Journal of
eISSN: 2373-4345


Case Report Volume 10 Issue 1
1Dental School, Federal University of Pernambuco, Brazil
2Department of Prosthodontics and Oral Facial Surgery, Federal University of Pernambuco, Brazil
Correspondence:
Received: January 07, 2019 | Published: January 14, 2019
Citation: Carvalho JL, Guimarães RP, Souza FB, et al. Risks and actual results of over the counter products on dental bleaching: a case report. J Dent Health Oral Disord Ther. 2019;10(1):28-33. DOI: 10.15406/jdhodt.2019.10.00455
The search for pre-determined standards of beauty is taking space in Dentistry, often at the expense of their own oral health. In order to meet this population, the market has been offering various whitening techniques, many without the supervision of the dentist. Are the over the counter (OTC) products, purchased directly from the shelves of pharmacies, grocery stores or internet available in various presentations, such as gels, varnishes, toothpastes, strips, mouthwashes and chewing gum. Despite the ban on the sale, in Brazil, by the National Health Surveillance Agency (ANVISA), these products can be purchased at foreign sites and reach consumers via post. This paper reports the case of a female patient, who sought guidance for the use of a bleaching product in the form of varnish (Pro Light/Dentovations), acquired via the Internet. After use according to manufacturer's guidelines, the bleaching result was lower than expected, so the patient was submitted to the office whitening to achieve the desired effect. This work should be a warning about the risk of using these home whitening indiscriminately, instead of low significance results.
Keywords: cosmetic dentistry, dental aesthetics, hydrogen peroxide, tooth whitening
Alterations of the natural color of teeth occurs in dependence on innumerable extrinsic and intrinsic factors. Extrinsic stains can be caused by the ingestion of food with dyes, such as tea, coffee, cola-based soft drinks, red wine, beets, due to excessive use of smoke, accumulation of biofilm and use of some types of medicines. Its removal depends on a good hygiene or prophylaxis done in a dental office. Changes in intrinsic origin, in turn, occur due to a number of factors, such as: changes in tooth formation, diseases occurring during the intrauterine life, dental trauma, pulp mortification, inadequate access to the pulp chamber, misuse of drugs and of filling materials, fluorosis and aging of teeth.1,2
Vanity often overlaps the health care. It is believed that it is not enough to be healthy; it must be suitable to be the most stringent standards imposed by fashion. White teeth are an essential cosmetic factor, so the practice of whitening is increasingly disseminated in the media.3,4
Regardless of the technique performed, the final product and main active agent of bleaching is hydrogen peroxide, which acts as a potent oxidant through the formation of free radicals, reactive oxygen molecules and peroxide anions.5−7 The whitening techniques available are office whitening, supervised whitening, home-made custom molding and dentist guidance, as well as home bleaching products, which are marketed openly in some countries because they are considered as cosmetic products. When used under the guidance of a professional, over-the-counter (OTC) bleaching also achieves good results, but used without proper monitoring provide have side effects. To indicate the type of bleaching that is appropriate for each case, it is very important that the professional knows how to diagnose the cause of dental discoloration, as well as knows available whitening techniques.4−10
In 1991 the Food and Drug Administration (FDA) stopped considering bleaching agents as cosmetics, reclassifying them as drugs or medications. In 1994 the ADA (American Dental Association) established criteria and recommendations for use for the efficacy of bleaching and patient safety. 4 In Brazil, the National Agency for Sanitary Surveillance (ANVISA) approved in 2015 a resolution on the commercialization and control of dental bleaching agents.8,11
The side effects of bleaching agents are diverse. According to Caldas et al.,8 changes in the morphology of the enamel structure associated with bleaching agents can be observed, such as areas of depression, crater formation, surface porosities, expansion of the Retzius incremental striations, microhardness and prism exposure. Araújo et al.12 say that the main factor of enamel degradation is the time that the bleaching agent comes into contact with it.8−13 However, some studies report that lesions have no clinical significance, since after a period of 7 to 14 days the exposed surfaces can be remineralized. This occurs mainly if treated appropriately as the topical application of fluoride gel after bleaching.8,12,14
In addition to these more common side effects, bleaching agents may also be responsible for soft tissue damage. They can either burn or necrotic tissues due to the caustic effect of hydrogen peroxide. These substances participate as promoters or co-carcinogens, potentializing the effects triggered by the inducers. It is noteworthy that these chemicals are not initiators, because in the absence of an initiating agent they are unable to initiate oral cancer.4,14
Considering the risks of the indiscriminate use of peroxide products without professional indication and supervision, this paper aims to report a clinical case in which the patient made use of a home bleaching agent with professional supervision, as well as the whitening in the office. There is also an alert for the risks of excessive and incorrect use of bleaching agents.
A female patient sought the dental clinic service of the Federal University of Pernambuco (Brazil) in search of guidelines for the use of a domestic bleaching product acquired through the internet. It was the product Pro Light (Dentovations), which appears as a lightening varnish with activating light (Figure 1).

Figure 1 Presentation of the pro light household bleaching varnishes (luster premium white/dentovations).
The patient was instructed to use the product exactly as the manufacturer recommended, two or three times a day, to perform 20 applications within a week. Detailed instructions for how to use the product are described in Figure 2.
Prior to step 4, the patient is instructed to perform mouthwash with about 10 ml of the liquid contained in the flask 1 (Figure 1) for 10 seconds, without swallowing, which the manufacturer calls a pre-treatment, or "throttle rinse." After applying the gel, it is asked to wait the time of 20s for the gel to dry and thus, the teeth can come in contact with lips and tongue. Twenty applications are recommended, which the manufacturer calls "treatments". These can be done all at once, or within a week if the patient has not had dental bleaching in the previous six months.
Photographic shots were taken before and after treatment. The objective color registration was performed using an Easy Shade (Vita) digital spectrophotometer. The coloring of the middle third of the upper anterior elements (13 to 23) was taken as reference, according to the CIELab space of the Commission Internationale de l'Eclairage and also the respective values in the Classical Vita Scale (Figure 3). For the numerical record, the arithmetic mean between the L* a* and b* values of the six previous elements was considered (Table 1).

Figure 3 Initial clinical appearances before and after the use of domestic bleaching, with emphasis on the classification of the classical vita scale (tooth 13 to 23).
Tooth |
L* initial |
a* initial |
b* initial |
L*After OTC |
a* After OTC |
b* After OTC |
L* final |
a* final |
b* final |
13 |
79,90 |
1,10 |
27,40 |
78,50 |
1,80 |
30,10 |
75,20 |
2,00 |
28,90 |
12 |
77,20 |
2,70 |
30,60 |
81,80 |
-0,10 |
27,20 |
78,50 |
-0,10 |
23,80 |
11 |
83,00 |
-0,50 |
23,30 |
83,80 |
-2,50 |
20,80 |
81,00 |
-2,20 |
17,90 |
21 |
83,20 |
-0,10 |
23,30 |
84,60 |
-1,60 |
22,50 |
83,00 |
-1,70 |
18,20 |
22 |
82,60 |
1,50 |
28,80 |
82,20 |
0,20 |
27,90 |
79,50 |
0,50 |
25,60 |
23 |
77,00 |
2,20 |
29,60 |
78,20 |
2,00 |
31,10 |
76,80 |
1,90 |
28,30 |
Mean |
79,9 |
1,15 |
27,17 |
81,52 |
-0,03 |
26,60 |
79,00 |
0,07 |
23,78 |
Table 1 Absolute and mean values recorded by the spectrophotometer
For the determination of the staining differences at different treatment times, the ΔE was calculated using the formula: ΔE* =[ΔL* 2 Δa* 2Δb* 2] 1/2, where ΔL*=L0-L1; Δa=a0-a1; Δb= b0-b1, where 0 (initial measure) and 1 (final measure). The value of ΔE between the initial color and the color obtained after the use of the product was 2.08.
Figure 4 shows the comparison between the records made by the patient herself, with the scale that accompanies the product. Initially it pointed the value 15, considering its central incisors, and after the treatment, it mentioned the value 9.

Figure 4 Photographic records showing the color selected by the patient using the color scale accompanying the product, taking element 21 as reference.
Because she was not satisfied with the result of the household product, the patient underwent a 35% hydrogen peroxide (Whiteness HP Maxx/FGM) office bleaching session, which was used in a single application of 40min, with activations with LED device (Gnatus) being 20s per tooth, every 10 min. Figure 5 illustrates the clinical sequence of office whitening.
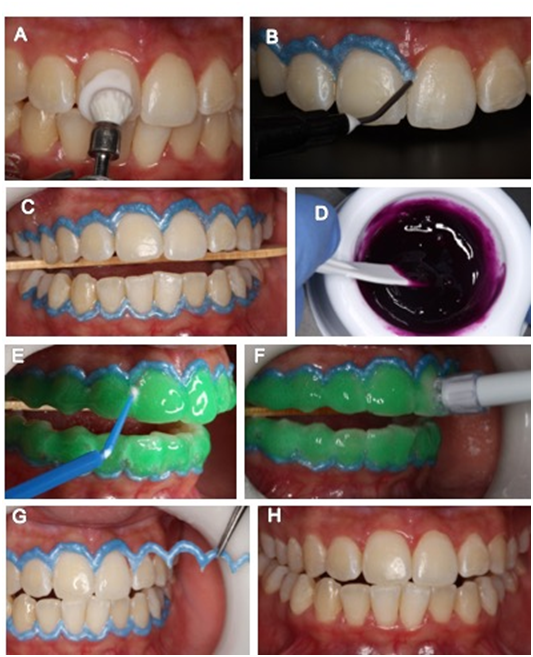
Figure 5 In-offices bleaching. A: Prophylaxis with paste of pumice stone and water. B: Application of the gingival barrier; C: Positioned tongue protector; D: product handling (Whiteness HP/Maxx); E: Elimination of bubbles with a brush; F: Removal of the gel at the end of treatment with trimmed sucker; G: Removal of the gingival barrier; H: Final clinical aspect.
After the office whitening session, neutral fluoride gel was applied for 1min and the patient was instructed to avoid the consumption of color drinks for 72 hours until the complete rehydration of the tooth structure. Figure 6 shows the comparison between the initial clinical appearance and after the office bleaching. The value of ΔE for the office technique was 3.78.
People have been experiencing intense social pressure around the "perfect smile and white" as a pattern of beauty, which leads to widespread disclosure and greater interest on the part of people regarding dental bleaching before any aesthetic rehabilitation.3−5 The popularization of vital tooth whitening began in 1989, with the work of Haywood and Heymann, and this possibility was disseminated through the media through articles and advertising spaces.
In order to satisfy the public, the market offers various bleaching techniques, many of them in the form of home whitening. This whitening modality, without the supervision of the dentist, uses the law of supply and demand, thus providing a lower cost product. Thus, bleaching leaves often be treated with due care and attention it deserves, and is now treated as a cosmetic, and often abused, as a makeup, not taking into account its side effects which may be mild or rather severe.3,4,13 In our case, the patient, even making use of a domestic bleaching, did not give a professional monitoring for fear of side effects that its misuse could come to cause. However, in most cases, patients using these products indiscriminately, without professional supervision.
OTC products appeared in the United States in the early 2000s as a lower cost dental alternative than the traditional one made by professionals. This is even the biggest draw of advertising campaigns, which highlight the empowerment of consumers by their own whitening. OTCs generally contain low concentrations of hydrogen peroxide or carbamide, and they come in a variety of forms, such as strips, varnish, gels, pastes, mouthwashes, chewing gum, chewing gum and toothpaste widely available to consumers in pharmacies, supermarkets and internet.8, 15 The patient reported that she purchased the OTC product in the form of a varnish, via the internet at a North American site and received it at home through a posting service.
Toothpastes and mouthwashes have limited efficacy since they contain only abrasives to remove stains from the outer surface of the teeth. Only some of these products contain bleaching chemicals that could justify their effectiveness. There are also toothpastes that have a bluish dye dyeing the tooth momentarily producing transient and illusory whitening effect. These whitening pastes, which remove surface stains, should not be confused with actual bleaching agents, which act by oxidizing the pigments and "breaking them" into lighter molecules, thus attenuating the color of the teeth.6,16
The most commonly used abrasives in the toothpastes available in Brazil are calcium carbonate, silica, alumina and calcium bicarbonate, although others may be present. While these abrasives can polish the surface of the tooth, its abrasive action along with the mechanics produced by brushing can cause injury to the teeth. On the contrary, the wear action of bleaching toothpastes can lead to prolonged use in the darkening of the teeth due to the gradual reduction of the enamel thickness.17 According to Sokolonski et al.,17 the demineralization due to bleaching containing carbamide peroxide is significantly less than that caused by sodium bicarbonate. Thus, dentifrices containing a very high amount of abrasives, especially sodium bicarbonate and alumina, if used abusively, cause greater abrasion to tooth enamel than bleaching with peroxides.6,16, 17,18
Other side effects are associated with improper use of bleaches, such as: changes in the properties of restorative materials, such as increased solubility of cements. Structural erosion may also lead to dentin hypersensitivity.6,8,12,16,17,18 In the case presented here, there was mild degree of sensitivity, transiently during use of the product. More serious injuries can be found in soft tissues, due to the caustic effect of hydrogen peroxide, in the form of gum burns and even necrosis in more severe cases. According to Consolaro et al.,4 bleaching agents participate as promoters or co-carcinogens in oral chemical carcinogenesis, potentiated and triggered by early carcinogenic agents, including in other gastrointestinal mucosae. When the isolates do not reveal carcinogenic, that is, they were unable to associate with oral cancer. In other words, hydrogen peroxide does not induce, does not initiate a normal cell from a mutation that evolves into a malignant neoplasm, but may stimulate a proliferation of the primed cell. Almost all of these home whitening products often do not provide complete information on their package inserts. The product presented here, for example, does not even contain any information about the components of its formulation. That is: it is not known which substance is responsible for whitening, nor, in the eventual occurrence of hypersensitivity, will be able to identify any components responsible for an abnormal organic response.
In the office bleaching, the risk of peroxide becoming a promoting agent is lower, because in this type of bleaching the trained professional makes use of a gingival barrier, isolating the teeth, thus preventing direct contact of the gel on the gingiva. In this way the absorption of the product by the organism is diminished and the risks are significantly smaller. In addition to the fact that during the office bleaching, the patient comes in contact with the oxidant in small frequency and for a short time.4,14 From the point of view of the way of use, the product mentioned here is very uncomfortable because the patient needs to avoid the contact for some time of the lips with the teeth after the application of the product, as well as the varnish with the gingiva after the application, task is almost impossible. Moreover, the concentration of the bleaching agent is not known, nor even the possible consequences of the contact of these soft tissues with it. The carcinogenic effect of the whitening agent is very small, but its importance is in the frequency with which the hydrogen peroxide comes in contact with the buccal mucosa: every day, several times every 24 hours. It is at this moment that the professional orientation is essential to avoid this effect, since often the user does not worry about the side effects of the product, because he thinks that it is a cosmetic, so it makes abusive use, for ignore the risk involved in using a bleaching agent indiscriminately.4.14
Hydrogen peroxide can and should be used in the mouth, even as an antiseptic in some specific situations, for example in pericoronaritis, or in acute ulceronecrosant gingivitis. However, its direct and continuous use on the mucosa should be occasional and for therapeutic purposes and should never be used without prescription.8 In order to control the free access of the Brazilian population to these products, ANVISA created a resolution, starting on January 14, 2015, in which any bleaching product based on peroxide in concentrations above 3% was classified as a stripe product red and can only be purchased in pharmacies by prescription from a dental surgeon. The measure also requires that the packaging and campaigns of the same follow the terms of the resolution, containing the text "Sale under dental prescription." But these products (OTC) are legalized in the USA. Thus, ANVISA together with the Dental Council of Dentistry (RO) are unable to control their sale through the internet and consequently delivery by post.8,11,13
The office technique is usually done with hydrogen peroxide in concentrations of 35 to 40%. After an interval of 7 days another session can be performed, depending on the need of the patient, and the same procedures are repeated. Pimenta et al.2 found that after the second session, the removal of pigments is usually satisfactory. In the case presented here, the need for multiple sessions was evidenced by the low ΔE value after the single session performed. Some authors have also proven that more expressive bleaching results are obtained with the association of supervised and clinic techniques.2,5
Aesthetics is essential in the social life of the individual. The way you see yourself directly influences your self-esteem and your social life as a whole, both professionally and emotionally. What is not aesthetically pleasing to the eye is not accepted, since the image passes a greater amount of information and at a much greater speed than the speech. Teeth and smile draw a lot of attention in the process of non-verbal communication. A beautiful smile gives the impression of care, health and well-being. It is important in everyone's life, but abuse and exaggeration should not be committed, balance is essential, beauty and health cannot be separated.15−20
None.
The authors declare that there is no conflict of interest.

©2019 Carvalho, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.