Journal of
eISSN: 2374-6947


Review Article Volume 12 Issue 1
1Department of Internal Medicine, Hind Institute of Medical Sciences, India
10Department of Internal Medicine, Shri Tulasigirish Cardiodiabetes Hospital & Diabetes Research Foundation, India
11Department of Internal Medicine, Jothydev’s Diabetes Research Centers, India
12Department of Internal Medicine, Diabetes Care & Hormone Clinic, India
13Department of Internal Medicine, Trichy Diabetes Speciality Centre (P) Ltd, India
14Department of Food and Nutrition, The Maharaja Sayajirao University of Baroda, India
15Department of Internal Medicine, Advanced Center for Diabetes, Thyroid and Obesity, India
2Department of Internal Medicine, M.V. Hospital for Diabetes, India
3Department of Internal Medicine, Aegle Clinic, India
4Department of Internal Medicine, Centre for Diabetes Care, India
5Department of Physiology, King George’s Medical University, India
6Department of Internal Medicine, Jai Clinic and Diabetes Care Centre, India
7Department of Internal Medicine, Diabetes Wellness Care, India
8Department of Internal Medicine, Omnia Hospital, India
9Department of Internal Medicine, Diabetes and Wellness Clinic, India
Correspondence: Anuj Maheshwari, Professor, Department of Internal Medicine, Hind Institute of Medical Sciences, Ataria, Sitapur Road, N Lucknow, Uttar Pradesh, India
Received: June 02, 2025 | Published: June 18, 2025
Citation: Maheshwari A, ViswanathanV, Sanjay A, et al. Diabetes care in rural India – review. J Diabetes Metab Disord Control. 2025;12(1):42-47. DOI: 10.15406/jdmdc.2025.12.00295
Type 2 Diabetes Mellitus (T2DM) is a growing public health crisis globally, with rural India experiencing a significant increase in prevalence due to urbanization, lifestyle changes, and limited healthcare access. This review highlights the multifaceted challenges of T2DM management in rural India, including inadequate awareness, delayed diagnosis, and suboptimal treatment adherence. Factors such as genetic predisposition, socio-economic barriers, and cultural beliefs exacerbate the burden while resource constraints in rural healthcare systems hinder effective disease management. Innovations like mobile health technologies, government initiatives, and community-based education programs have shown promise in bridging healthcare gaps. This paper also emphasizes the critical role of structured diabetes education, affordable medication access, and culturally sensitive interventions in improving glycemic control and preventing complications. Strengthening primary healthcare infrastructure, fostering public-private partnerships, and integrating traditional and allopathic medicine are identified as essential strategies to address this pressing health issue. The findings call for comprehensive policies that prioritize early detection, lifestyle modifications, and equitable healthcare delivery to mitigate the rising diabetes burden in Indi’s underserved areas.
Keywords: Type 2 diabetes mellitus (T2DM), rural healthcare, diabetes management, healthcare access, public health interventions
Diabetes is a significant global health issue, arising from persistently elevated blood glucose levels.1 It is spreading rapidly in India, a country predominantly inhabited by a rural population. Rapid urbanization has led to a marked decline in the rural population—from 82% in 1960 to 64% in 2023—but India still remains home to a substantial rural community.2 Rapid urbanization, the influence of mass media, reduced physical activity, and changing dietary patterns have significantly altered lifestyle patterns among India's rural population.3 As a result, the gap in diabetes prevalence between rural and urban areas is steadily narrowing. Around 90% of diabetes cases are attributed to T2DM, which involves both insulin resistance and inadequate insulin production by the pancreatic islet β cells, leading to high blood sugar levels. Insulin resistance in T2DM is commonly associated with obesity, sedentary lifestyle, and aging.1,4 Persistent insulin resistance in T2DM can lead to various complications, including large blood vessel problems like atherosclerosis and small blood vessel issues such as kidney disease, nerve damage, and vision problems.5 Asia, with its large population and fast economic growth, has become a key area of focus, where individuals are developing diabetes at younger ages and with lower BMIs. Factors contributing to this include the "metabolically obese" phenotype, high levels of smoking and alcohol consumption, a diet rich in refined carbohydrates, and reduced physical activity.6 Early malnutrition, followed by later over nutrition, also plays a role. While genetics offer some understanding, they don't fully account for ethnic differences in diabetes risk. Although lifestyle changes can help prevent the condition, addressing the growing epidemic requires significant public policy changes, particularly in promoting healthier diets and increased physical activity.7
Risk factors for T2DM in rural India
Importance of addressing diabetes in rural India
Managing chronic diseases like diabetes presents significant challenges, mainly due to the need for ongoing adherence to treatment and the prevention or management of related complications. This requires consistent engagement from healthcare systems throughout the continuum of care. Diabetes care demands coordination across all levels of healthcare, with a crucial role played by the patient’s knowledge, attitudes, and commitment to treatment and adherence. Diabetes self-care refers to the actions individuals with, or at risk of, diabetes take to manage the disease independently. Effective self-care is complex and requires a comprehensive approach involving healthy eating, regular physical activity, frequent blood sugar monitoring, medication adherence, problem-solving skills, healthy coping strategies, and behaviors that reduce risk. These actions are essential for achieving optimal glycemic control and avoiding future complications.
Rising prevalence of diabetes in rural India
According to the Indian Council of Medical Research–India Diabetes (ICMR–INDIAB) study, the prevalence of diabetes in India has reached 101 million individuals (approximately 57.3 million in rural India).9 Diabetes is no longer confined to urban populations in India. Recent studies indicate a rapid increase in diabetes prevalence in rural India, narrowing the gap with urban areas. According to the ICMR-INDIAB study (2023), the overall diabetes prevalence in India is 11.4%, with urban areas having a higher burden (17.2%), but rural areas catching up at 9.4%.9 The Ranasinghe et al.,17 systematic review also highlights that diabetes prevalence in rural India increased from 2.4% in 1972 to 15% in 2019 (Figure 1).17 This sharp rise is primarily driven by urbanization, lifestyle changes, increased consumption of processed foods, and reduced physical activity.
The highest diabetes prevalence is observed in the southern and northern states, while the central and northeastern regions have relatively lower prevalence rates. This regional disparity highlights the need for region-specific diabetes interventions considering economic development, healthcare infrastructure, and local dietary patterns (Table 1).9 Recently released ICMR-INDIAB results from Jammu and Kashmir reported a prevalence of 26.5% in urban areas and 14.5% in rural areas.18
|
Prediabetes |
Diabetes |
||||
|
Prevalence |
Rural |
Urban |
Prevalence |
Rural |
Urban |
|
≥ 15% |
Himachal Pradesh, Delhi, Haryana, Chandigarh, Rajasthan, Madhya Pradesh, Chhattisgarh, Uttar Pradesh, West Bengal, Sikkim, Tripura, Kerala, Puducherry, Goa |
Himachal Pradesh, Delhi, Haryana, Chandigarh, Rajasthan, Madhya Pradesh, Chhattisgarh, Odisha, Bihar, Uttar Pradesh, West Bengal, Sikkim, Tripura, Kerala, Karnataka Puducherry, Goa |
≥ 10% |
Himachal Pradesh, Punjab, Delhi, Chandigarh, Bihar, West Bengal, Goa, Kerala, Puducherry |
Himachal Pradesh, Delhi, Punjab, Haryana, Chandigarh, Uttarakhand, Rajasthan, Madhya Pradesh, Chhattisgarh, Odisha, Bihar, Jharkhand, West Bengal, Sikkim, Meghalaya, Assam, Nagaland, Mizoram, Tripura, Kerala, Karnataka Puducherry, Goa, Telangana, Andhra Pradesh, Tamil Nadu, Maharashtra, Gujarat |
|
10-14.9% |
Uttarakhand, Bihar, Arunachal Pradesh, Assam, Meghalaya, Odisha, Telangana, Karnataka, Maharashtra, Gujarat |
Uttarakhand, Jharkhand, Arunachal Pradesh, Assam, Nagaland Telangana, Andhra Pradesh, Maharashtra, Tamil Nadu |
7.5-9.9% |
Uttarakhand, Haryana, Tripura, Odisha, Chhattisgarh, Maharashtra, Tamil Nadu |
Uttar Pradesh, Manipur |
|
5.0-9.9% |
Punjab, Jharkhand, Manipur, Mizoram, Nagaland, Andhra Pradesh, Tamil Nadu |
Punjab, Gujarat, Meghalaya, Manipur, Mizoram |
5.0-7.4% |
Gujarat, Arunachal Pradesh, Assam, Andhra Pradesh, Telangana, Karnataka |
Arunachal Pradesh |
|
0-4.9% |
- |
- |
0-4.9% |
Rajasthan, Uttar Pradesh, Madhya Pradesh, Jharkhand, Bihar, Meghalaya, Manipur, Nagaland, Mizoram |
- |
Table 1 Regional variations of diabetes in rural India9
High burden of undiagnosed diabetes and poor control
A major challenge in rural diabetes care is the high proportion of undiagnosed cases and poor glycemic control. The SMART India study (2023) found that 36.7% of rural individuals with diabetes remain undiagnosed, compared to 22.8% in urban areas.19 The National Family Health Survey (NFHS-5) reported that only 7% of individuals with diabetes in India have their condition under control, with rural populations having even lower treatment and control rates.14 This lack of diagnosis and control increases the risk of complications such as cardiovascular disease, kidney failure, neuropathy, and blindness, imposing a significant economic and health burden on rural families. A study by Rai et al.,20 in Karnataka reported that individuals residing in rural areas had 2.30 times higher odds of having undiagnosed diabetes compared to those in urban areas (Adjusted Odds Ratio [AOR]: 2.30, 95% CI: 1.19–4.45). Additionally, rural participants were 2.33 times more likely to have untreated diabetes than their urban counterparts (OR: 2.33, 95% CI: 1.65–3.31).20
Socioeconomic barriers
Diabetes care in India is heavily influenced by socioeconomic factors, with rural populations facing greater barriers to awareness, treatment, and control of the disease. The disparities in diabetes management between rural and urban India stem from limited healthcare access, financial constraints, and lower health literacy. According to the NFHS-5 data, awareness [urban (33.7%) vs. rural (23.9%)] and treatment [(urban (27.8) vs. rural (17.7) were slightly more in urban, while control of diabetes was poor in both urban and rural India [urban (6.3) vs. rural (8.3)].14 This indicates that a significant proportion of rural individuals with diabetes remain undiagnosed and untreated, likely due to the lack of screening programs and poor access to diagnostic facilities, a disparity further exacerbated by financial constraints, distance to healthcare centers, and the limited availability of specialized care in rural areas. Wealthier urban populations tend to have higher awareness and better diabetes management, whereas poorer rural populations face significant barriers to diagnosis and treatment. According to the ICMR-INDIAB study, states with lower human development indices have higher proportions of undiagnosed diabetes and poorer diabetes care.9
The cost of diabetes management, including regular glucose monitoring and medication, poses a significant financial burden for rural populations, leading to delayed or inadequate treatment (Figure 2). A systematic review by Oberoi et al.,21 (32 studies), found that the cost of managing diabetes in India ranges between ₹8,000 and ₹46,000 per annum, posing a significant financial burden, especially for individuals in rural areas.
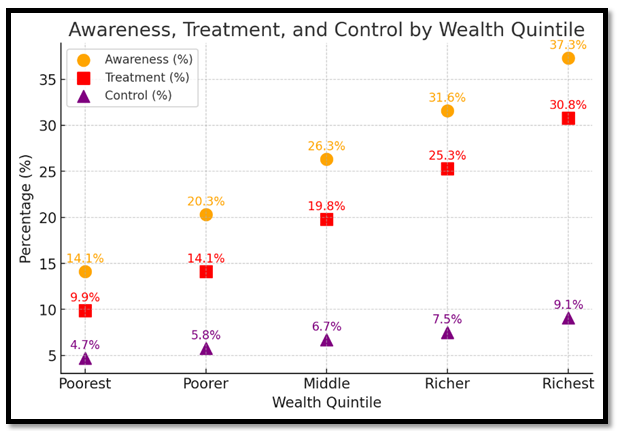
Figure 2 Socioeconomic impact on diabetes awareness, treatment, and control14 (based on NFHS-5 data).
Limited healthcare access and need for strengthened infrastructure
One of the biggest hurdles in rural diabetes care is limited access to healthcare facilities and specialists. A shortage of trained endocrinologists, diabetologists, and diagnostic facilities in rural areas delays diagnosis and treatment initiation. Only 45.2% of individuals in rural areas with diabetes have access to adequate diabetes care, compared to 68.5% in urban India.9 A study by Banerjee found that elderly residents in rural areas were seven percentage points less likely to utilize healthcare services compared to their urban counterparts.22
The Health Dynamics of India report on infrastructure and human resources, published by the Ministry of Health and Family Welfare, highlights a severe shortage of community health centers (CHCs) in rural India, with an almost 80% deficit in required facilities. Additionally, the report reveals that 31.4% (52,116) of all rural sub-centers lack proper infrastructure, as they do not have dedicated buildings.23 As of March 2023, only 4,413 specialist doctors were available in rural CHCs, far below the required 21,964 specialists, indicating a critical gap in healthcare accessibility.24
In addition to limited healthcare infrastructure, several contextual barriers hinder effective diabetes care in rural India. Low levels of educational attainment reduce awareness of diabetes symptoms, complications, and the importance of long-term management, often resulting in delayed diagnosis and poor treatment adherence. The WHO SAGE study in India found that individuals with more years of education were more likely to be aware of their diabetes diagnosis and engage in effective self-management practices.25 The absence of certified diabetes nurse educators—who play a vital role in delivering personalized diabetes self-management education—further limits patient support in these settings.26 The National Diabetes Educator Program (NDEP) and the Association of Diabetes Educators (ADE) were established with the goal of training and certifying professionals to become qualified diabetes educators.27 Long travel distances and poor public transport hinder routine follow-ups, especially for the elderly, increasing both out-of-pocket costs and wage loss. To address these barriers, the Indian government launched Ayushman Bharat in late 2018 to improve primary healthcare access, provide free NCD medications, and deliver care closer to people's homes.28,29 Moreover, extreme weather conditions, such as monsoon floods or heat waves, often disrupt access to care and medication supply chains, particularly in geographically vulnerable regions.30,31 These factors collectively contribute to underdiagnosis, irregular treatment, and poor glycemic control, highlighting the urgent need for decentralized and context-sensitive diabetes care models in rural India.
Government & private initiatives & policies
The Indian government has launched several recent initiatives specifically aimed at managing and preventing T2DM, focusing on early detection, affordable treatment, and lifestyle modification. Table 2 shows some of the initiatives.
|
Initiative |
Description |
|
Screening and standard care initiative (2025 Target)25 |
The Ministry of Health and Family Welfare aims to screen and provide standardized care for 75 million individuals with diabetes or hypertension by 2025. In collaboration with WHO, this initiative integrates diabetes management into primary healthcare, focusing on accessible and quality care. |
|
Ayushman Bharat health and wellness centres (HWCs)26 |
HWCs under Ayushman Bharat focus on screening individuals over 30 years old for diabetes and other non-communicable diseases (NCDs). They provide free consultations, diagnostics, and treatment for diabetes, especially targeting rural and underserved populations. They also promote wellness activities and lifestyle changes to prevent diabetes onset. The progress of each HWC is verified against performance indicators through online portals. |
|
National programme for prevention and control of non-communicable diseases (NP-NCD)27 |
As part of the National Health Mission (NHM), NP-NCD has expanded to include over 700 District NCD Clinics and numerous community-level facilities. The program emphasizes infrastructure strengthening, health promotion, and awareness campaigns for managing diabetes and early diagnosis. |
|
Free medication and generic drug access26 |
Through initiatives like the Pradhan Mantri Bhartiya Janaushadhi Pariyojana (PMBJP), the government provides affordable diabetes medications, including insulin, at subsidized rates in government-supported pharmacies. |
|
Rural diabetes prevention and control campaign28 |
Initiated in 2021, this campaign focuses on diabetes prevention and control in rural areas, exemplified by its launch in Purana Ramnagar village, Varanasi district. |
|
Chunampet rural diabetes prevention project (CRDPP)29 |
This project implements comprehensive diabetes screening, prevention, and treatment using a combination of telemedicine and personalized care in rural India. |
|
Research society for the study of diabetes in India (RSSDI)30,31 |
I. Village adoption program: doctors actively collaborate with specific villages to deliver direct diabetes care. This initiative focuses on educating rural populations about diabetes prevention, healthy lifestyle practices, and disease management through structured awareness sessions. II. Actively contributes to advancing diabetes care by conducting research on T2DM, developing and updating clinical guidelines for T2DM management, III. Comprehensive screening programs to identify individuals at risk, assessing factors such as obesity, hypertension, and prediabetes. IV. RSSDI trains community healthcare workers, equipping them with the necessary skills to effectively manage diabetes cases within their villages. V. Mobile clinics and health camps, offering free diabetes screenings and treatments and ensuring access to healthcare in remote regions. |
Table 2 Key Diabetes management initiatives in India
Recommendations
A well-rounded approach that includes education, early detection, strengthened healthcare infrastructure, lifestyle support, medication access, follow-up care, and supportive policies can empower rural communities to better prevent, identify, and manage T2DM. The strategies outlined below provide a roadmap for implementing these interventions in India’s rural regions.
Increase awareness and education
Expand screening and early detection initiatives
Strengthen primary healthcare infrastructure
Promote lifestyle interventions and dietary changes
Improve accessibility and affordability of medications
Affordable Medication and regular Medication Supply Chains: Expand government schemes and public-private partnerships to subsidize diabetes medications and insulin, making them accessible to low-income rural populations.
Enhance monitoring and follow-up
Leverage policy support and public health programs
While universal diabetes screening and telemedicine initiatives are highly promising, their implementation in rural India faces challenges. Universal screening requires a substantial scale-up of workforce training, logistics, and community engagement, particularly in remote and underserved regions. Telemedicine, though cost-effective in the long term, depends on stable internet connectivity, digital literacy among patients and providers, and sustained infrastructure investments. Policy translation should therefore be phased and context-specific, beginning with high-risk populations and supported by pilot programs, public–private partnerships, and capacity-building efforts.32–38
Diabetes care in rural India remains a significant public health challenge, requiring long-term, sustainable interventions tailored to the unique needs of rural populations. The increasing prevalence of T2DM in these regions highlights the urgent need for improved screening, early detection, and accessible treatment options. Addressing challenges requires region-specific strategies, including community-based screening programs, dietary education, and mobile healthcare units. By adopting a patient-centered, technology-driven, and policy-supported approach, rural India can move towards better diabetes control and prevention. Encouraging healthier lifestyle habits, improving medication adherence, and expanding government-backed initiatives will help mitigate the growing burden of diabetes in these underserved regions. The future of diabetes care in rural India depends on sustained efforts, innovative healthcare delivery models, and collective action from both the public and private sectors, ensuring that no community is left behind in the fight against diabetes.
We extend our acknowledgment to Dr. Raghunath Dantu from MEDEVA for his involvement in the manuscript editing process.
The authors declare no competing interests.
No funding was received for conducting this study.

©2025 Maheshwari, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.