Journal of
eISSN: 2373-4345


Research Article Volume 16 Issue 1
Diploma in Economics, specialised as health-economist in dentistry, former Head of Department of “Dental Care“ in the Federal Ministry of Health, Bonn/Germany and German representative in the Council of European Chief Dental Officers (CECDO), ret, Germany
Correspondence: Rüdiger Saekel, Marienburger Str. 28, D53340 Meckenheim, Germany
Received: January 01, 2025 | Published: February 3, 2025
Citation: Saekel R. Evolution of oral health among younger generations and its possible effects on adult populations: demonstrated by longitudinal data from twelve affluent nations. J Dent Health Oral Disord Ther. 2025;16(1):12-24. DOI: 10.15406/jdhodt.2025.16.00636
Objective: The study aims to examine the impact of consistent dental preventive programmes during childhood and adolescence on the oral health of adult populations in twelve affluent nations.
Methods: The research utilises existing longitudinal epidemiological data, primarily sourced from representative national surveys whenever feasible.
Results: The lowest increases in DMFT during adolescence and middle-age, a period of 28 years, have been realised in Korea, Sweden, and Spain, with increments of 3.7, 5.5 and 6.8, respectively. These figures seem to indicate that well-established preventive measures, oral hygiene habits and regular dental check-ups during youth are maintained into middle-age in these countries. However, this assertion holds true only for Sweden, as Korea and Spain initiated extensive preventive efforts in their youth only after the year 2000. An analysis of the single DMFT components reveals that the low D-values, minor M-values, and high F-values observed in middle-aged individuals from Sweden, Denmark, Norway, Japan, Switzerland and Korea, reflect highly effective dental care systems not only in Sweden but also in these other nations. In contrast, Germany, Great Britain, Australia, Spain and Portugal exhibit lower effectiveness in their dental systems, as preventive strategies were introduced significantly later. The disparities in oral health between the two categories of countries (those with early versus late preventive initiatives) become more pronounced in older age groups.
Conclusion: Comprehensive dental initiatives targeting youth, which commenced in the 1960s and early 1970s, have shown a beneficial effect on oral health that extends into adulthood and later life in countries such as Sweden, Denmark, Norway, and Switzerland. Conversely, nations that implemented regular preventive programmes later, during the 1980s and 1990s or thereafter, have only observed positive outcomes among the middle-aged population, with improvements subsequently leveling off, as seen in Great Britain, Germany, Korea, New Zealand, Portugal, and Spain. Therefore, it is advisable that these countries consider implementing preventive strategies for young adults to strengthen the oral health practices established in their formative years.
Keywords: dental preventive programmes, oral health, childhood and adolescence, DMFT (decayed, missing, filled teeth), effective dental care systems, national surveys, youth dental initiatives, oral health outcomes, middle-age oral health
The main oral diseases, such as caries and periodontitis, while not life-threatening, are often overlooked in health policy discussions. In many countries, dental health is regarded as a marginal issue and frequently neglected in overall healthcare strategies.1 This oversight fails to account for several important factors. First, oral diseases are chronic, in phases progressive, and cumulative in nature,2 affecting significant portions of both children and adults worldwide. Second, traditional dental treatments are costly and the mere quantity of such treatments in the dental sector places a considerable financial burden on societies and healthcare systems. It is estimated that dental care accounts for approximately 5% to 10% of total healthcare costs.3 For instance, in European Union (EU) countries, dental care expenses rank third, following diabetes and heart disease, and even exceed those associated with cancer treatment.4 Third, many common oral disorders are largely preventable, especially when modern dental knowledge and proven methods are employed and when the population has good oral health awareness and is practising proper oral self-care. Then, significant savings in economic resources and enhancements in the overall oral health of the society can be expected.5,6.7
Empirical evidence across the world suggests that different age groups are particularly affected by these major dental diseases throughout their lives.8 The natural history of oral diseases has been described as follows: Primary (baby) teeth are prone to caries after eruption, with prevalence peaking around the age of six.2 The prevalence of caries in permanent teeth also shows a steep increase following eruption, reaching its highest levels in late adolescence or early adulthood. After this peak, the rate of caries remains relatively stable into old age. Severe periodontal disease, defined as deep pockets of more than 6 mm2, typically emerges in early adulthood and increases progressively, peaking around the age of 50. Additionally, total tooth loss (edentulism), begins in middle age and continues to rise steadily into the senior years.2 This empirically deduced model of natural history of oral conditions over an individual´s lifetime is not compelling and occurs only if a person does not get appropriate dental treatment and does not practise sufficient oral self care.
Caries progression is most active during childhood. As individuals reach the end of adolescence, they may begin to experience an accumulation of periodontal diseases. The developmental stages of toddlers, preschoolers, and adolescents, which typically conclude around age 18, might play a crucial role in influencing oral health in later adult life. For example, Heilmann et al. found "good evidence that early childhood is a sensitive period influencing lifelong oral health trajectories".1 They also argue that oral diseases provide an excellent context for applying life course epidemiological research due to their cumulative and chronic nature, their widespread prevalence across populations, and the potential for precise measurement1. Besides, life course studies might help to discover social determinants influencing oral health outcomes. One of the most well-known longitudinal birth cohort study is the since 1972 ongoing Dunedin Multidisciplinary Health and Development Study, whose oral health findings have been published recently.9 Nevertheless, despite some initial attempts to implement such research concepts, the application of life course epidemiology to oral health remains challenging due to a lack of suitable longitudinal data.10
Recent research has increasingly shown that oral health and related behaviours during childhood and adolescence significantly influence oral health in adulthood.11 This influence can even shape an individual's oral health prospects for a lifetime.12 These findings are derived from individually-oriented life course studies that examine the socioeconomic characteristics of preschoolers and their association with oral health in adolescence and adulthood. The results primarily rely on three small prospective birth cohort studies conducted in England, New Zealand, and Brazil.1 However, it is important to note that many of their measures are only categorical.10 Given this context, the conclusion by Heilmann et al. “that traditional preventive approaches, which depend on clinical interventions and simplistic educational support, are ineffective, costly, and likely to increase oral health inequalities within the population“1 seems premature and remains open to debate.
To verify these findings and assessments, we will conduct a reality check by analysing population-oriented long-term clinical epidemiological data from the younger generation. We will then compare these results with clinical outcome data from older adult populations to determine whether the aforementioned connections exist or can be disproven. Additionally, we investigate why some countries exhibit better oral health outcomes than others aiming to identify those countries, respectively dental care system types and to crystallise the reasons behind these differences.
We utilise existing longitudinal clinical oral health data from younger generations, specifically 5 to 6-year-olds, 12-year-olds, 15-year-olds, and 18-year-olds, from selected high-income countries with different dental care systems. By examining the effects of these early oral health outcomes and practises on the dental health of older age groups, we aim to explore how long these habits extend into adulthood and try to identify factors that may have supported or hindered this development. The necessary data is sourced from international organizations such as the World Health Organization (WHO), the Malmö University database, the World Bank, and the Organization for Economic Cooperation and Development (OECD). Additionally, this material is supplemented by research papers from the countries under investigation.
To establish a solid empirical foundation, we selected twelve countries from around the world for analysis. These countries are categorized as high-income by the World Bank, indicating that they are economically similar in terms of development. However, they vary significantly in geographic and cultural conditions, as well as in their dental care systems. To ensure uniform initial conditions among the countries studied, we specifically chose nations where the oral health of adolescents, as measured by the number of Decayed, Missing, and Filled permanent teeth (DMFT), is very low (less than 1.2 DMFT for 12-year-olds) or at least low (DMFT >1,2-2.6), according to WHO standards.
Based on these criteria, the three Nordic countries of Sweden (SE), Denmark (DK), and Norway (NO) exemplify the Nordic welfare system. Great Britain (GB) represents a national health system, while Germany (DE), Japan (JP) and South Korea (KR) showcase social security systems. Australia (AU) and New Zealand (NZ) represent a private/public healthcare system, whereas Switzerland (CH) incorporates a private insurance system. Additionally, Portugal (PT) and Spain (ES) illustrate the Southern European system. Table 1 displays important general characteristics of these countries.
|
Country |
Dental care type |
GDP1/capita, PPP (current intern. $)2 |
Population density (people/sq km) |
Degree of urbanization (%)3 |
|
Sweden (SE) |
Nordic Welfare model |
70,206 |
26 |
88 |
|
Denmark (DK) |
76,688 |
149 |
88 |
|
|
Norway (NO) |
104,460 |
15 |
82 |
|
|
Great Britain (GB) |
National Health model |
58,906 |
286 |
85 |
|
Germany (DE) |
Social security model |
69,338 |
242 |
77 |
|
Japan (JP) |
50,207 |
340 |
92 |
|
|
South Korea (KR) |
54.033 |
530 |
82 |
|
|
Australia (AU) |
Private/public model |
69,115 |
3 |
80 |
|
New Zealand (NZ) |
54,110 |
20 |
87 |
|
|
Switzerland (CH) |
Private insurance model |
92,980 |
226 |
74 |
|
Portugal (PT) |
Southern European model |
48,759 |
114 |
65 |
|
Spain (ES) |
52,779 |
96 |
80 |
Table 1 Characteristics of the selected countries 2024
Reference:13-15
Generally, the delivery models for dental care are organised separately from general health provision and range from public to private schemes.16 The Nordic Welfare model is characterised by high government involvement, easy availability, and tax financing.17 Its public sector is widely school-based and provides preschoolers, schoolchildren and adolescents with comprehensive dental care free-of-charge.16 Adult oral care is mainly provided by private dental practitioners on a fee-for-service basis partly subsidised by national health insurance.16 Great Britain practices a National Health Service model that is tax-financed and provides oral care to the whole population, whereby children until 18 years of age are free of charge and adults´ treatments are subsidised. A growing part of dental care is delivered by dentists under private contracts. The social security models of Germany and Japan are featured by long-established statutory sickness insurance covering 90% of the population in Germany and 100% in Japan.16 Service delivery comes from private dental practitioners, whose treatment fees are negotiated by sickness funds and the dental associations. The public sector, with salaried dentists, is small in Germany and mostly engaged in serving kindergarten- and schoolchildren. In Japan, the public dental activities are regularly conducted by private practitioners on a part-time basis. This model works well and is suggested to be unique for the Japanese oral care system.18 Korea has been implementing its social security model only since 1997. The National Health Insurance (NHI) provides coverage for 96% of the population, although it encompasses only a limited range of dental treatments.19 Australia and New Zealand practice a mixed private/public system. In Australia, individuals are provided by either private or public dental services. For private oral services, people can purchase health insurance. The public sector, financed by the Commonwealth and State governments, serves mainly the low socioeconomic groups and children.20 In New Zealand, the dental system ensures state-funded dental care until the age of 18 years, and adult dental care, generally, has to be privately financed.9
The Swiss dental model is a private system with the possibility of private insurance against dental diseases. Costs for dental care are only covered by the social health insurance system if they were “generated by serious and unavoidable diseases of the masticatory system or by another serious illness or its aftermath“.21 The Swiss legislator considers caries and periodontal diseases to be largely preventable through adequate self-care practices (Federal law on health insurance (KVG), Article 31 from 18th March 1994). Approximately 10% of the population holds private insurance policies,22 indicating that the majority of dental treatments are financed through out-of-pocket expenses.
Portugal and Spain practice the Southern European model, where private dentists provide oral care for the entire population. Government resources or third party payment systems exist only for special population groups. The Spanish public health service offers free dental provision for children up to age 16.23 For people over 16 years of age, dental care is excluded from comprehensive general health care. A small proportion of the adult population (ca. 20%) has private dental health insurance.22 Portugal, having a National Health Service (NHS) that is “tendentiously free,“ implemented in 2005 a Portuguese Public Health Programme (PPOHP) offering fissure sealants, provided by dental hygienists.22 Since 2008, a model of contracting between the NHS and private providers was introduced in dental care24 and a ´dental voucher` was added as a complementing strategy for controlling oral diseases in the younger generation. A specific budget was established by the government, which is yearly continued. For children 3 to 16 years of age, this programme offers regular observation for diagnosis, treatment plan, and basic treatments such as fissure sealing.22
To assess dental caries in primary teeth, we employ the well-established index for decayed, missing and filled teeth (dmft). The prevalence of caries-free status among preschool children is expressed as the percentage of 5/6-year-olds with a dmft of zero. The Significant Caries Index (SiC) serves as a measure of caries risk, specifically identifying the top third of children most affected by caries. For example, a SiC of 3 indicates that, on average, there are three teeth affected by caries present among the top third of preschoolers. This index enables us to evaluate the extent to which social disparities in dental care could be reduced over time. The oral health of permanent teeth is evaluated using the previously mentioned DMFT index. Periodontal conditions are assessed through the Community Periodontal Index (CPI), where a grade of 4 indicates a pocket depth of 6 mm or greater, signifying severe periodontitis. This degree of periodontal disease is recognised as a public health issue and highlights an immediate need for intervention.2
Our macro-level investigation is characterised as a descriptive, observational, and cross-national study that utilises long-term trends obtained from existing epidemiological data across the countries under examination. This approach enables us to identify connections, similarities, or disparities, which will subsequently allow us to present evidence of associations, relationships, and influencing factors. Nevertheless, given the nature of this study, we are unable to establish conclusions regarding causation.
The evaluation commences with the age group of 5 to 6 years, as this is when the prevalence of dental issues in primary teeth reaches its highest point. This assessment illustrates the trends observed over recent decades in the countries being studied. We provide documentation on both prevalence and severity of dental decay by reporting the percentage of cavity-free preschoolers and the degree of caries severity, utilising the dmft index (Table 2).
|
Country |
Indicator |
Data |
||
|
SE |
year |
2010 |
2015 |
2020 |
|
dmft |
0.9 |
1.3 |
0.9 |
|
|
dmft=0 |
80 |
78 |
78 |
|
|
DK |
year |
2006 |
2012 |
2022 |
|
dmft |
1.2 |
0.51 |
0.8 |
|
|
dmft=0 |
- |
- |
78 |
|
|
NO |
year |
2008 |
2015 |
2022 |
|
dmft |
0.8 |
0.7 |
0.7 |
|
|
dmft=0 |
79 |
82 |
81 |
|
|
GB |
year |
1997 |
2003 |
20195 |
|
dmft |
1.7 |
1.5 |
0.8 |
|
|
dmft=0 |
55 |
- |
77 |
|
|
DE2 |
year |
2000 |
2009 |
2016 |
|
dmft |
2.7 |
1.9 |
1.7 |
|
|
dmft=0 |
47 |
52 |
54 |
|
|
JP |
year |
1999 |
2011 |
2016 |
|
dmft |
- |
1.8 |
2.4 |
|
|
dmft=0 |
35 |
50 |
60 |
|
|
KR |
year |
2000 |
2006 |
2012 |
|
dmft |
5.5 |
2.9 |
2.8 |
|
|
dmft=0 |
- |
- |
38 |
|
|
AU |
year |
2000 |
2009 |
2013/14 |
|
dmft |
1.7 |
2.4 |
1.3 |
|
|
dmft=0 |
- |
49 |
65 |
|
|
NZ |
year |
2000 |
2010 |
2022 |
|
dmft |
1.8 |
1.9 |
2.0 |
|
|
dmft=0 |
54 |
57 |
56 |
|
|
CH |
year |
20003 |
20114 |
20214 |
|
dmft |
2.3 |
1.9 |
1.3 |
|
|
dmft=0 |
- |
- |
58 |
|
|
PT |
year |
1990 |
2005 |
2014 |
|
dmft |
4.2 |
2.1 |
1.6 |
|
|
dmft=0 |
- |
50 |
55 |
|
|
ES |
year |
2000 |
2010 |
2020 |
|
dmft |
1.1 |
1.2 |
1.3 |
|
|
dmft=0 |
- |
63 |
65 |
|
Table 2 Long-term trends of caries in deciduous teeth (dmft) and percentage of caries-free (dmft=0) 5/6-year-olds
1.5 years, 2. 6-7years; 3. Canton Zürich; 4. Canton Basel-Land; 5. England, 5-year-olds.
Reference: 18,25,26, 28
The status and advancement of oral health concerning primary teeth are notably favourable in the Nordic countries (SE, DK, NO), and Great Britain, achieving or nearly achieving the WHO target of at least 80% of preschoolers being cavity-free by 2020.27 In most of the other nations, the percentage of caries-free children is on the rise; however, in Korea, the lack of comparative data prevents any assessment of a potential increase in the proportion of caries-free children aged 5 to 6 years. In New Zealand, the score for cavity-free preschoolers has been stagnating during the last 20 years at a modest level of about 55%. While the rates of dental caries have plateaued at a dmft-level of 0.7 to 0.9 in the Scandinavian countries, they are gradually declining in Great Britain, Germany, Switzerland, Portugal, and Korea. However, in Australia, New Zealand and Spain, these rates have remained stable for some time, and even have risen during the last five years in Japan (Table 2). In so far, there is space for improvement in the countries previously mentioned.
The progression of oral health concerning permanent teeth among 12-year-olds in the studied countries is detailed in Table 3. During the 1960s and 1970s, a systematic and extensive effort to control the widespread caries in industrialised nations commenced. This initiative was prompted by a peak in caries experience, for instance among German adolescents aged 13 to 14, with a DMFT score of nearly 9 in the year 1973.29 Switzerland and the Scandinavian nations of Sweden and Denmark were among the first to implement preventive measures aimed at oral health for children and adolescents. Germany followed suit in the 1980s. Initial successes from these programmes were observed less than a decade later. In Switzerland, preventive dentistry efforts began in the Canton of St. Gall as early as the 1950s.30 Significant preventive actions in the 1960s resulted in a reduction of DMFT from 8.1 to 5.3 within the first eight years.31 In Denmark, a stringent preventive strategy was legally enacted in 1972, leading to a notable decline in DMFT for 12-year-olds from 5.2 to 2.0 over a span of thirteen years.32 A similar trend was observed in Sweden, where the number of affected dfs tooth surfaces decreased from 11.2 in 1973 to 5.9 in 1983.33 Subsequently, after the legal introduction of group prophylaxis for children and adolescents in Germany, a significant reduction in caries among 12-year-olds was recorded between 1989 and 1994, with DMFT dropping from 6.4 to 2.4.29 Since that time, the rate of caries decline has slowed but has continued to improve, as illustrated in Table 3 for the past fifteen to twenty years. In the 1990s, dental care prevention in Great Britain gained momentum through the introduction of a hybrid capitation model within the NHS, alongside organised preventive initiatives aimed at schools and underprivileged areas.34,35 In Korea, Portugal and Spain, organised preventive programmes commenced no earlier than approximately the year 2000. Nonetheless, significant decreases in caries prevalence were achieved in all four countries. However, in Korea, the reduction in DMFT levels plateaued at 1.8 between 2012 and 2018. This stagnation in the decline of DMFT is likely attributed to a small, high-risk group that exhibits a relatively elevated SiC value.36 Significant regional disparities in DMFT levels among adolescents, ranging from 1.4 to 2.4, are evident across the Korean metropolitan areas. Consequently, there is a pressing need for targeted preventive programmes aimed at adolescents residing in high-risk areas for dental caries to address the existing backlog in oral health of Korean children.36-38
|
Country |
Indicator |
Data |
||
|
SE |
year |
2001 |
2011 |
2021 |
|
DMFT |
0.9 |
0.8 |
0.7 |
|
|
DMFT=0 |
61 |
65 |
68 |
|
|
SiC |
2.6 |
2.2 |
2.2 |
|
|
DK |
year |
2001 |
2014 |
2022 |
|
DMFT |
0.9 |
0.4 |
0.4 |
|
|
DMFT=0 |
61 |
78 |
79 |
|
|
SiC |
- |
- |
- |
|
|
NO |
year |
2003 |
2013 |
2022 |
|
DMFT |
1.7 |
1.0 |
0.8 |
|
|
DMF=0 |
40 |
60 |
61 |
|
|
SiC |
- |
2.7 |
2.3 |
|
|
GB |
year |
2001 |
2008/9 |
2017 |
|
DMFT |
1.3 |
0.7 |
0.5 |
|
|
DMFT=0 |
- |
- |
77 |
|
|
SiC |
3.2 |
- |
- |
|
|
DE |
Year |
2000 |
2009 |
2016 |
|
DMFT |
1.2 |
0.7 |
0.5 |
|
|
DMF=0 |
52 |
69 |
79 |
|
|
SiC |
3.4 |
2.2 |
1.3 |
|
|
JP |
year |
2000 |
2017 |
2021 |
|
DMFT |
2.7 |
0.8 |
0.6 |
|
|
DMFT=0 |
26 |
65 |
72 |
|
|
SiC |
- |
- |
- |
|
|
KR |
year |
2000 |
2012 |
2018 |
|
DMFT |
3.3 |
1.8 |
1.8 |
|
|
DMFT=0 |
42 |
43 |
93 |
|
|
SiC |
6.1 |
4.5 |
4.9 |
|
|
AU |
year |
2000 |
2009 |
2012/14 |
|
DMFT |
0.8 |
1.1 |
0.9 |
|
|
DMFT=0 |
- |
56 |
62 |
|
|
SiC |
2.5 |
4.8 |
- |
|
|
NZ |
year |
2002 |
2016 |
2022 |
|
DMFT |
1.6 |
0.9 |
0.7 |
|
|
DMFT=0 |
44 |
63 |
69 |
|
|
SiC |
- |
- |
- |
|
|
CH |
year |
20001 |
20111 |
20212 |
|
DMFT |
1.0 |
0.9 |
0.6 |
|
|
DMFT=0 |
- |
63 |
73 |
|
|
SiC |
2.5 |
2.5 |
1.7 |
|
|
PT |
year |
1999 |
2005 |
2013/14 |
|
DMFT |
1.5 |
1.5 |
1.2 |
|
|
DMFT=0 |
- |
44 |
53 |
|
|
SiC |
3.8 |
3.8 |
2.7 |
|
|
ES |
year |
1998 |
2006 |
2020 |
|
DMFT |
1.2 |
1.5 |
0.6 |
|
|
DMFT=0 |
- |
- |
71 |
|
|
SiC |
3.2 |
3.7 |
1.9 |
|
Table 3 Long-term trends of caries in permanent teeth (DMFT), percentage of cavity-free (DMFT=0) teeth and SiC in 12-year-olds
Reference: 25, 26,29, 36, 37,38
It is important to highlight that all countries, except for Korea, where the DMFT of 1.8 is categorised within the low WHO caries range, are classified as having very low caries prevalence. Notably, Portugal is the country that has recently achieved this benchmark. In all the countries observed, there has been a notable increase in the percentage of adolescents free from caries over time. Concurrently, the SiC index has generally decreased in most countries for which data is available, with the notable exceptions of Australia and Korea. In Australia, the SiC index has nearly doubled, indicating a rise in social inequality concerning dental care, while in Korea, it has remained unchanged. Both nations consequently fail to achieve the WHO target for 2015, which aimed to reduce the SiC index for 12-year-olds to below three.38
Overall, the reduction of caries in Denmark is most advanced and appears to have plateaued. With a consistent DMFT of 0.4 over the past decade and about 80% of adolescents being caries-free, the decline in caries seems to be reaching its limit. Unfortunately, data on the SiC values are not accessible. Nevertheless, the decrease in caries prevalence has been observed across nearly all socioeconomic subgroups and municipalities, leaving only a few demographic disparities in underprivileged areas of Denmark.39
In addition to Korea and Portugal, the remaining countries exhibit limited potential for enhancing their DMFT values. A DMFT score of 0.4 may represent the most favourable outcome, as the proportion of individuals in the high risk category is unlikely to reach zero. The most significant advancements are expected to occur in increasing the percentage of caries-free adolescents and in lowering the SiC values, especially in Korea and Portugal. For example, the German Dental Association set a target for 2030 aimed at achieving a caries-free rate of at least 90% among adolescents.40
The transition from adolescence to adulthood is marked by significant physical and neurologic transformations. Additionally, there are notable behavioural changes, such as increased participation in sports, smoking, alcohol consumption, and alterations in eating habits. Furthermore, a greater inclination towards risk-taking behaviours is observed. This period also sees a tendency for young individuals to move towards obesity. These various biological and attitudinal changes can have a considerable impact on oral health.41 It is thus pertinent to examine the trends in oral health among individuals aged 15 and 18 years. In Table 4 the corresponding DMFT values, the proportion of caries-free adolescents, and the available SiC scores, collectively imply a positive progression for these specific age cohorts. To facilitate in evaluating the changes occurring between the ages of 12 and 18 years, we provide only the most recent data at a single time point in Table 4. Regrettably, the required and timely data are not accessible in all countries.
|
Country |
Indicator |
12 years |
15 years |
18 years |
∆ 12/15 absolute |
∆ 12/18 absolute |
DMFT change in % in 12/18 years |
|
SE |
Year DMFT DMFT=0 SiC |
2021 0.7 68 2.2 |
- - - - |
20211 2.2 40 - |
- - - - |
- 1.5 -28 - |
- 314 - - |
|
DK |
Year DMFT DMFT=0 SiC |
2022 0.4 79 - |
2022 0.7 70 - |
2022 1.2 57 - |
- 0.3 -9 - |
- 0.8 -22 - |
- 300 - - |
|
NO |
Year DMFT DMFT=0 SiC |
2022 0.8 61 2.3 |
2022 1.8 45 - |
2022 2.8 32 - |
1.0 -16 - |
2.0 -29 - |
- 318 - - |
|
GB |
Year DMFT DMFT=0 SiC |
2017 0.5 77 - |
2013 1.4 54 - |
- - - - |
- 0.9 -23 |
- - - - |
- - - - |
|
DE |
Year DMFT DMFT=0 SiC |
2016 0.5 70 1.3 |
2012/132 1.5 - 1.9 |
- - - - |
- 1.0 - 0.6 |
- - - - |
- - - -
|
|
JP |
Year DMFT DMFT=0 SiC |
2021 0.6 72 - |
20164 0.6 62 - |
20164 1.9 53 - |
0 -10 |
1.3 -19 |
- 316 - - |
|
KR |
Year DMFT DMFT=0 SiC |
2018 1.8 93 4.9 |
2006 4.2 - 8.3 |
- - - - |
- 2.4 - 3.4 |
- - -- - |
- - - - |
|
AU |
Year DMFT DMFT=0 SiC |
2012/14 0.9 62 - |
2007 2.1 - - |
- - - - |
- 1.2 - - |
- - - - |
- - - - |
|
NZ |
Year DMFT DMFT=0 SiC |
2022 0.7 69 - |
- - - - |
20095 3.7 68 - |
- - - - |
- 3.0 -1 - |
- 528 - - |
|
CH |
Year DMFT DMFT=0 SiC |
2021 0.6 73 1.7 |
2021 0.7 69 - |
20066 3.1 28 - |
0.1 -4 - |
2.5 -45 - |
- 516 - - |
|
PT |
Year DMFT DMFT=0 SiC |
2013/14 1.2 53 2.7 |
2005 3.0 28 6.9 |
2013/14 2.5 32 - |
- 1.8 -25 - |
- 1.3 -21 - |
- 208 - - |
|
ES |
Year DMFT DMFT=0 SiC |
2020 0.6 71 1.9 |
2020 0.9 65 2.8 |
- - - - |
- 0.3 -6 0.9 |
- - - - |
- - - - |
Table 4 Changes in caries prevalence, caries-freedom, and SiC among individuals aged 12, 15, and 18 years around 2020 (or closest available year)
1.19 years; 2. State of Brandenburg; 3. 14 years; 4. 17 years; 5. 21 years (mean of 18-24), 6. 20-year-old recruits.
Reference: 25,26, 39,40,42,43, 44
In several countries, including Sweden. Denmark, Norway, Japan, and Portugal, the caries increase among individuals between age 12 and age 18 is relatively low. This observation holds true for Switzerland as well, particularly since the Swiss values focused on 20-year-olds instead of 18-year-olds. In contrast, New Zealand exhibits more elevated caries increments. The reduction in the percentage of caries-free individuals among 18-year-olds in Sweden, Denmark, Norway, Japan and Portugal is as anticipated, showing a moderate decline of approximately 20 to 30 percentage points. Switzerland, however, presents a more significant decrease of 45 percentage points, although here again it is important to note that this figure pertains to 20-year-olds rather than 18-year-olds. Remarkably, New Zealand shows an exceptionally minimal decline among older adolescents, with only a one percentage point reduction. This figure is particularly striking given that it is based on data from 2009, when the DMFT for this age group was notably high at 3.7 (Table 4). Comparisons of the SiC scores are limited to Germany, Korea, and Spain. In Germany, the SiC scores for 12- and 15-year-olds are quite low, at 1.3 and 1.9, respectively,42 reflecting the effectiveness of caries preventive strategies in this high risk demographic. A similar conclusion can be drawn for Spain, while in Korea, social disparities are more pronounced among 12- and 15-year-olds, with scores of 4.9 and 8.3, respectively.
Taking into account the increase in caries over a 6-year period from age 12 to age 18, it can be observed that Portugal exhibits a two-fold percentage change, while Sweden, Denmark, Norway, and Japan demonstrate a three-fold percentage change. The five-fold percentage change noted in Switzerland and New Zealand is attributed to the inclusion of older age groups, specifically 20 and 21-year-old adults, rather than limiting the analysis to 18-year-olds (Table 4).
As interim conclusion we can state significant advancements in oral health among younger generations, specifically those aged 18 and under, across various high-income countries. This development provides a hopeful basis for older generations to preserve their natural teeth as they age. The extent of this potential effect and the factors that may contribute to it will now be explored with regard to middle-aged adults (Table 5). Our hypothesis suggests that better oral health in individuals aged 18 and younger is positively associated with improved oral health in middle-aged adults, and, to a lesser degree, in older adults. Furthermore, we assume that the length of time adults benefit from preventive programmes during their youth is positively related to better dental outcomes in older age groups.
|
Country |
12 years |
35-44 years |
∆ 12/35-44 |
65-74 years |
∆ 35-44/65-74 |
|
SE DK NO GB DE JP KR AU NZ CH PT ES |
0.7 0.4 0.8 0.5 0.5 0.6 1.8 0.9 0.7 0.6 1.2 0.6 |
6,23 13.5 10.8 11.1 11.2 12.02 5.5 10.31 10.0 11.2 10.4 7.4 |
5.5 13.1 10.0 10.6 10.7 11.4 3.7 9.4 9.3 10.6 9.2 6.8 |
15,4 23.1 21.0 21.4 17.7 19.2 8.74 19.46 24.2 13.45 15.1 15.0 |
9.2 9.6 10.2 10.3 6.5 7.2 3.2 9.1 14.2 2.2 4.7 7.6 |
Table 5 Comparison of DMFT values in 12-year-olds and 35/44-year-olds in selected countries studied, around 2020 or nearest
1.35-54 y; 2. Mean of 35-39/40-44 y; 3. 40 y; 4. 60 y; 5. 73 y; 6. 55-74 y.
References: 25, 26, 46- 49
The modest absolute increases in DMFT values over a span of 28 years in Korea, Sweden, and Spain are particularly significant, with increments of 3.7, 5.5 and 6.8, respectively. This suggests that in these countries, the preventive measures and well-established oral care practices aimed at the younger generation have been sustained into middle age. However, this explanation provided does not apply to Korea and Spain, as noteworthy preventive programmes have only been established since the year 2000. It is challenging to determine the conditions that have resulted in these unexpected outcomes. It will be intriguing to explore whether these unique, unidentified factors have also had an impact on oral health among older age groups. In contrast, most other countries exhibit a DMFT increase ranging from 9 to 11, with Denmark standing out, showing the highest increase at 13.1 (Table 5). This indicates that the leading country for adolescents ranks last among middle-aged adults. Conversely, Korea demonstrates the highest caries prevalence in adolescents but the lowest among middle-aged individuals. However, it is important to note that Korea implemented a nation-wide social security system only very late (1997), covering minimal dental benefits. Since 2009 the dental benefits catalogue has been expanded, albeit still in a limited manner.19 Additionally, while the DMFT value in 12-year-olds was relatively high at 1.8 in 2012 and since then stagnated, it had significantly decreased from 3.3 in 2000,36 reflecting a substantial improvement in a short timeframe. Furthermore, Spain has experienced a moderate increase in DMFT, although dental care for adults over 16 years is not included in comprehensive general health care insurance.23 This suggests that a favourable environment for maintaining dental health seems to exist in Spain. In Portugal, the initial preventive programmes for schoolchildren were introduced in a limited capacity during the 1980s and were only comprehensively expanded between 2005 and 2016.45 Despite this, Portuguese middle-aged adults exhibit an oral health status, measured by the overall indicator DMFT, that is comparable to that of citizens from other nations that have benefitted from a more extensive and prolonged period of preventive dental care during their youth.
Utelising the available real values for DMFT increases among 12-, and 18-year-olds (a duration of six years), we derived hypothetical values for DMFT increases between the ages of 12 and 35/44-year-olds (a span of 28 years when calculating with the mean age of 40 years). We assume a linear progression between the respective age groups. The results are illustrated in Figure 1.
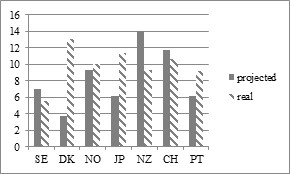
Figure 1 A comparison of projected and real developments of DMFT scores1 among individuals aged 12 and 35/44-years from several countries being studied.
1. Values and calculations from Table 4 and 5.
In Sweden, New Zealand, and Switzerland the real values are lower than the projected values, indicating a significant impact of the excellent oral health of the younger population on the oral health of middle-aged adults. Comprehensive preventive programmes were established in these three nations as early as the 1960s and early 1970s. Denmark, Norway, and Japan initiated their preventive measures for the youth also at an early stage, however, they were not as effective to sustain the beneficial preventive effects into middle-aged adults.
The positive long-term preventive measures and the beneficial oral hygiene habits acquired during childhood and adolescence, should also contribute to improvements in the composition of DMFT scores among middle-aged individuals. Figure 2 examines whether these changes have been observed. In the majority of countries, the D-component is ≤ 1, specifically in Sweden, Denmark, Japan, Korea, Switzerland, Australia, New Zealand, and Spain. The M-component is also minimal in Sweden, Denmark, Japan, Korea, and Switzerland. Notably higher M-values are recorded in Portugal (4.0), Great Britain and Australia (both 3.6) and Germany (2.1). The F-component predominantly prevails in most countries, with the exceptions of Portugal and Australia, as illustrated in Figure 2. The very low D-values, minor M-values and high F-values reflect a significant efficacy of the dental care system regarding accessibility, tooth retention and the restoration of natural teeth. This is particularly evident in Sweden, Denmark, Norway, Japan, Switzerland, and Korea, with Germany, Great Britain, Australia and Spain showing lesser degrees of effectiveness. However, there remains a notable incidence of early tooth loss in Portugal, Great Britain, and Australia. Portugal, in particular, is characterised by high D-, and M-values alongside low F-values, indicating a low effectiveness of its dental care system for middle-aged adults. That contrasts sharply with the rapid improvement in oral health in a short time among younger individuals in Portugal.
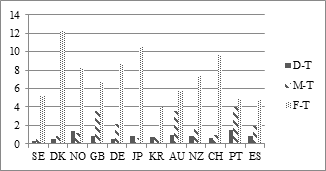
Figure 2 Composition of the DMFT of 35/44-year-olds1,2,3 in the countries under investigation around 2020.
References: 25, 46-48,50-54
Limited research has been conducted on middle-aged individuals and their progression into seniority, despite the fact that periodontal diseases are most common during this stage, with tooth loss beginning in those aged 35- to 44.55 This situation renders individuals susceptible to tooth loss due to issues related to saliva production, which can lead to cavities and gum diseases, thereby increasing the likelihood of tooth loss as one ages.56 Throughout this transition, the count of remaining teeth plays a significant role.55
The increase in caries among middle-aged adults and seniors reveals that Switzerland, Korea, Portugal Germany, Spain and, Japan experienced the lowest absolute increases in DMFT, ranging from 2 to 7 (Table 5). In contrast, Australia, Sweden, Denmark, Norway, and Great Britain exhibited increases between 9 and 10, while New Zealand recorded even a rise of 14,2, suggesting adverse conditions for the dental health of seniors.
When specifically comparing the DMFT scores of individuals aged 65 to 74, it becomes evident that alongside New Zealand, the DMFT values of seniors in Denmark, Britain and Norway are comparatively high (see Table 5). This seems to indicate a less satisfactory dental health status. But, is this the whole truth? Figure 3, illustrating the composition of the single DMFT scores, gives the answer. It reveals that the D-component is well under control in all countries with the exception of Norway and Portugal, where the share of untreated decayed teeth can be improved. However, the decisive differences result from the M- and F-component. Missing teeth are only a minor problem in Sweden, Switzerland and Norway, whereas they are the main problem in Great Britain, New Zealand, Portugal, Spain, Germany, and Korea. In these countries, the M-component significantly exceeds the F-component, suggesting a prevailing focus on restorative and prosthetic treatment approaches. Such treatment philosophy leads to a reduced effectiveness of the dental care system in preserving natural dentition. This approach seems to be particularly pronounced in Portugal, where researchers characterise the adult oral health panorama as bleak.57 The loss of permanent teeth in the Portuguese population is so frequent that 70% of the adult population had lost at least one tooth and 33% more than six teeth. In the age bracket 45 to 65 and over, only about half of the individuals replace their lost teeth, mostly with removable protheses.58 Also, Spain and Korea face the same problem, whereat the level of tooth loss in Korea is less distinct. Striking is the case of New Zealand where both values, the M-, and F-component, are nearly equally high. The extreme favourable proportion of the F-component in relation to the M-component in Sweden, Norway and Switzerland signalises a strict tooth retaining approach in those countries (Figure 3).
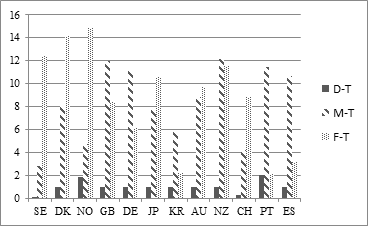
Figure 3 Composition1 of the DMFT in 65/74-year-olds from selected countries studied around 2020 or nearest available year.
References: 25, 49, 51,54, 59, 60, 63
An additional assessment will investigate the validity of these findings. To achieve this, we utilise the proportion of seniors who are edentulous, as this metric reliably reflects the functionality and effectiveness of a country´s dental care system. The current situation is shown in Figure 4.
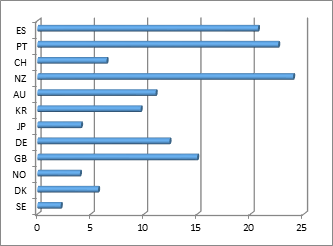
Figure 4 Edentulism in 65/74-year-old individuals1,2,3 (in %) from the observed countries around 2020 (or nearest).
References: 25, 46, 51,61-63
The graphic reveals that edentulism among seniors is no longer a significant issue in Sweden. It is only a minor concern in Norway, Japan, Denmark, and Switzerland. These results for the senior population align with those observed in the middle-aged demographic (Figure 2). Countries such as New Zealand, along with the Iberian Peninsula nations of Portugal and Spain, and to a lesser degree Great Britain, continue to face significant challenges in addressing the issues of high tooth loss and associated edentulism among the elderly population. The significant backlog in tooth loss and edentulism among seniors in Germany and Great Britain is highlighted by German research. It prognoses that it will not be until 2030 that German seniors will attain average tooth loss rates of 5.6 MT and average edentulism rates of 4.2%.64,65 These figures have already been met or surpassed in countries such as Sweden, Norway, Switzerland and Korea for some time. Consequently, Germany and Great Britain are at least 15 years behind the leading nations in senior oral health. The time required for Spain, Portugal, and particularly New Zealand to catch up will be even more extended.
In light of this context, we can address our two hypotheses: The positive impacts of preventive programmes for children and adolescents are particularly evident in Sweden, Korea, and Spain up to the ages of 35 and 44 (refer to Table 5). Additionally, the detailed analysis of the DMFT index among middle-aged individuals reveals that the earlier preventive measures taken for younger populations have also contributed positively to the effectiveness of dental care systems in Denmark, Norway, Japan, and Switzerland. Moreover, it has been demonstrated that the benefits of such programmes are more pronounced in countries that adopted preventive care for the younger generation earlier, as illustrated by the contrasting examples of Sweden, Denmark, Norway, Switzerland, and Japan, compared to Germany, Great Britain, Spain, and Portugal (see Figures 2, 3, and 4).
In the following sections, we will analyse the factors that lead to the differing outcomes observed in the countries under investigation. To offer a concise summary of the essential behavioural and supply-related elements influencing the oral health of the population, we present pertinent data in Table 6. Additionally, we incorporate the CPI 4 for seniors as an indirect measure of the quality of oral hygiene practices.
It is noteworthy that societies with particularly high oral health standards, such as Sweden, Denmark, and Switzerland, exhibit a relatively high per capita sugar consumption (Table 6). This suggests that effective oral health practices and consistent use of dental care services may mitigate the adverse effects of sugar consumption on oral health. However, the significant occurrence of severe periodontitis in Denmark challenges this correlation, implying that the relationship between oral care practices and periodontal health is more intricate than it appears. Similarly, in Norway, despite low sugar consumption and commendable oral hygiene practices, the prevalence of CPI grade 4 among seniors is relatively high at 26.6%. In contrast, Switzerland demonstrates a fairly high per capita sugar intake alongside good oral care habits, resulting in a very low CPI 4. The situation in New Zealand presents further complexity, with extremely high sugar consumption per capita, a low smoking rate, and only average oral care practices, yet it maintains remarkably low incidence of severe periodontitis (<3%). Conversely, in Germany, the combination of high sugar intake and adequate oral health behaviours leads to a significantly elevated prevalence of severe periodontitis among seniors (Table 6). In conclusion, while Sweden and Switzerland consistently exhibit favourable oral health behaviours, many other countries show only average oral care practices, which require enhancement, as evidenced by the high rates of tooth loss and edentulism among the elderly population.
|
Country |
Dentists per 10,000 |
Dental hygienists/- therapists/ per 10,000 |
Sugar consume/ capita (g/day) |
Smokers (%)
|
Tooth brushing in 35-75 y ≥ twice/day |
Dental flossing/ toothpick (%) |
Yearly dental visits 5 25-65+ y (%) |
CPI 4 65/74 y (%) |
|
SE DK NO GB DE JP KR AU NZ CH PT ES |
8.2 7.2 9.3 4.9 8.5 8.3 5.3 6.2 5.0 4.1 11.8 8.5 |
0.43 0.22 0.11 0.71 0.17 13.2 4.93 0.15 1.384 0.28 0.66 1.29 |
92 110 74 82 101 44 77 101 132 114 62 89 |
25 18 17 16 23 27 21 14 14 26 25 28 |
88 68 69 77 86 77 91 9612 66 69 73 66 |
33 39 - 30 48 - 36 5613. - 50 26 - |
556 73 80 63 70 50 3910 4411 - 687 48 40 |
7 20 26.63 - 24.6 17.88 34.29 51.11 <32 3.7 8.6 11.6 |
Table 6 Overview of important factors influencing the oral health status of the population in the countries studied around 2020
References: 25, 38, 46, 47, 51, 52, 58, 61, 66-84
In terms of the supply side and accessibility to dental services, Portugal, the least affluent nation in our survey, exhibits the highest dental density, with 11.8 dentists per 10,000 individuals (Table 6). Conversely, Norway, which also demonstrates a pronounced dental density of 9.3, has many private practitioners expressing concerns over a lack of patients. This situation arises from considerable improvements in oral health over the last 25 years, leading to a notable decline in dental attendance rates and a reduction of over 50% in the number of treatments per dentist.85 The countries with the lowest dental densities include Switzerland (4.1), Great Britain (4.9), New Zealand (5.0), Korea (5.3), and Australia (6.2), where it is important to acknowledge the contribution of dental hygienists and dental therapists to the overall dental workforce. In the remaining countries, dental density varies between 7.2 and 8.5. Notably, in Japan, dental hygienists outnumber dentists, while in Korea, the ratio of dentists to dental hygienists approaches 1:1 (Table 6). Nonetheless, researchers assert that there is a deficiency of dentists in Korea, resulting in numerous underserved regions in smaller cities.37 This highlights the great diversity in the composition of the dental workforce across the countries examined. It is also noteworthy, that Switzerland, with 50% fewer dentists than many other nations, manages to maintain very favourable oral health outcomes for its population.
An additional examination of the financial aspects of various dental care systems provides a comprehensive understanding of the overall situation. When evaluating total dental expenditures on a per capita basis across the surveyed countries, it becomes evident that Norway and Switzerland, the two wealthiest nations, allocate the highest resources to support their dental care systems (refer to Figure 5). Following them, Germany ranks as the third most expensive system. In contrast, Portugal, the least affluent country, allocates the smallest proportion of its resources to dental care. Additionally, Great Britain, Korea, New Zealand and Japan also exhibit relatively low expenditure shares. Notably, the high ratios of dental hygienists and therapists in Japan, Korea, and New Zealand may significantly influence these costs. These findings underscore the substantial impact of a society´s socioeconomic status on the dental care sector, particularly as it relates to income levels as measured by GDP per capita86,87 and the structure of the dental workforce.
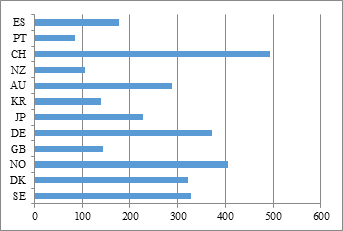
Figure 5 Total outpatient dental costs per capita in US$ in the countries studied, 2019.
Reference: 66
This relationship is further examined in Figure 6. By using Norway, the wealthiest nation, and Switzerland, which has the highest dental spending per capita, as reference points, it becomes evident that Sweden and Japan distribute their financial resources in alignment with their GDP (see Figure 6). Nevertheless, many countries, such as Denmark, Norway, Great Britain, Korea, Australia, New Zealand, Portugal, and Spain invest less in dental care than their GDP would allow. In contrast, only Germany and Switzerland dedicate a larger share of their resources to the dental sector in relation to their GDP.
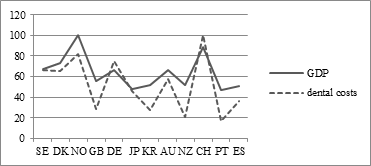
Figure 6 Confrontation of indices for GDP/capita (NO=100) and dental expenditure/capita (CH=100)1 in the countries surveyed, 2019.
When evaluating the total dental expenditures of a country in relation to its GDP, the findings are illustrated in Figure 7. Here, Germany exhibits the highest burden of dental costs, as its GDP is insufficient to accommodate such elevated expenses for dental care. In contrast, the relationship between dental care expenditures and GDP in other countries is significantly more favourable. In other words, the highest per capita spending in Switzerland and Norway is supported by considerably higher GDPs per capita in those nations compared to Germany. These observations can only be derived from the relative measure of dental care costs as a percentage of GDP, which is why this indicator is predominantly employed in macro-level international comparisons.
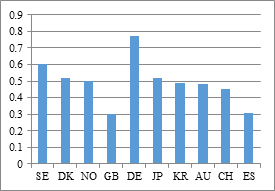
Figure 7 Total dental costs in % of GDP in the countries studied,1 2019.
Reference: 88
Another possible explanation for discrepancies in dental outcomes and the effectiveness of dental systems could be the level of out-of-pocket expenses associated with different dental care systems, along with data regarding unmet dental care needs attributed to financial constraints.
Figure 8 illustrates that, with the exception of Japan and Germany, where out-of-pocket expenses are approximately 25%, the majority of countries exhibit significant out-of-pocket shares ranging from 50% to 70%. In Switzerland, New Zealand, and Spain, these shares can even escalate to between 80% to 98%.
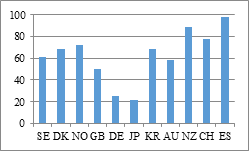
Figure 8 Out-of-pocket payments1 (%) in the observed countries, 2019.
Reference: 89-91
Figure 9 indicates that in most nations, fewer than 10% of patients report unmet dental needs due to financial constraints. However, in Australia and New Zealand, a concerning 40% of adult patients complain that they cannot afford dental services.9,94 The significant prevalence of tooth loss already observed in middle-aged Australians, as illustrated in Figure 2, coupled with the severe tooth loss and the highest rates of edentulism found among elderly New Zealanders, as represented in Figure 3 and 4, seems to indicate a direct correlation with inadequacies in the provision of adult dental care in these nations.
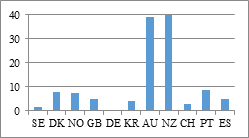
Figure 9 Unmet needs for dental care due to financial constraints (% of patients), 2023.1
References: 92-94
The analysis of oral health development across a population´s life cycle, coupled along with an exploration of potential determinants such as oral behaviour, dental infrastructure, and the characteristics of the dental system, allows for evaluative insights into the performance of the twelve countries surveyed. Notably, all countries observed demonstrated either very good or good oral health status among their youth up to the age of 18, indicating a similar baseline for oral health as individuals transition into adulthood. Over two decades later, the oral health of the middle-aged demographic (ages 35 to 44) and the effectiveness of the dental systems in Sweden, Denmark, Korea, Norway, Japan, and Switzerland surpass those of Germany, New Zealand, Great Britain, Australia, Portugal and Spain in both aspects. By the time, individuals reach senior age, a significant disparity in oral health and system efficacy emerges among the countries. Sweden, Norway, and Switzerland report minimal tooth loss with particularly low rates of edentulism also observed in Japan, and Denmark. In contrast, higher levels of tooth loss are evident among citizens of Great Britain, Germany, New Zealand, Portugal, Spain and Australia. Additionally, the rates of edentulism among seniors in New Zealand, Portugal, Spain, Great Britain, and Germany are notably higher than in the other countries, suggesting that the efficacy of dental care systems in these countries is less favourable. The proportion of out-of-pocket expenses is highest in Spain and New Zealand, at 80% and nearly 100%, respectively, resulting in New Zealand experiencing the most pronounced rate of unmet needs due to costs. However, despite also having high of out-of-pocket payments, Spain and Switzerland report low levels of unmet dental needs for financial reasons. This indicates that the relationship between out-of-pocket expenses and unmet dental needs is more intricate than anticipated, or that the subjective measure of unmet needs may lack reliability due to methodological issues. A representative study conducted in Korea also indicated that 41% of the adult population experienced unmet dental needs attributed to financial constraints.95 In contrast, findings from another study involving 175,000 participants showed a significantly lower rate of unmet needs at 3.7%,96 thereby reinforcing our concerns. Nonetheless, the cases of Norway, Korea, and Denmark illustrate that it is possible for nations to maintain good oral health into advanced age, despite dental sytems necessitating substantial co-payments ranging from 70% to 80%. It is likely that the per capita GDP influences this situation, as individuals in more prosperous societies may find it more feasible to manage such high co-payments.
The macro-level effects of dental care in Germany provide another noteworthy example. The country´s dental system is characterised by the highest cost relative to GDP (0.77%), a low co-payment rate, and average dental health outcomes among the adult population. There is a significant prevalence of tooth loss and edentulism among the seniors, largely due to the continued reliance on invasive treatments for adult dental care.97 The stark contrast between the low number of dental hygienists and the extremely high number of dental technicians highlights the existing imbalance within Germany´s dental sector.7 This situation suggests that there are considerable improvements to be made. This assessment is further reinforced by the observation that many countries with superior oral health among adults allocate only 5% to 6% of their GDP to dental care (Figure 7).
The survey indicates that individuals who receive earlier and more thorough education regarding oral health awareness, oral hygiene practices and regular dental check-ups during their childhood and adolescence are more likely to retain their natural teeth as they age. Additionally, the findings suggest that various types of dental care systems can contribute to high oral health standards across populations throughout their lifetimes, while also demonstrating effective and efficient performance of dental care systems, as evidenced by countries such as Sweden, Denmark, Norway, Japan, and Switzerland. Nevertheless, the notion that care systems can be managed effectively or adequately remains applicable, as illustrated by the experience of Germany, Great Britain, Australia, New Zealand, Portugal, and Spain. Moreover, nations with proactive oral health policies and appropriate monitoring (such as Sweden, Denmark, and Japan), along with those engaged in extensive research on dental health services (including Sweden, Denmark, Japan, Korea, and Switzerland), play a crucial role in enhancing the overall effectiveness of dental care systems.
Comprehensive dental initiatives targeting youth, which commenced in the 1960s, have shown beneficial impacts on oral health throughout adulthood and into old age in countries such as Sweden, Denmark, Norway, and Switzerland. In contrast, nations that introduced regular preventive programmes later, during the 1980s and 1990s or beyond, have observed positive outcomes only within the middle-aged demographic, after which improvements plateaued, as seen in Great Britain, Germany, Korea, New Zealand, Portugal, and Spain. Consequently, in these countries, it is to consider implementing preventive measures for young adults to reinforce the oral health practices established in earlier years. Our findings further indicate that maintaining good oral health is not contingent upon a specific type of dental care, whether it is state-funded, social security-based, or privately-funded. However, the presence of an effective monitoring system for dental health, along with a comprehensive oral health policy that includes clear objectives, significantly enhances the potential for health policy interventions aimed at gradually optimising dental care services. Sweden, Denmark and Japan serve as exemplary models in this context. Regarding the efficacy of dental care systems, there exists a notable variation in treatment philosophies for adults across different countries: some prioritise early detection and a strict tooth retaining approach as seen in Sweden, Denmark, Norway, Japan, and Switzerland, while others tend to overlook early care in favour of more invasive procedures and tooth replacement strategies as observed in New Zealand, Portugal, Spain, Great Britain, Germany, Australia, and Korea.
None.
The author declares that there is no conflict of interest.

©2025 Saekel. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.