Journal of
eISSN: 2373-4345


Case Report Volume 16 Issue 2
Faculty of Dental Medicine, University Hospital of Farhat Hached Sousse, Tunisia
Correspondence: Hanen Boukhris, Faculty of Dental Medicine of Monastir, Farahat Hatched Hospital, Service of Dentistry, Research Laboratory LR 12SP10, Functional and Aesthetic Rehabilitation of Maxillary, 4000 Sousse, University of Sousse, Tunisia
Received: March 17, 2025 | Published: June 5, 2025
Citation: Boukhris H, Zidani H, Salah KBH, et al. Mesiodens: a multidisciplinary approach to diagnosis and management. J Dent Health Oral Disord Ther. 2025;16(2):51-54. DOI: 10.15406/jdhodt.2025.16.00643
Mesiodens, the most common type of supernumerary tooth located in the anterior maxillary region, can lead to various dental complications, including altered eruption, malocclusion, and aesthetic concerns. This paper aims to examine the clinical characteristics, classification, and treatment modalities of mesiodens, focusing on the available management options, both conservative and surgical. A thorough review of the literature was conducted to assess the prevalence, types, and outcomes of treatments for mesiodens. The findings indicate that conical mesiodens are the most prevalent, although other variations, such as tuberculated and molariform mesiodens, are also observed. Treatment strategies depend on the type of mesiodens, the patient's age, and the presence of associated dental issues. Options include extraction followed by spontaneous eruption, orthodontic traction, or surgical repositioning. The paper concludes that while extraction remains the most common intervention, retaining mesiodens is an appropriate alternative when specific clinical criteria are met. Optimal treatment planning is crucial to ensure both functional and aesthetic success.
Keywords: mesiodens, supernumerary teeth, maxillary anterior region, treatment strategies, dental eruption, orthodontic management, surgical intervention
The presence of supernumerary teeth, particularly mesiodens, is a relatively common dental anomaly that can lead to various complications, including impaction, malpositioning, and aesthetic concerns. Mesiodens, which are additional teeth located in the maxillary midline, often disrupt the normal eruption of permanent incisors, resulting in transposition, rotation, or delayed eruption. These anomalies pose significant challenges in both functional and aesthetic rehabilitation, requiring careful clinical and radiographic evaluation for an appropriate treatment approach.1-3
The management of such cases is complex and necessitates a multidisciplinary approach, integrating orthodontic, surgical, and prosthetic considerations. Cone beam computed tomography (CBCT) plays a crucial role in assessing the precise position of the impacted teeth and their relationship with surrounding structures. The decision to extract or retain mesiodens depends on multiple factors, including their morphology, position, and impact on adjacent teeth. When retention is considered viable, prosthetic solutions can be implemented to enhance both function and aesthetics.4
This case report presents the comprehensive prosthetic rehabilitation of a young adult with dysmorphic mesiodens in transposition with impacted central incisors. Due to the anatomical complexity and the patient’s high aesthetic demands, a conservative approach was chosen. The treatment plan included the extraction of the impacted permanent incisors, preservation of the mesiodens, and their rehabilitation with zirconia-based ceramic crowns. The therapeutic strategy aimed to achieve optimal functional integration while restoring a natural and harmonious smile. This report highlights the importance of a meticulous diagnostic process and a personalized treatment plan to ensure long-term success in similar cases.5,6
The patient, a 22-year-old male, is in good general health, cooperative, and highly concerned about aesthetics. He sought consultation to correct the shape of his two dysmorphic central incisors in order to achieve an aesthetically pleasing smile.
Clinical examination
The extraoral examination revealed a dental smile. The intraoral examination showed inadequate oral hygiene, with discoloration on the lingual surfaces of the teeth due to smoking. From a periodontal perspective, there was misalignment of the gingival margins, a pseudo-pocket of approximately 4 mm in the region of tooth 11, and a significant vestibular bulge in the anterior maxillary sector, covered by mucosa of normal appearance. At the dental level, both central incisors exhibited an atypical (cuspidated) morphology and were malpositioned (rotation and version), along with anterior mandibular crowding (Figure 1).
Radiographic examination
A panoramic radiograph (Figure 2) revealed the presence of two impacted teeth in the anterior region.
To further investigate, a cone beam CT scan was performed, confirming the presence of retained teeth that were highly positioned near the nasal fossae, with an almost horizontal eruption axis, an apical curvature, and a morphology resembling that of typical central incisors. Sagittal slices revealed that the mesiodens had fully developed roots and an intact root canal system without significant calcifications (Figure 3).
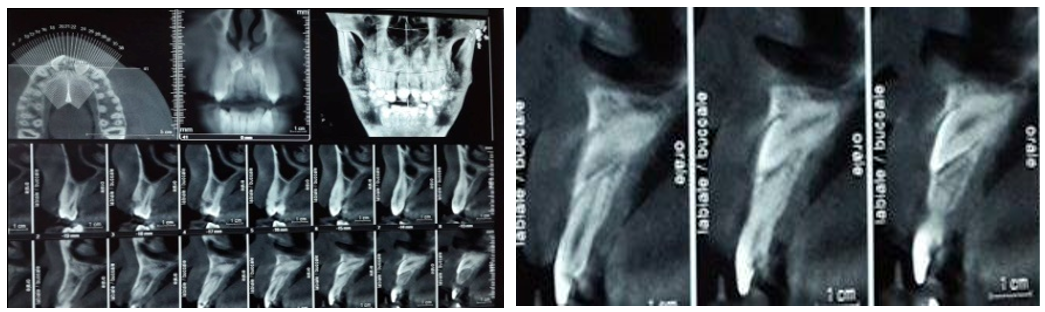
Figure 3 a-b Cone beam shows the presence of two upper, nearly horizontal impacted teeth with an apical bend.
Diagnosis and therapeutic decision
Following clinical and radiological evaluation, the diagnosis of cuspidated mesiodens in transposition with impacted permanent central incisors was established. Given the impossibility of orthodontically repositioning the impacted teeth, the chosen treatment plan included the extraction of the impacted teeth, the preservation of the two mesiodens, and the fabrication of two zirconia-based ceramic crowns for these mesiodens.
The treatment was divided into several stages:
Preprosthetic care and first-generation provisional prosthetic restoration
After rigorous oral hygiene motivation and initial periodontal treatment (scaling, root planing, and polishing), atypical corono-peripheral preparations were performed on the two mesiodens to accommodate ceramic crowns. The preparations adhered to fundamental guidelines, including chamfer or shoulder finish lines with rounded internal angles, rounded edges, and minimal axial taper to prevent undercuts. A mesial stripping of the lateral incisors was also conducted. Endodontic treatment of the mesiodens was performed using a thermal gutta-percha obturation technique (Thermofill) (Figure 4). Two chairside provisional crowns were fabricated using an isomolding technique with self-curing acrylic resin.
Second-generation provisional prosthetic restoration and soft tissue management
A gingivectomy was performed on teeth 11 and 21 to reestablish a harmonious gingival contour (Figure 5).
Two laboratory-made CAD/CAM provisional crowns were fabricated from high-density PMMA resin and cemented on the day of surgery for a three-month temporization period. This technique enhanced precision, saved time, and improved soft tissue healing.
Definitive prosthetic restoration
A simultaneous double-mix impression was taken using a second-generation silicone material. Shade selection was performed using the VitaPan 3D Master shade guide. CAD/CAM technology was employed to fabricate two zirconia frameworks using yttria-stabilized tetragonal zirconia polycrystal (Y-TZP, Cercon® ht, DEGUDENT), which offers high translucency and excellent light transmission properties, making it suitable for anterior restorations (Figure 6). The zirconia frameworks were tried in the mouth to verify stability, marginal fit, and available space for ceramic layering. A fluid silicone material was used to detect any areas requiring adjustments, prioritizing preparation modifications over altering the intaglio surface of the framework.
Final cementation
After final try-in and ceramic layering, adhesive cementation was performed using a resin-modified glass ionomer cement (FujiCem®-Fuji), which was chosen due to the subgingival margins of the prosthetic restorations. These cements provide good adhesion to dentin, which can be further enhanced by pretreatment with polyacrylic acid to open the dentinal tubules (Figure 7).
Mesiodens, the most frequent type of supernumerary teeth, are typically located in the midline between the maxillary central incisors. Their global prevalence ranges from 0.09% to 2.05%.7 Anatomically and clinically, they may present unilaterally or bilaterally, with a higher prevalence in males and in the permanent dentition. According to Mohan et al., mesiodens occur as single entities in 76–86% of cases, in pairs in 12–23%, and as multiple teeth in less than 1% of cases.4
Morphologically, mesiodens are classified as conical, tuberculate, or molariform.6 Conical types are the most common, often presenting as isolated teeth with complete root development, frequently erupting spontaneously in the palatal region between the central incisors.7 Tuberculate mesiodens, such as in the present case, exhibit multiple cusps or tubercles and are often bilateral. They are more likely to remain unerupted and are commonly associated with eruption disturbances of adjacent permanent incisors.7 Molariform mesiodens, although rare, resemble premolars and also show full root development.
The clinical consequences of mesiodens include delayed eruption, rotation, or ectopic positioning of the permanent incisors. Studies have reported that 26% to 52% of cases show obstruction of normal eruption paths due to mesiodens.8 These disturbances not only affect occlusion but also have esthetic and psychological impacts, particularly in children and adolescents, potentially leading to bullying and diminished self-esteem.9,10
The standard treatment protocol for mesiodens is early diagnosis, followed by surgical extraction, particularly when eruption of the adjacent permanent teeth is compromised. In such cases, spontaneous eruption of the incisors may occur, or surgical exposure combined with orthodontic traction may be required.1,8 Advanced imaging techniques such as cone-beam computed tomography (CBCT) enhance the diagnosis and planning of extraction by allowing precise localization and evaluation of root formation and spatial orientation.2,3
In specific situations where orthodontic management is not feasible- due to patient age, financial constraints, or refusal- alternative strategies must be considered. One such approach is surgical repositioning, which may be suitable when the mesiodens is in favourable alignment, adequate space is present, and minimal bone manipulation is needed. However, this technique carries a risk of ankylosis and requires a careful preoperative evaluation.11
Another alternative, especially in the presence of ankylosis or when aesthetic needs are high, is extraction followed by implant placement. This option is often reserved for adults and is advantageous in preventing potential complications such as root resorption, discoloration, or periodontal compromise.2
Interestingly, a more conservative and less conventional strategy- preservation of the mesiodens with extraction of the impacted permanent incisor- has been described in selected cases. This approach is justified only when the mesiodens are well aligned, immobile, fully developed, and free of pathology, including cystic lesions or root resorption of adjacent structures.5,11-13 Additionally, the mesiodens must not show signs of enamel defects, such as hypo mineralization or hypoplasia.14
Treatment planning must be highly individualized, considering the patient’s age, esthetic expectations, economic situation, compliance with long-term follow-up, and occlusal context. Thorough evaluation of the eruption potential and root development of the impacted incisor is essential, as well as assessment of the position, root formation, and mobility of the mesiodens.14
In cases where orthodontic treatment is not an option, restoration of mesiodens as esthetic substitutes may provide a feasible alternative. Such a complex rehabilitation requires precise prosthodontic planning, including study models, diagnostic wax-ups to optimize anterior guidance, potential endodontic treatment, and periodontal recontouring surgery to achieve gingival symmetry.13 Recent case reports and reviews support this approach, especially when functionality and esthetics can be predictably restored.14,15
Mesiodens, the most common type of supernumerary teeth, present a significant challenge in clinical practice due to their potential impact on occlusion, esthetics, and the eruption of permanent incisors. While extraction remains the conventional treatment approach, alternative strategies such as surgical repositioning, implant placement, or even retention with prosthetic rehabilitation may be considered in select cases. The choice of treatment must be guided by a thorough clinical and radiographic evaluation, taking into account patient-specific factors, the condition of the impacted permanent incisors, and the long-term functional and esthetic outcomes. In cases where orthodontic treatment is not feasible, a well-planned restorative approach can provide a satisfactory solution, ensuring both esthetic and functional integration of the retained mesiodens.
None.
The authors declare that there are no conflicts of interest.

©2025 Boukhris, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.