Journal of
eISSN: 2373-4345


Case Report Volume 9 Issue 6
1Department of Oral and Maxillofacial Surgery and Traumatology, Federal University of Bahia, Brazil
2Dentist, Surgeon, Estadual University of Feira de Santana, Brazil
Correspondence: Luis Claudio Cardoso dos Santos, Faculty of Dentistry, Federal University of Bahia (UFBA), Alameda dos Jasmins, number 88, Candeal, Cond. Jardim das Mangueiras, ap 402, Bahia, Brazil, Tel (071) 99633-8313
Received: November 14, 2018 | Published: December 11, 2018
Citation: Santos LCC, Pereira LR, Silva DT, et al. Fronto-nasal cranioplasty using polymethylmethracylate - case report. J Dent Health Oral Disord Ther. 2018;9(6):513-515. DOI: 10.15406/jdhodt.2018.09.00439
Patients who present a background of bone defects seek for harmonic facial contours through surgical rehabilitation. To facilitate the maxillofacial reconstruction, there are two groups of grafts that can be used: the bone and alloplastic materials, such as the polymethyl methacrylate (PMMA), which is one of the alloplastic materials usually used by surgeons in facial rehabilitation. The aim of this study is to present a clinical report about a frontal cranioplasty using PMMA and compare its use with other materials in the literature. A male patient, 35 years old, ASA I, had a motorcycle accident, and a physical examination showed a sinking in the frontal region, deviation of right nasal dorsum and restriction of air passage through the left nostril. At the imaging examination, it was found suggestive signs of naso-orbit-ethmoid fracture and external table fracture in the middle region of the frontal bone. The patient was submitted to a surgical procedure for reconstruction of bone defect and a PMMA graft was used in the frontal bone region. PMMA is usually used because of its ease of adaptation to the bone, reduction of time of the surgery and decrease of blood loss and possibility of infection. PMMA is an attractive alternative for maxillofacial reconstructions.
Keywords: bone fractures, biocompatible materials, polymethyl methacrylate
Patients whom have a historic of of bone defects caused by infections, congenital malformation, neoplasias, iatrogenic deformation, radiotherapy and trauma, seek for harmonic facial contours through surgical rehabilitationn. The cranioplasty restores the skull morphologically and functionally, and it is a fundamental indication for the recovery of the lost bone contour, treatment of the Trephine Syndrome and protection against trauma.1 To facilitate the maxillofacial reconstruction, two groups of materials could be used, such as bone grafts (autogenous, allogeneic, xenogene) and alloplastic materials (titanium, porous polyethylene, hydroxyapatite, and polymethylmethacrylate - PMMA). Although the bone graft is the most frequently used, it has some undesirable aspects of its characteristics, such as possible reabsorption of the graft and difficulty in modeling the bone fragments. As a result, it presents a low predictability and maintenance of the aesthetic-functional obtained at the time of surgery.2 Biomaterials should present some ideal characteristics, such as: biocompatibility, easy fixation, adaptable, light, must have dimensional stability, radiolucency, resistance, absence of electrical and thermal conductivity, inertia and low cost. The Polymethylmethacrylate - PMMA besides possessing several of these characteiristics is a highly viable material for aesthetic purposes.2 PMMA, also known as acrylic resin, is one of the alloplastic materials most commonly used by surgeons in facial rehabilitation of patients with bone deformities.2 The easy handling of the product is carried out in a sterile vat by mixing 2/3 of the powder into 1/3 of the liquid according to the amount needed, for approximately 30 seconds, until the texture is capable of sepatrating from the reservoir. After achieving greater consistency, it can be shaped individually.3 The other prefabricated biomaterials have standard sizes and, on several times, there are friability or excess hardness, thus hampering the wear and tear necessary to personalize the model.4 The possibility of molding the polymethylmethacrylate - PMMA implant through threedimensional prototypes before surgery has some advantages, such as easy adaptation to the bone, reduction of surgery time, reduction of blood loss and possibility of infection, the surgical strategy used, besides clarifying to patients recurrent questions about the procedure.3 In addition, besides to have body tolerance, in the polymerization phase, it must be irrigated abundantly with saline, to avoid losses to neighboring tissues and bone. They can be used on the plates and screws that fix the osteotomies, used with antibiotics, present low cost, give rise to a fibrous capsule, but are not able to integrate to the tissue. Thus, it is best indicated in the rehabilitation of adult patients. Since, because it is fixed and static, it may not follow the craniofacial development of growing youth and children.3 The aim of this study was to report a case of cranioplasty in the fronto-nasal region using PMMA, comparing with other materials used in the reviewed literature.
Patient M.S.L, 35 years old, ASA I, attended to the clinic of BucoMaxiloFacial Surgery and Traumatology of the Faculty of Dentistry of the Federal University of Bahia, reporting difficulty in breathing through the left nostril and sunken face. He reported a motorcycle accident about 1 (one) month, with trauma in the face, evolving with aesthetic complaints in the frontal and aesthetic-functional in a region of nasal dorsum with respiratory restriction in the left nostril. At the physical examination, was observed in the frontal bone a sunken region, deviation of the nasal dorsum to the right side and restriction of air passage through the left nostril. At the imaging examination, signs suggestive of naso-orbito-etmoidal fracture and external plaque fracture were observed in the medial region of the frontal bone (Figure 1). Surgical intervention was performed under general anesthesia, with coronal access and exposure of the bone defect. It was performed refraction of the nose bones, repositioning and fixation with "T" plate of the system 2.0, reconstruction of the external table of the fronto-nasal bone with preparation of polymethylmethacrylate (surgical cement) and bone defect was modeled directly and fixationed with 01 screw of system 2.0 (Figure 2). At the moment, the patient is undergoing postoperative follow-up, evolving with a significant improvement in facial esthetics and improvement of breathing through the left nostril (Figure 3).
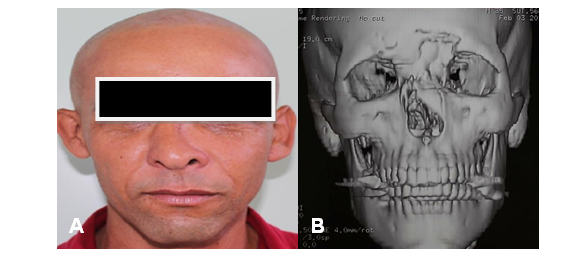
Figure 1 A: Initial clinical appearance in frontal view, showing bulging in frontal region and nasal dorsum deviation. B: 3D reproduction of computed tomography showing frontal and nasal bone defects.
In the daily routine of maxilo-facial surgery there are many causes of bone defects requiring face reconstruction. The substitutes of the hard tissue should be functional, and most of the time, aesthetic and affordable. The use of biomaterials allows reconstruction of these lost structures, restoring function and mechanical resistance.2,5 The cranioplasty technique was used for the treatment of the showed defect. This option is able to correct cranial defects, restore esthetics, protect neural tissue, normalize intracranial pressure, relieve neurological signs and improve the underlying physiology.1,2 Williams et al.,6 in their study on titanium cranioplasty in children and teenagers, reports that the gold standard for this type of defect are autogenous bone grafts. However, there are contraindications, shuch as high morbidity, possibility of reabsorption, risk of postoperative infection (when the defect has an excessive size, it requires a greater amount of tissue), longer in surgical time, adaptation difficulty of the graft, and failure of previous cranial reconstructions make it necessary to search for alternative materials.
There is a recurrent discussion in the clinical literature about the most appropiate alloplastic biomaterial for cranioplasty, such PMMA or titanium. Harris et al.,2 after use PMMA in craniofacial reconstructions, stated that titanium is highly biocompatible, without risk of hypersensitivity reactions, efficient resistance to corrosion, promotes the restoration of the external contour of the skull, but it has a high cost when compared to PMMA. Kwarcinsky et al.,7 when reviewed about the materials, the manufacturing method and the risk of infection of the implants for Craniofacial and Craniofacial Reconstruction, reported that titanium shows biological inertia, favorable strength-to-weight ratio, favorable cosmetic and functional results and natural osseointegration, however, titanium grafts often require pre-fabrication, leading to an increase in lead time and cost. Song et al.,8 in their study on biomaterials for reconstruction of cranial defects, said that the rate of occurrence of complications induced by the implant of titanium for cranioplasty was about 30%, including infection, seroma and hematoma. Some complications required removal of the implant. The PMMA, used in the present study, has several desirable characteristics in an ideal biomaterial, and it is frequently used in the cranioplasty. Harris et al.,2 studying the reconstruction of frontal humeral with a polymethylmethacrylate implant, in two different cases, found that PMMA was efficient in reducing morbidity and surgical time, as well as improving the quality of the prosthesis. In another study, Dantas et al.,5 researched on facial reconstruction with a polymethylmethacrylate implant, stated that this acrylic-based resin is a good option for reconstruction of facial bone defects because it has low cost, decreases surgical time, it is easy to manipulate and to shape, also it is biotolerable and inert. On the other hand, Medeiros et al.,9 after studied complications for use of PMMA injections in the face, says that all facial filling, with the exception of autologous fat implants, can induce an allergic reaction, possibly as angioedema, anaphylaxis or late granulomas. In contrast, in the case of cranioplasty presented in our study no signs of hypersensitivity reaction were observed, following the pattern of cases operated by the Maxilo-Facial Surgery and Traumatology service of the Faculty of Dentistry of the Federal University of Bahia in which there is no case history of the allergic reaction associated with the compound. Khader et al.,4 on his paper, showed that PMMA remains the most widely used polymer for cranioplasty because of its availability, easy to use, strength, tissue compatibility, low cost and radiolucency. Despite this, Basel et al.4 and Dantas et al.5 agree that one of the major disadvantages of PMMA is the high temperature released by an exothermic reaction during its polymerization process (70° to 80° C). It may lead to necrosis and inflammation of the surrounding tissue, requiring constant irrigation with cold saline to protect the brain. The researched scientific literature stand up for the use of polymethylmethacrylate as a graft by its ability to be shaped in an individualized and personalized way and by providing the lowest cost, when compared to alloplastic materials, for this reason can be more easily paid by private health insurance, by the Sistema Único de Saúde (SUS) or by the patient.
The variety of materials to substitute the hard tissue is widely described in the literature. Increasingly, bone substitutes have better properties, which demonstrates an increasing success rates in the performed procedures. This research demonstrates the longing for the ideal facial aesthetics. The PMMA is an easy-to-use, avaliable and versatile material. As shown, the literature bases the use of polymethylmethacrylate as a fill material, although it is necessary more studies to determine the ideal biomaterial. The PMMA prostheses are effective for cranoplasty and for many facial defects that require functional and aesthetic rehabilitation.
None.
Authors declare that there is no conflict of interest.

©2018 Santos, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.