Journal of
eISSN: 2373-4345


Research Article Volume 3 Issue 1
1Private practice, Orthodontist and Dentofacial Orthopedist, UAE
2Private practice, Dentist, Iran
Correspondence: Amjad Al Taki, Private practice, Orthodontist and Dentofacial Orthopedist, UAE, Tel 971 508772721
Received: August 18, 2015 | Published: November 13, 2015
Citation: Taki AA, Ghaffarpasand A. Effects of functional appliance therapy on the depth of the pharyngeal airways: activator vs. forsus. J Dent Health Oral Disord Ther. 2015;3(1):261-268. DOI: 10.15406/jdhodt.2015.03.00082
Aims: The aim of this study was to evaluate the changes in Dento-skeletal components following orthopedic therapy of Class II skeletal malocclusions, and to assess the effect of these changes on the depth of the pharyngeal airways, after treatment with removable and fixed functional appliances.
Methodology: 25 adolescents (14 boys and 11 girls, mean age 11.67 years) were chosen. The subjects were divided into two groups according to the treatment type: removable appliance group (13 subjects, 7 boys and 6 girls, mean age 12 years) and fixed appliance group (12 subjects, 7 boys and 5 girls, mean age 11.33 years). Lateral cephalometric radiographs taken before (T1) and after the treatments (T2) were digitally analyzed. Paired t-test was used to determine the possible statistically significant changes (T2-T1) for both groups. Identified differences between the groups were further analyzed using the Mann-Whitney U-test at the 95% confidence interval (P <.05).
Results: Functional appliance therapy showed no statistically significant changes in upper pharyngeal airway depth (UPAD) and middle pharyngeal airway depth (MPAD). Only the lower pharyngeal airway depth (LPAD) was increased significantly (P<.05) due to the forward positioning of the mandible, determined by significant increase in SNB, ANB, and Pog to N perp. Intergroup comparisons showed no statistically significant differences between removable and fixed appliances (P >.05).
Conclusion: Positive sagittal mandibular change, as a result of both types of functional appliances therapy, had a significant increase on the depth of the lower pharyngeal airway.
Keywords: functional appliances, airway, activator, forsus
Functional Appliances, in general, refer to removable or fixed appliances which are designed to change the vertical or sagittal relationships of jaws, mandible in particular. Treatment with these appliances, during the periods of active skeletal growth, has been a widely accepted therapeutic method for class II division I malocclusions1 characterized by mandibular retrognathism.2
Reduction in pharyngeal airway dimensions has been known to be associated with mandibular retrognathism,3 mainly relative to backward posture of soft palate and tongue, which increases chances of certain respiratory problems, such as snoring, and Obstructive Sleep Apnea (OSA).4 Nowadays, several appliances are used similarly in OSA patients to relocate tongue, soft palate, and hyoid bone in an aim to increase pharyngeal dimensions, and to subsequently improve respiratory function during sleep in these patients.5
Before determining whether the depth of the pharyngeal airways in retrognathic Class II subjects could be positively influenced by functional appliances, a more basic concept has to be discussed and clarified, and that is, the nature of the changes that are caused by such appliances. A controversy still exists among numerous authors as to whether the changes are purely skeletal,6,7 purely dentoalveolar,8 or a combination of both.9
In this study we will first assess the skeletal and dental effects of functional appliances in general, and then we will investigate if such treatment effects are comparable among removable versus fixed appliances. Eventually, the main objective of our study, i.e., subsequent effects of these appliances on the dimensions of pharyngeal airways, will be addressed. Having reviewed the literature, there are very few published studies4,10-14 that have investigated the effect of functional appliances on the dimensions of awake pharyngeal airways. Of these studies, four have included either headgear4,10,12 or maxillary expansion11 appliances in combination with functional appliances, and the other two studies have used only removable13 or only fixed14 functional appliances for their treatment effects evaluation.
To our knowledge, this study is the first to evaluate and compare the effects of different removable and fixed functional appliances on the depth of the upper (nasopharyngeal), middle (oropharyngeal), and lower (laryngopharyngeal) airways.
Sample selection
The sample consisted of 25 adolescents (14 boys and 11 girls, average age 11 years 8 months), whose lateral cephalograms taken before (T1) and after the treatment (T2) with functional appliances (total 50) were collected. The lateral cephalometric radiographs were compiled from their clinical records kept at private orthodontic clinic at Ajman University. The study was approved by the Ajman University of Science and Technology (UAE) Ethical Committee.
The inclusion criteria for the sample were:
The sample was then divided into two groups. The first group consisted of the subjects who were treated with removable functional appliances (Activator type), and the second group consisted of those who were treated with fixed functional appliances, Forsus Fatigue Resistant Device (FRD) (3M Unitek Corp, Monrovia, Calif).The sex and age distribution of the treatment groups are shown in Table 1. Although chronological ages appear different between groups, growth stages were closely matched according to cervical vertebra maturation (CVM) assessment on lateral cephalograms.
|
N |
Age(X) |
Min |
Max |
CVM |
Removable appliance group |
|||||
Boys |
7 |
12.57 |
11 |
15 |
CS3 |
Girls |
6 |
11.33 |
9 |
13 |
CS3 |
Total |
13 |
12 |
9 |
15 |
CS3 |
Fixed appliance group |
|||||
Boys |
7 |
11.85 |
8 |
16 |
CS3 |
Girls |
5 |
10.6 |
9 |
13 |
CS2 |
Total |
12 |
11.33 |
8 |
16 |
CS2-CS3 |
Table 1 Age (chronological and vertebral) and sex distribution of treatment groups
N indicates the number of patients; X, age pre-treatment (year); CVM, cervical vertebral maturation stages
The removable appliance group comprised of 13 subjects (7 boys and 6 girls, mean age 12 years), with the duration of treatment ranging from 6 to 15 months with an average of 11.6 months.
The activator appliance used was an acrylic monobloc with clasps used to fixate the appliance to the upper first molars. The appliance was produced from a construction bite that positioned the mandible anteriorly in an edge-to-edge incisal relationship. The lower jaw was postured forward in a Class I or overcorrected Class I molar relationship to stimulate mandibular growth. During treatment, contact was maintained between the appliance and the maxillary posterior teeth. The mandibular posterior teeth were encouraged to erupt by trimming acrylic on the occlusal and lingual aspect. The patients were instructed to wear the appliance a minimum of 14 hours per day.
The fixed appliance group comprised of 12 subjects (7 boys and 5 girls, mean age 11 years 4 months), and the duration of treatment ranged from 3 to 12 months with an average of 6.3 months. All Forsus treated patients were in the permanent dentition at the start of treatment, and they underwent a specific treatment protocol with preadjusted fixed appliances in combination with the FRD. The FRD was applied at the end of the aligning and leveling phase of orthodontic treatment, when a 0.019×0.025-inch stainless-steel arch wire was inserted at both arches. The mandibular arch wire was consistently cinched distal to the molars. In addition, brackets on the lower incisors presented with a torque of -6° to limit the buccal inclination of the lower incisors. The phase with the FRD was undertaken until Class II occlusion was overcorrected to an edge-to-edge incisor relationship.
Cephalometric analysis
A customized computer software (View Box 4, dHAL™, Kifissia, Greece) was used to digitize the lateral cephalograms, and the radiographs were analyzed utilizing the sequence predefined in the program. Databases containing final analytical calibrations were generated for all patients and were transferred to Excel (Office 2010, Microsoft™, WA, USA) for comparison. 21 cephalometric landmarks, 15 angular and linear measurements for skeletal, dental and airway parameters used in this study are illustrated in Figures 1-4.
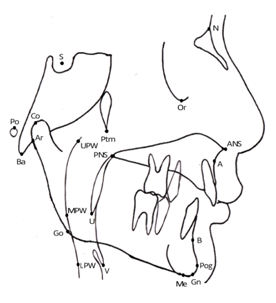
Figure 1 Cephalometric landmarks used in the study.
N, nasion; S, sella; Po, porion; Or, orbitale; Co, condylion; Ar, articulare; Ans, anterior nasal spine; Pns, posterior nasal spine; A, point A; B, point B; Pog, pogonion; Gn, gnathion; Me, menton; Go, gonion; Ptm, pterygomaxillary fissure; Ba, basion; U, uvula; V, vallecula; UPW, upper pharyngeal wall: the intersection of line Ptm-Ba and the posterior pharyngeal wall; MPW: middle pharyngeal wall: the intersection of perpendicular line on Ptm perpendicular from U with posterior pharyngeal wall; LPW, lower pharyngeal wall, the intersection of perpendicular line on Ptm perpendicular from V with posterior pharyngeal wall.
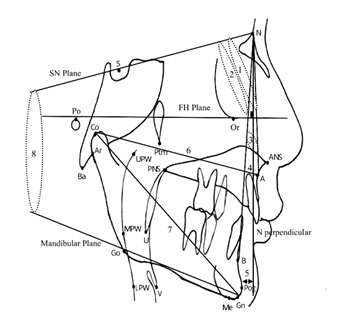
Figure 2 Skeletal cephalometric reference planes: angular and linear measurements used in the study. Reference planes: SN, the line joining S and N; FH plane (Frankfort Horizontal plane): line joining Po and Or; Mandibular plane: line joining Go and Gn; N perpendicular (N perp): perpendicular line on FH plane at N. Angular and linear parameters: 1. SN,: angle between SN and NA line; 2. SNB, angle between SN and NB line; 3. ANB, angle between NA and NB lines; 4. A to N perp: linear distance from A to N perp line; 5. Pog to N perp: linear distance from pogonion to N perp line; 6. Co-A, effective midfacial length: linear distance between Co and A; 7. Co-Gn, effective mandibular length: linear distance from Co to Gn; 8. SN-GoGn, angle between the SN plane and the mandibular plane.
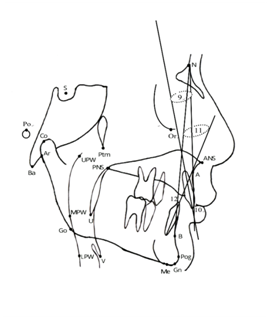
Figure 3 Dental cephalometric angular and linear measurements used in the study (cont’d): 9. U1-NA°, angle between the NA line and line crossing the incisal edge and apex of upper central incisor; 10. U1-NA (mm), distance from the tip of upper central incisor to the NA line; 11. L1-NB°, angle between the NB line and line crossing the incisal edge and apex of lower central incisor; 12. L1-NB (mm): distance from the tip of the lower central incisor to NB line.
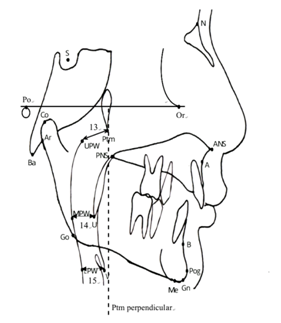
Figure 4 Airway cephalometric reference plane: and linear measurements used in the study. Reference plane: Ptm perpendicular (Ptm perp): perpendicular line of FH plane at Ptm point. Linear measurements (cont’d), 13. UPAD (Ptm-UPW), linear distance between Ptm and UPW; 14. MPAD (U-MPW), linear distance between U and MPW; 15. LPAD (V-LPW), linear distance between V and LPW.
Cephalometric error assessment
In order to evaluate the errors in localization and digitization of the landmarks, about one month after the initial cephalometric analysis, 10 pre or post-treatment radiographs were selected at random from the sample and were rescanned, redigitized and remeasured by the same examiner. Then, the Dahlberg formula was used to estimate the random method errors, and the Forsberg’s formula was used to estimate the systematic errors.
The random method error was found to exceed 0.77ᵒ for G-Sn-Pg' (Facial Convexity), and two other soft tissue measurements G-Sn (HP) (Maxillary prognathism), and G-Pg'(HP) (Mandibular prognathism) were found to have systematic errors exceeding ±2.07 in t value. These errors may well be due to the fact that proper localization of the soft tissue points on cephalometric radiographs is difficult. As a result, all cephalometric soft tissue landmarks and measurements were removed from the study to avoid the anticipated discrepancy in results.
Statistical analysis
The collected data, as a whole, were statistically analyzed by descriptive analysis for mean, range and standard deviation using SPSS software (SPSS for Windows, Release 7.5.1, Chicago, USA).
Sexual dimorphism was compared between the two groups using parametric Student t-tests. The pretreatment cephalometric measurements (T1) of the two groups, and the changes over the treatment (T2) were compared using nonparametric Paired t-tests, after they were subjected to the Kolmogorov-Smirnov test to assess normality distribution of the variables.
In order to evaluate the intergroup differences, the change from T1 to T2 (T2-T1) was compared between the two groups using the Mann-Whitney U-test. The results were regarded as statistically significant at P <.05.
Sexual dimorphism
The results of the independent samples test demonstrated that the mean cephalometric values for the two groups at T1 and T2 did not differ significantly according to gender. Therefore, it was determined that the sexual dimorphism was not present for the two groups, and the sexes were evaluated together.
Treatment effects
Intergroup and intragroup comparisons at T1 (before treatment) and T2 (after treatment), for dento skeletal and airway changes are shown in Tables 2-5.
Intragroup skeletal measures (Table 2): The skeletal measurements related to the maxilla, SNA, A to N perp, and Co-A (effective maxillary length) showed no statistically significant changes between pre-treatment and post-treatment stages.
|
Pre-treatment (T1) |
Post-treatment (T2) |
P |
|
X±SD |
X±SD |
|
Skeletal variables |
|||
SNA |
83.36±3.90 |
82.48±4.78 |
NS |
SNB |
76.40±3.63 |
78.40±3.67 |
** |
ANB |
7.08±1.55 |
4.16±2.19 |
*** |
A to N perp |
0.56±1.23 |
0.36±1.71 |
NS |
Pog to N perp |
-2.80±2.31 |
-0.44±3.77 |
** |
Co-A |
33.92±10.05 |
33.80±8.19 |
NS |
Co-Gn |
40.04±11.69 |
41.0±9.79 |
NS |
SN-GoGn |
27.72±6.09 |
26.88±6.13 |
NS |
Dental variables |
|||
U1-NA° |
24.60±10.18 |
23.2±7.66 |
NS |
U1-NA (mm) |
1.64±1.50 |
1.88±1.05 |
NS |
L1-NB° |
31.44±6.63 |
36.96±6.34 |
*** |
L1-NB (mm) |
2.72±1.88 |
3.08±1.53 |
* |
Table 2 Skeletal and dental pre-treatment and post-treatment variables in the total sample
NS, not significant; *P<0.05; **P<0.01; ***P<0.001
Pertaining to the mandibular skeletal measures, however, it was observed that changes in SNB, and Pog to N perp, from T1 to T2 were statistically significant (P<0.01). In contrast, the effective mandibular length (Co-Gn) and the vertical skeletal measure used in this study (Sn-GoGn) were not influenced significantly, and stayed almost the same after the treatment. This suggests that mandibular sagittal or vertical growth patterns were not positively affected from T1 to T2, however, the antero-posterior position of the mandible, determined by point B or Pogonion could be enhanced by removable or fixed functional treatment.
As a result of change in SNB, ANB was decreased by 2.92 degrees on average, which was considered statistically significant (P<0.001). This means that functional treatment in the subjects was successful in correcting maxillomandibular relationship, i.e., reducing the skeletal Class II discrepancy.
Intragroup dental measures (Table 2, cont’d): The upper central incisor, which was used to evaluate the dentoalveolar changes in the maxilla, showed no significant change in response to treatment. Neither angular (UI-NAᵒ) nor linear (UI-NA (mm)) measurements varied from T1 to T2, indicating that the functional appliances in the sample subjects did not lead to either proclination or retroclination of the maxillary incisors.
In the mandible, a significant increase by 5.52 degrees was noted in the LI-NB angle (P<0.001), followed by a less but significant increase in linear LI-NB (P<0.05). This suggests that the lower incisors were significantly proclined relative to NB in both millimeters and angulation.
Intergroup skeletal and dental comparison (Table 3): All of the skeletal variables related to both maxilla and mandible were comparable between the two groups, meaning no significant differences existed between effects of the treatment by removable or fixed appliances on any of the skeletal parameters.
|
Removable appliance group |
Fixed appliance group |
P |
|
X±SD |
X±SD |
|
Skeletal variables |
|||
SNA |
-1.15±3.93 |
-0.75±.52 |
NS |
SNB |
2.08±3.33 |
1.92±2.94 |
NS |
ANB |
-3.15±2.23 |
-2.67±1.61 |
NS |
A to N perp |
0.00±2.12 |
-0.33±1.56 |
NS |
Pog to N perp |
3.08±3.84 |
1.50±.23 |
NS |
Co-A |
0.92±5.44 |
-0.92±4.91 |
NS |
Co-Gn |
3.00±6.34 |
2.50±5.20 |
NS |
SN-GoGn |
-0.15±4.34 |
-1.67±4.01 |
NS |
Dental variables |
|||
U1-NA° |
-2.54±6.74 |
1.17±.46 |
NS |
U1-NA (mm) |
0.00±1.63 |
0.67±1.83 |
NS |
L1-NB° |
4.08±5.84 |
6.83±7.40 |
NS |
L1-NB (mm) |
0.31±0.95 |
0.42±0.90 |
NS |
Table 3 Comparison of the skeletal and dental treatment changes (t2-t1) between the two groups
Also, the effect of treatment on dental showed no significant difference between the two groups, giving the indication that both types of appliances produced similar influence on the teeth in both jaws.
Intragroup and intergroup airway measurements (Tables 4,5): The upper pharyngeal airway depth (UPAD) and the middle pharyngeal airway depth (MPAD) did not change significantly after the treatment, while the value for the lower pharyngeal airway depth (LPAD) was measured to be significantly different from T1 to T2 (P < 0.05). Between the two groups, all pharyngeal airway dimensions (UPAD, MPAD, and LPAD) were comparable among the group subjects, meaning removable and fixed appliances acted on the pharyngeal airways in a similar manner.
|
Pre-Treatment (T1) |
Post-Treatment (T2) |
P |
|
X±SD |
X±SD |
|
Airway variables |
|||
UPAD |
5.08±1.80 |
4.84±1.91 |
NS |
MPAD |
3.96±1.77 |
4.20±1.80 |
NS |
LPAD |
5.16±1.97 |
6.24±2.71 |
* |
Table 4 Airway pre-treatment and post-treatment in the total sample
|
Pre-treatment (T1) |
Post-Treatment (T2) |
P |
|
X±SD |
X±SD |
|
Airway Variables |
|||
UPAD |
-0.23±2.09 |
-0.08±1.00 |
NS |
MPAD |
0.46±1.51 |
-0.25±0.87 |
NS |
LPAD |
0.62±1.94 |
1.33±2.02 |
NS |
Table 5 Comparison of the airway treatment changes (t2-t1) between the two groups
In this study we aimed to evaluate the nature of changes produced using different types of functional appliances. Because the pharyngeal airway is situated between the bony structures of the cervical vertebra and the facial skeleton, we proposed that the depth of this hollow tube would be dictated by the antero-posterior position of the facial bones. In other words, if orthopedic treatment with functional appliances can stimulate growth of, or induce the forward position of the maxillo-mandibular complex, they would positively affect the airway patency in individuals.
Skeletal changes
In this study, no significant change in the vertical facial pattern was noted, indicated by the orientation of the mandibular plane in relation to the cranial floor (SN-GoGn). This result was in agreement with several authors,8,16 who found no evidence of increased facial height during treatment with various functional appliances. There were no significant differences between the removable and fixed appliance groups, which suggest that increase in the skeletal vertical dimension should be related to growth rather than to treatment with different types of functional orthopedics.17
Concerning skeletal sagittal changes, this study revealed no significant change in any of the three variables used to evaluate maxillary growth or position, either in the total sample or in groups. These results were in agreement with many other authors who evaluated treatments with FR2,18 Herbst,19 Twin Block20 and Jasper Jumper21 appliances.
In the mandible, our results showed that correction of the Class II malocclusion in the subjects was achieved with significant increase in SNB, caused by positive forward movement of point B and pogonion, without any increase in the length of the mandible. This was in agreement with Baccetti et al.22 who noticed forward movement of pogonion, and Patel et al.23 who found forward movement of pogonion and B point. On the other hand, other studies6,7 have found that such therapy resulted in the stimulation of mandibular growth. However, their results have been either based on studies done on animals, or based on very small sample sizes.
Dentoalveolar changes
The study showed that upper incisors did not show any changes to treatment with functional appliances, and the results were comparable between removable and fixed appliance groups. This is against other investigators who claim that functional appliances produce lingual tipping of the upper incisors.16,21
Nevertheless, the lower incisors were proclined considerably in all subjects following the treatment. This effect is probably attributed to the consequent downward and forward force on the lower incisors induced by the protrusion of the mandible. This finding corroborates other studies that used the Frankel,18 Herbst7 and Jasper Jumper.21
Airway changes
Owing to their location, the pharyngeal airways have important roles in both respiratory and digestive systems. Hence, any change in their dimensions would manifest in the efficiency of the deglutition or respiration functions carried out by them.
Upper Pharyngeal Airway Depth (UPAD): The depth of the nasopharyngeal airway in the sample subjects did not show any significant change between T1 and T2 stages of the treatment. Previous study carried out by Mergen et al.24 did not report any differences in the nasopharyngeal dimensions among subjects with different maxillo-mandibular relations, reporting that the dimensions of the bony nasopharynx are relatively independent of other dimensions of the facial complex. Therefore, no effect has to be attributed to the functional appliances, either fixed or removable, as they relate to influencing the upper airway depth.
Middle Pharyngeal Airway Depth (MPAD): The oropharyngeal airway dimensions are dictated by the thickness and length of the soft palate. Jena et al.25 found out that in subjects with mandibular retrognathism the length of the soft palate increases as a result of the backward position of the tongue, which compresses the soft palate and results in decreased thickness and increased length of the soft palate. Muto et al.3 also reported a similar observation. Moreover, Kurt et al.26 concluded that the decreased airway dimension in the soft palate area was due to increased soft palate volume and must be taken into consideration in treatment planning of OSA patients. The unchanged middle pharyngeal airway depth in our study suggests that following the treatment, the increase in thickness and the resulting decrease in length of the soft palate did not occur, and therefore the MPW remained the same despite forward positioning of the mandible. In support were findings of Abu Allhaija et al.27 who found comparable oropharyngeal airway depths among Class II subjects with retrognathic mandibles to Class I subjects with normal mandibles.
Lower Pharyngeal Airway Depth (LPAD): The laryngopharyngeal or hypopharyngeal airway depth is maintained by both tongue root and hyoid bone. Yamaoka et al.28 found that the tongue root was situated more posteriorly in Class II females subjects compared with Class III ones. Also, the change in hyoid bone position and lower pharyngeal airway space caused by anteroposterior position of the mandible is well documented.29
In our study the depth of the inferior pharyngeal airway was increased, and had a significant correlation with the changes in SNB angle, ANB angle, and the distance from Pog to N perp. These results suggest that as the mandible was anteriorly positioned in our subjects, the tongue root was positioned more anteriorly away from the posterior pharyngeal wall, the hyoid bone as well was positioned more anteriorly, and as a consequence, the lower pharyngeal airway was widened.
Our result agrees with those of previous studies29,30 that also reported that a wider lower pharyngeal airway resultant from anterior positioning of the mandible in his their subjects.
Limitations of current study
The lateral radiographs have been used as tools for evaluation of airway size. Since, however, much of the retro-glossal pharyngeal information is missing from the anteroposterior two-dimensional view of these films, a better and more accurate analysis of pharyngeal tissues can be obtained with the use of more comprehensive methods, such as MRI or CBCT.
The skeletal, dental and airway effects produced by removable and/or fixed functional appliances are as follows:
The authors declare no conflict of interest.

©2015 Taki, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.