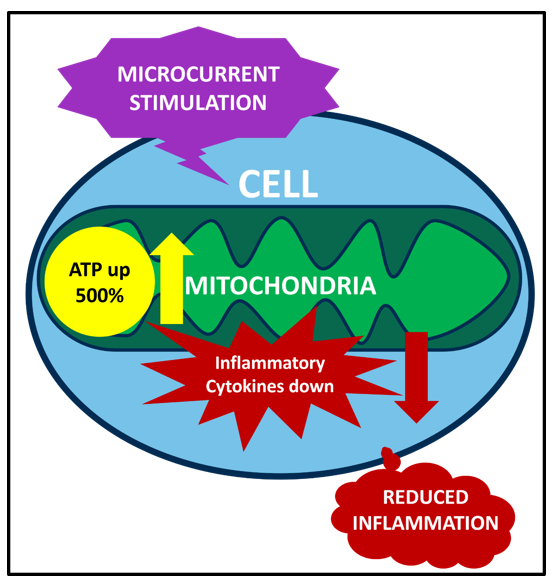
Figure 2 Microcurrent stimulation of cell membrane receptors signals mitochondria to increase ATP as much as 500% and decrease cell secretion of pro-inflammatory cytokines, resulting in reduced inflammation.
These technologies show potential in treating inflammation-related conditions, such as diabetic neuropathy, long-COVID, dry AMD and even PTSD. Moshe Lebowitz, in his Human Brain Expo talk, proposed viewing PTSD as an “autoimmune mentality” linked to vagus nerve inflammation, where microcurrent stimulation can reduce inflammatory biomarkers like interleukin-6 and C-reactive protein.3 For example, vagus nerve stimulation via wearables may alleviate PTSD symptoms by modulating the sympathetic nervous system (SNS).14 In sports, electroceuticals prevent injuries by improving blood circulation and promoting muscle recovery. In defense, they support soldier health by managing fatigue and stress in the field.16
A compelling demonstration of this convergence is a case study by Lebowitz et al.,13 presented at the 5th International Conference on Electronic Textiles (2023). The study utilized Healables’ ElectroGear e-textile sleeve to enhance a baseball pitcher’s recovery. The sleeve, composed of knitted nylon and a polyether–polyurea copolymer, features embedded dry microcurrent electrodes and a WelMetrix physiologic motion sensor.
These outcome magnitudes should be interpreted in the context of prior work on throwing-induced fatigue and recovery. A systematic review of shoulder ROM and muscle strength after pitching shows that throwing bouts can produce immediate and clinically meaningful changes in shoulder motion and function, and that strength and performance metrics commonly change in the first 30 minutes after an acute throwing episode.17
Several intervention studies and simulated-game protocols have measured shoulder strength and functional decline immediately after pitching and at 24 and 48 hours, finding measurable declines at 24 hours that sometimes persist to 48–72 hours depending on the metric and protocol used. For example, experimental simulated-game studies that re-measured pitchers at 24 and 48 hours document that passive and active recovery modalities differentially affect the speed of return of strength and ROM, with some protocols only partially restoring pre-pitch measures by 48 hours.18,19
Clinical significance and implication for pitcher availability
Taken together, the magnitude of the ElectroGear effect (≈16% improvement over baseline at 24 h vs a ≈16% decline without treatment) implies a clinically meaningful acceleration of acute recovery. Typical care trajectories often show reduced strength or ROM at 24 h with variable return toward baseline over the subsequent 48–72 h.20 Consequently, some teams deliberately schedule lower-intensity arm care or refrain from heavy throwing for 48 h. Thus, a device that (a) prevents the usual decline and (b) produces a net gain relative to baseline within 24 hours could permit earlier loading, faster progression to pitching readiness, and greater pitcher availability across short recovery windows. This conclusion is supported by work emphasizing the 24 hour window as the critical recovery period following acute pitching bouts.21,22 Furthermore, a study of baseball pitchers showed acute decreases in shoulder internal rotation in particular after an acute throwing episode. Moreover, measurable deficits lasted up to 72 h in this important functional metric.23 In fact, season-long studies of collegiate baseball pitchers have documented significant strength attrition over this time for rotator cuff/periscapular muscles. This emphasizes the need for intervention during the season such as that proposed here.24
Moshe Lebowitz’s Human Brain Expo talk highlighted a pilot study with IDF soldiers in the field, where Healables’ wearable initially failed to address musculoskeletal (MSK) issues due to undiagnosed PTSD.3 The study revealed that soldiers’ vagus nerve dysfunction, driven by chronic SNS activation, hindered MSK healing. By adjusting the protocol to include a “factory reset” microcurrent session targeting vagus nerve inflammation immediately prior to MSK treatment, 38 of 42 soldiers (90%) achieved significant pain reduction, improved range of motion, and reduced PTSD symptoms.3
The team observed that soldiers exhibiting PTSD symptoms displayed heightened tension, which inhibited the effectiveness of standard MSK healing protocols. This observation aligns with research linking PTSD to inflammation; for instance, a large-scale study found that individuals with PTSD history had a 58% higher risk of autoimmune diseases (hazard ratio = 1.56, 95% CI: 1.25–2.01), indicating a physiological underpinning.18 Moreover, PTSD patients often show elevated inflammatory biomarkers, including interleukin-1, interleukin-6, and tumor necrosis factor-α, compared to controls.19 The Healables approach leverages evidence that vagus nerve stimulation can mitigate inflammation20 and that microcurrent therapy modulates inflammatory responses by enhancing cell proliferation and cytokine regulation in fibroblast cells.21
This underscores the potential of e-textiles to address both musculoskeletal and neurological conditions. These findings highlight the benefits and possibly the necessity of addressing PTSD-related physiological states to optimize MSK therapy efficacy in military personnel.
Conventional management in combat and austere environments primarily follows protocols akin to prolonged field care: early stabilization, symptomatic NSAID use, rest, graded mobilization, and physical therapy as feasible.25 While direct comparative studies on healing timelines in deployed MSK injuries are limited, a systematic review of MSK pain interventions in serving military personnel reports generally modest improvements even with structured conservative care, and considerable variability in time to functional recovery depending on injury severity and treatment access.26 In field settings, delays in definitive rehabilitation and limitations in follow-up contribute to extended recovery timelines—often measured in weeks rather than days.
For PTSD, the Department of Defense and Veterans Affairs recommend trauma-focused cognitive-behavioral therapies—primarily Cognitive Processing Therapy (CPT) and Prolonged Exposure (PE)—as first-line treatments.27 Meta-analyses reveal that CPT and PE yield large within-group effect sizes (Cohen’s d ≈ 0.78–1.10) with clinically meaningful symptom reduction in approximately 49–70% of treated military personnel; however, a significant proportion (≈60–72%) continue to meet PTSD diagnostic criteria post-treatment, and dropout rates are high.28 A Cochrane-aligned systematic review reinforces that individual CBT–TF offers the strongest evidence, but notes reduced efficacy and higher dropout rates in military versus civilian populations; group formats are less effective, and therapies such as EMDR lack sufficient support.29 Treatment durations commonly span 8–12 weeks, with sustained symptom improvement up to six months but diminishing effects at 12 months.30
Comparative analysis: Healables vs. Standard field care31
The Healables protocol addresses two critical shortcomings of existing care approaches: (1) delayed or incomplete recovery in MSK injuries, especially under field limitations; and (2) lower-than-desired efficacy of standard PTSD therapies, particularly in comorbid, active-duty populations.32 By integrating autonomic modulation via vagus-targeted microcurrent prior to MSK therapy, the wearable appears to create a neurophysiological precondition that substantially enhances both physical and psychological recovery within an accelerated (24-hour) timeframe (Table 2).33
|
Aspect |
MSK field care standard of care |
PTSD field care standard of care |
Healables wearable outcome |
|
Time to improvement |
Weeks–months, variable |
8–12 weeks for symptom reduction; partial remission rates |
Observable within 24 hours; 90% of participants improved |
|
Approach focus |
Structural and symptomatic only |
Psychological/trauma-centered, not integrated with MSK treatment |
Simultaneous modulation of autonomic (vagal) and MSK pathways |
|
Efficacy in comorbid cases |
Poor when PTSD present |
Modest efficacy; many remain symptomatic post-treatment |
High combined efficacy in MSK and PTSD symptoms |
Table 2 The Healables wearable e-textile shows promise for comorbid MSK and PTSD cases in the field when compared with the standard MSK and PTSD field care
These results suggest a synergistic advantage of the Healables e-textile intervention over conventional field care: rapid, high-rate functional improvement in both MSK and PTSD domains, where existing therapies individually provide slower or less complete recovery.34 If replicated in controlled trials, this approach could revolutionize acute rehabilitation strategies in military medicine, especially under prolonged field-care constraints.35
AI enhanced by smart textiles
The convergence of artificial intelligence (AI), predictive analytics, and mind genomics holds transformative potential for healthcare, particularly when underpinned by high-quality, reliable health data. Research demonstrates that AI excels at interpreting complex health data for predictive analytics, identifying patterns and forecasting outcomes with remarkable accuracy—yet this capability hinges on consistent and robust input data.22,23
Smart textiles address this need by providing an innovative platform for continuous, real-time monitoring of bioinformatics and physiological data, capturing nuanced changes in health status.24,26 This uninterrupted data stream significantly enhances AI’s predictive power, enabling more precise detection of anomalies and supporting mind genomics approaches that map individual cognitive and physiological responses.27,29
Moreover, smart textiles can integrate closed-loop bioelectric neurostimulation, allowing AI-driven insights to trigger automated, real-time interventions—creating a seamless ecosystem for monitoring and treatment.28,32 This synergy not only redefines continuous health monitoring but also ushers in a paradigm of personalized, proactive therapeutics tailored to individual needs.
The case studies highlight the transformative potential of smart e-textiles and wearables. However, challenges persist:
Initiatives like Fashinnovation and Wearable Tech Ventures are pivotal in fostering innovation, while Lebowitz’s work suggests bioelectric medicine could reduce reliance on pharmaceuticals.3,7,8 Continued research and collaboration are essential to overcome these hurdles.
Future research should explore large scale double-blind randomized controlled trials for sports performance and medical inflammatory conditions. Because therapeutic microcurrent is subsensory, it is well suited for both therapeutic and sham treatment in these trials. Additionally, the connected and continuous data features of smart e-textiles allow for accurate and cost-effective data integrity in multi-site clinical trials. As such, the synergy of therapeutic microcurrent delivered through smart e-textiles should be explored for long-covid, PTSD, fibromyalgia, dry macular degeneration, diabetic neuropathy and sports injuries.36–48
The integration of smart e-textiles, wearables and AI heralds a new era in health and sports technology. By offering comfortable, functional solutions, they enable continuous monitoring, personalized therapy, and enhanced performance. The ElectroGear sports and Healables PTSD pilot studies illustrate their potential in sports performance and recovery as well as musculoskeletal and neurological health. RFK’s vision of a wearable future signals ubiquitous adoption and provides confidence and optimism that the industry will see technical and regulatory transformations to unlock the full impact of the convergence of smart e-textiles, wearables and AI.
We acknowledge the pioneering work of Moshe Lebowitz, Michael April, Howard Moskowitz, Healables, Dexmat, and Wearable Tech Ventures in advancing smart e-textiles and wearables.
None.
The authors declare that the e-textiles and wearable microcurrent research, case studies and pilot studies referenced in this paper of the Healables and ElectroGear products were sponsored by Healables.

©2025 Lebowitz, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.