Journal of
eISSN: 2373-4345


Case Report Volume 4 Issue 6
1Lebanese school of dentistry, Lebanon
2Department of Oral & -facial Imaging - School of Dentistry, Lebanese University, Lebanon
3Department of Oral and Maxillo-facial Imaging - School of Dentistry, Lebanese University, Lebanon
Correspondence: Chadi Torbay, Lebanese school of dentistry, Lebanon, Tel 9613947112
Received: May 04, 2016 | Published: August 9, 2016
Citation: Torbay C, Nasseh I, Sokhn S. Use of CBCT in the detection of second mesiobuccal (MB2) canal in maxillary first molar. J Dent Health Oral Disord Ther. 2016;4(6):172-175. DOI: 10.15406/jdhodt.2016.04.00134
Multiple procedures are used to detect the presence of second mesiobuccal canal in the mesial root of the upper first molar. In this article, a case will be presented in order to show the use of cone-beam computed tomography (CBCT) in the detection of a second mesiobuccal (MB2) canal in maxillary first molar, unidentified neither clinically nor with conventional radiographic methods.
Keywords: CBCT, MB2, root canal therapy, endodontic
The main objective of root canal therapy is thorough shaping and cleaning of all pulp spaces and its complete filling with an inert filling material (European Society of Endodontology 2006). The inability to locate, debride or fill properly all canals of the root canal system induce a decrease in the long-term prognosis, and is a major cause of post-treatment disease.1,2 Together with diagnosis and treatment planning, a better knowledge of the root canal system and its frequent variations are an absolute necessity for a successful root canal treatment. In literature, the mesiobuccal (MB) root of the maxillary first molar has generated more research and clinical investigation than any other root.3 The purpose of this article is to show through a clinical case the use of CBCT in detecting an MB2 for better prognosis of a mistreated first maxillary molar, and facilitate the way for endodontic retreatment in a conventional way rather than surgical one.
Prevalence of the second mesial canal
Histological studies suggest that the presence of two MB systems ranged from 18 to 96%.4 Moreover they communicate frequently along their lengths, and terminate separately in two or more portals of exit in greater than 58% of the time.5 Clinician must assume that all maxillary first molars have four canals until proven otherwise.3 Many literature case reports discussed the presence of three root canals in the upper mesial root.6 The second mesiobuccal (MB2) entrance of the pulp system in the mesial root is commonly located within the developmental groove on an approximate line between the MB1 and the palatal orifice, and parallel to the mesial marginal ridge (MMR). Knowing that all orifices originate on the pulpal floor, and approximately lie on the same plane, the clinician must move mesially rather than chasing apically into the pulpal floor to identify the MB2. The MB2 orifice may be displaced lingually far from the MB1 orifice and closer to the palatal orifice7 (Figure 1). While the standard research techniques, such as dental operating microscope, magnifying loupes, ultrasonic tips, staining the chamber floor, rhomboidal access cavity and micro-openers, increase the finding of a second mesiobuccal canal (MB2), the root canal anatomy still presents a complex challenge that requires diagnostic approaches to successfully localize, negotiate, disinfect and fill the root canal system.8
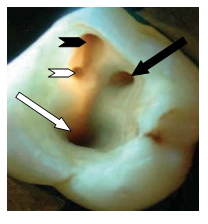
Figure 1 Trapezoidal access cavity of an upper first molar showing the four entrances of the canals (black head arrow MB1, white head arrow MB2, and black arrow MP and white arrow distal canal).
Cone beam technology in endodontic
The development of X-ray cone-beam computed tomography (CBCT) systems have been introduced for imaging hard tissues of the maxillofacial region.11 CBCT is capable of producing sub-millimeter resolution (ranging from 400μm to as low as 125μm) with images of high diagnostic quality. The short scanning time (10-70s) and radiation dosage is reportedly up to 15 times lower than that of conventional CT scans. Although the CBCT principle has been in use for almost three decades,12 its use is mainly systematic for surgical procedures rather than endodontic treatments. CBCT in endodontic has been indicated and used to assess internal anatomy,13 to diagnose the presence of apical lesions,12 to detect root resorption,14 root fractures15 and also to estimate root canal length.16 This new technology provides a 3D representation with minimal distortion and clarifies the detection of what was unknown in a 2D x-ray.
A 35-year-old patient was referred for an endodontic retreatment of the first upper right maxillary molar. The patient chief complaint is the malaise while eating and a tumefaction that pumps up from time to time. The previous endodontic treatment was done five years ago and a crown restoration was done. The patient medical history presents no problems and his dental hygiene is acceptable. Upon extra-oral examination, no tumefaction was detected while the intraoral exam showed a buccal fistula, a ceramo-metallic crown and no food impaction was present between adjacent teeth (Figure 2A). Using the gutta-percha technique, a peri-apical radiograph was taken with gutta percha cone within the fistula orifice. It showed a metal post in the palatal root, with a well-defined radiolucency at the apical side of the mesial root (Figure 2B).

Figure 2a Intra-oral exam showed a ceramo-metallic crown at the upper first molar with a buccal fistila.
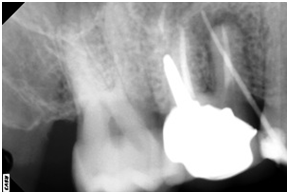
Figure 2b A peri-apical radiograph showed a metal post in the palatal root, with a well-defined radiolucency at the apical side of the mesial root.
Hypotheses elaborated in this case are many including:
Treatment possibilities in this case:
The treatment procedure consisted on the removal of the crown with the aid of a crown removal kit; ultrasonic tips were used for the removal of the metallic post, and the search for the entrance of the second mesial canal was conducted with the use of binoculars. While searching for the MB2 a perforation in the pulp chamber floor was performed. Decision was made to obturate the perforation with MTA and to postpone the session until a CBCT is done. While studying the CBCT, the cuts in the three planes (axial, sagittal and frontal cuts) showed a clearly not obturated canal in the mesial root in direct relation with the lesion (Figure 3). A new search for the MB2 entrance was conducted and finally the MB2 entrance is found. Endodontic therapy was done and two separated mesiobuccal canals where completely cleaned and obturated. A peri-apical radiograph was done five month later showing the complete cicatrisation of the lesion (Figure 4).
Failure of endodontic treatment in maxillary first permanent molar teeth is due to the failure to locate and clean the MB2 canal.17 Since Hess in 1921, its incidence has been reported and discussed by several authors. Weine in 1969 showed that 51% of molars have two mesial canals (of 208 teeth, 107 showed two canals in maxillary molars merging toward a single apical foramen, or into two distinct canals with separate apical foramina). Furthermore, a wide range of variation is present in the literature with respect to frequency of occurrence of the number of canals in this root.3 Cleghorn in his literature review highlighted the difference between laboratory (60.5%) and clinical studies (54.7%) in identifying multiple canals in the MB roots of maxillary first molars.4 An ex vivo micro-computed tomography study also compared MB2 presence with results showing 20% incidence of one canal and 80% incidence of two canals in the MB root.27 Finding additional root canals play an important role in the outcome of root canal treatments.5 CBCT examination, widely employed for oral diagnosis, has improved the ability to diagnose MB2 canals, because it allows image visualization from multiple orientations at very thin slices without disturbing the overlapping structures. Although there is little evidence of the influence of root filling and voxel size in MB2 canal detection19 and artefacts that can compromise scan quality,20 authors report that the sensitivity and specificity values of CBCT for the diagnosis of MB2 are high.25 According to ALARA principles (As Low as Reasonably Achievable), the examination protocols must provide both adequate diagnostic ability and also reduced radiation exposure.18 Even though CBCT is a reasonable method for investigating the presence of MB2 canals according to the basic principles of justification of means and aims the dose of radiation should be considered.
Cone beam computed tomography is a useful addition to the endodontist’s armamentarium for identifying the number of root canals or the missed ones. Compared to standard radiographic techniques, it has higher mean values of specificity and sensitivity due to the ability to manipulate the cuts in different plans providing by that a better way to examine root canal anatomy in fine details, which elevates the possibility to apply its utility in diagnosis or in retreated endodontic cases especially when surgery is planned, and maybe as a first approach before treating the tooth to avoid omitting any canal from being cleaned and obturated. The morphology of the mesiobuccal root of the maxillary first molar teeth is a complex pulp system and the present classifications do not fully reflect its complexity.25 In order for the practitioner to have a clear concept of the pulp system in the tooth under treatment one should use all the armamentarium provided till our date.
None.
None.
The author declares there are no conflicts of interest.

©2016 Torbay, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.