Journal of
eISSN: 2373-6410


Mini Review Volume 15 Issue 3
1Clinical Fellow in Neurosurgery, Royal Infirmary of Edinburgh, Department of Clinical Neurosciences, UK 2
2Senior Consultant Neurosurgeon, Clinical Director NeuroKonsilia Inc., Spain
Correspondence: Juan F Martínez-Canca, Senior Consultant Neurosurgeon, Clinical Director NeuroKonsilia Inc., Spain,
Received: July 10, 2025 | Published: July 25, 2025
Citation: Martínez-Soler P, Martínez-Canca JF. Laminectomy and spinal stability: a biomechanical rebuttal to patient alarmism. J Neurol Stroke. 2025;15(3):66-70. DOI: 10.15406/jnsk.2025.15.00625
In contemporary clinical practice, there persists a troubling tendency among certain orthopaedic surgeons to incite fear regarding alleged “post-laminectomy instability.” This narrative, often unfounded, has led to a pathologization of operated anatomy and the overindication of unnecessary spinal fusions. The implications of such a trend are multifaceted: patients may be subjected to more invasive procedures than necessary, spinal biomechanics may be compromised long-term, and healthcare resources may be allocated inefficiently. This article offers a critical review of the alarmist perspective, contrasting it with the biomechanical principles established by Francis Denis and other authoritative voices. It delves into the anatomy and function of spinal columns, analyses the real impact of Laminectomy on structural integrity, and addresses the nuanced, often underexplored, issue of spinal fusion overuse. Through an evidence-based, clinically grounded approach, the work aims to promote a more balanced and discerning view of spine surgery indications, advocating for responsible, individualized decision-making over reflexive instrumentation.
For decades, Laminectomy has held a central role in the surgical management of spinal pathologies, particularly in patients suffering from spinal canal stenosis, compressive myelopathy, or radiculopathy (Figure 1).1
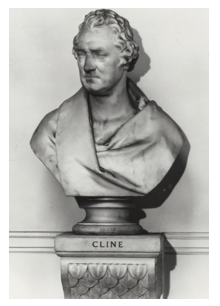
Figure 1 British surgeon Henry Cline performed the first well-publicized Laminectomy in 1814, though the patient died shortly after. American surgeon Alban G. Smith is credited with the first successful Laminectomy in 1828 (no reliable portrait is available).
As a decompressive procedure, it is designed to relieve pressure on the neural elements by removing non-load-bearing posterior structures - typically the laminae and ligamentum flavum.1 The technique is time-tested, widely practiced, and often yields excellent symptomatic relief.
Despite its established role, a growing number of patients find themselves at the receiving end of cautionary tales following Laminectomy. They are told that their spine has become "unstable," that their vertebral column can no longer support physiological loads adequately, and that without immediate fusion - with pedicle screws, rods, cages, and sometimes bone grafts - they risk collapse, deformity, or neurologic deterioration. The psychological and clinical weight of such a warning can be profound, often driving patients toward complex instrumentation procedures they neither expected nor fully understand.
The roots of this alarmist view are multifactorial. Some arise from an overextension of the concept of spinal stability, often conflated with mere anatomical modification. Others stem from a reluctance to differentiate between structural change and functional compromise. Moreover, the perceived instability is frequently not supported by objective criteria - such as imaging-based dynamic movement or confirmed mechanical failure - but instead inferred from surgical doctrine or anecdotal precedent.
This paper challenges that paradigm. It seeks to rigorously examine whether the concerns surrounding post-laminectomy instability are justified through the lens of established spinal biomechanics and clinical evidence. In doing so, it posits a categorical answer: no, routine Laminectomy does not inherently destabilize the spine. Rather, the concern over spinal instability appears, in many instances, to be disproportionately emphasized - rooted more in prevailing surgical paradigms and market-driven incentives than in robust empirical evidence.2,3
In 1983, American Orthopaedic Surgeon Francis Denis, MD introduced a landmark conceptual framework that reshaped the understanding of spinal stability: the three-column model.4 This biomechanical theory offered a pragmatic and anatomically grounded tool for evaluating the structural integrity of the spine, particularly in the thoracolumbar region - a common site for traumatic injury and degenerative disease (Figure 2).
Denis proposed that the spinal column is not a monolithic structure but rather a coordinated system of three longitudinal columns, each with distinct biomechanical roles:
Crucially, Denis asserted that spinal stability is preserved when at least two of these three columns remain structurally intact.4 A lesion or intervention that affects only a single column - most notably the posterior one - does not, by itself, confer clinical or mechanical instability.
This model represented a critical evolution from previous dichotomous models (such as Holdsworth’s two-column concept),5 by recognizing the central role of the middle column and offering a more detailed appreciation of how traumatic or iatrogenic disruptions might influence load distribution and kinematic control.
Its relevance to modern surgical practice, particularly in the context of Laminectomy, cannot be overstated. Standard decompressive Laminectomy typically involves removal of elements limited to the posterior column - the laminae and ligamentum flavum - while leaving the vertebral bodies, intervertebral discs, longitudinal ligaments, and often the facet joints completely intact.1,6
Accordingly, when performed thoughtfully, Laminectomy does not breach the integrity of the middle or anterior columns and thus does not meet the biomechanical threshold for segmental instability.7 The continued invocation of post-laminectomy instability in such cases, therefore, stands on shaky theoretical ground - if not outright contradiction of Denis' biomechanical principles.
In other words, a proper decompressive technique involves the removal of parts of the laminae and ligamentum flavum:
Instability does not automatically arise unless the procedure includes extensive bilateral facet joint resection or coexists with significant preexisting degenerative changes.8–10
More than forty years after its introduction, Denis’ model remains an indispensable lens through which spinal integrity should be interpreted - not only in trauma, but also in the realm of decompressive and reconstructive surgery. It provides a shield against hasty generalizations and encourages clinicians to pursue stability not as a reflexive dogma, but as a scientifically defined condition.4,7
Within contemporary spine surgery discourse, the term “instability” has undergone a regrettable semantic inflation - its precision diluted, its scope overstated, and its implications often misunderstood.2,11 This distortion is not merely academic: it has real consequences for clinical decision-making, patient outcomes, and the ethical stewardship of surgical intervention.
It is increasingly evident that many practitioners - whether through inadvertent imprecision or strategic convenience - conflate three distinct concepts under the same linguistic umbrella:
By collapsing these categories into a single, emotionally charged label - “instability” - the surgical narrative gains a powerful rhetorical tool: one that justifies more aggressive interventions, pre-emptive fusions, and even prophylactic instrumentation.2,16 But this rhetorical power is achieved at the expense of anatomical truth and biomechanical rigor.
Such linguistic imprecision, whether borne of habit, pedagogical inertia, or commercial incentives, contributes directly to the overindication of spinal fusion procedures - interventions that are neither benign nor universally appropriate.11,17 Instrumented fusion is a procedure with well-documented risks: adjacent segment disease, hardware failure, loss of spinal mobility, and substantial postoperative morbidity, among others.8,18 To offer it based on fear rather than fact is to fail the very essence of evidence-based medicine.
It is particularly paradoxical - and academically disheartening - that this conceptual erosion is often perpetuated by professionals within traumatology, a discipline that owes much to the foundational work of Francis Denis himself.4 That the intellectual legacy of a surgeon who meticulously defined the biomechanical parameters of stability should now be misappropriated to justify unwarranted fusion betrays not only a lapse in critical thinking, but a subtle disrespect for the very principles upon which modern spine biomechanics were built.
One might reasonably suggest that some of these colleagues - especially those who invoke “instability” with such theatrical certainty - might benefit from a return to first principles, revisiting the anatomical and functional criteria set forth by Denis.4,7 The spine, after all, is not a static scaffold to be locked down at the first sign of degeneration; it is a dynamic, load-sharing structure, evolved for motion, not immobilization.19
This is not a condemnation of spinal fusion per se - when truly indicated, it remains a cornerstone of spinal reconstructive surgery.9,20 But the distinction between necessity and convenience, between precision and presumption, must be vigilantly preserved.
In the current climate, where patients are increasingly informed, and where clinical ethics demand ever higher standards of justification, the burden lies with the surgeon to ensure that terms like "instability" are not wielded as incantations of fear, but as scientific diagnoses grounded in demonstrable pathology.2,3
In recent years, there has been a steady and disquieting rise in the number of spinal fusion procedures being recommended and performed - many of which, upon rigorous examination, fall short of the stringent clinical thresholds that once defined the necessity of such an intervention.11,16 Fusion, while undeniably valuable and at times indispensable in cases of demonstrable mechanical instability (such as in spondylolisthesis with slippage, gross segmental hypermobility, or spinal deformity correction), is increasingly being applied in settings where the evidence of benefit is ambiguous or entirely absent (Figure 5).20–22
This phenomenon reflects more than individual error or preference - it suggests a deeper cultural drift within segments of the surgical community. A convergence of systemic, educational, and financial influences may be at play. Chief among them:
Compounding this trend is a growing tendency to conflate anatomical alteration with mechanical failure. The mere presence of disc degeneration, facet hypertrophy, or radiological asymmetry is too often misread as harbinger of collapse, when in fact these features may be long-standing and clinically irrelevant.8,25 Consequently, fusion is sometimes proposed prophylactically - just in case - a rationale that belongs more to pre-emptive myth than to scientific medicine.2,11
It must also be underscored that spinal fusion is far from a benign or neutral intervention. The downstream consequences of segmental fixation are well documented, and include:
Thus, the casual or uncritical expansion of fusion indications carries more than biomechanical consequences - it entails ethical ones. Surgery should never be dictated by fear, habit, or financial gravity. It must be predicated upon individualized assessment, verifiable dysfunction, and judicious restraint.16,21
This is not a condemnation of fusion, nor a call for therapeutic nihilism. On the contrary - it is a plea for surgical sophistication. Spinal fusion, when warranted, can be life-altering. When unwarranted, it can be life-altering too - but for the worse.29
As stewards of spinal integrity, we are obliged to distinguish between what can be fused and what must be fused. The scalpel, like the pen, must serve reason - not reflex.2,20
Multiple studies have demonstrated that:
Challenging vertebral alarmism
Laminectomy is neither a biomechanical sentence nor an open door to catastrophic instability.1,6 It is, when correctly indicated and artfully executed, a conservative act of liberation - a technical expression of anatomical reverence aimed at relieving compression while preserving form and function.9 Yet, in some circles, it has been misrepresented as an incomplete gesture, a compromised intervention, or worse: a liability waiting to manifest failure.
This distortion has not emerged from new evidence or improved understanding, but from a troubling alliance of outdated dogma and economic expediency.3,11 In such environments, fear becomes a tool - instability a mantra - and fusion, a foregone conclusion. The result is a culture that conflates surgical intervention with hardware deployment and treats any uninstrumented spine as inadequately treated.16,18
But let us be unequivocal: the anatomical truth of the spine does not bow to financial models, nor should it be silenced by surgical orthodoxy.7,11 To preserve motion, to respect the biomechanical wisdom of evolution, and to favour less invasive approaches where possible - this is not radicalism. It is clinical integrity.13,24
The call to reclaim Laminectomy’s rightful place is not a nostalgic retreat to simpler times, but a demand for rationality in an age of excess. It is a defence of spinal physiology against the creeping pathologization of normal anatomy. It is an appeal to intellectual courage, to question the reflexive fusion, and to remember that restraint is not weakness, but wisdom.14,21
We must do more than operate - we must interpret. We must weigh not only what we can do, but what we should do. And in doing so, we must reject the theatrical warnings of collapse that haunt patients into accepting hardware they may never have needed.2,20
Let us restore balance - not only to the spine, but to the conversation. Let us speak the language of biomechanics, not the dialect of fear.4,7
In the end, the spine is not a battlefield to be fortified - it is a structure to be understood. And the patient is not a vessel for implants - but a human being, seeking clarity, dignity, and healing.
None.
The authors declare that there are no conflicts of interest.

©2025 Martínez-Soler, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.