Journal of
eISSN: 2373-4345


Case Report Volume 9 Issue 4
1Department of Dental Surgery, Kyrgyz-Russian Slavic University in Bishkek, Kyrgyzstan
2Department of Internal Diseases, Kyrgyz-Russian Slavic University in Bishkek, Kyrgyzstan
Correspondence: Sabirova AI, Sabirova A.I, PhD student, Department of Dental Surgery, Kyrgyz-Russian Slavic University in Bishkek, Kyrgyzstan
Received: September 01, 2018 | Published: November 29, 2018
Citation: Sabirova AI, Mamytova AB, Sabirov IS. Correlation of the cytokine status, arterial stiffness and oral health status in patients with the metabolic syndrome. J Dent Health Oral Disord Ther. 2018;9(4):298-301. DOI: 10.15406/jdhodt.2018.09.00396
Ameloblastoma are benign tumors whose importance lies in its potential to grow into enormous size with resulting bone deformity. They are typically classified as Unicystic, multicystic, peripheral and malignant subtypes. Unicystic ameloblastoma (UCA) refers to those cystic lesions that show clinical, radiographic, or gross features of an odontogenic cyst, but on histological examination show a typical ameloblastomatous epithelium lining, with or without luminal and/or mural tumor growth. We present a very rare case of Unicystic ameloblastoma in girl child with an age of 10 years, clinical and radiographic features of UCA, its differential diagnosis, histopathology and current concepts of management has also been discussed in the presenting paper.
Keywords: ameloblastoma, computed tomography, imaging of ameloblastoma, Unicystic ameloblastoma
Ameloblastoma is the most common benign odontogenic tumor accounting for approximately 1% of tumors and cysts of the jaw and 10% of all the odontogenic tumors.1 It is a slow-growing, persistent and locally aggressive neoplasm that may originate from the epithelium involved with the formation of teeth such as enamel organ, odontogenic rests of Malassez, reduced enamel epithelium and odontogenic cyst lining.2 Ameloblastoma may occur centrally within the bone or peripherally, without an intraosseous component in the soft tissues overlying the alveolar ridge. Intraosseous lesions are of two types solid/conventional/multicystic and unicystic.3 Unicystic Ameloblastoma (UA), a variant of ameloblastoma first described by Robinson & Martinez4 in 1977, refers to those cystic lesions that show clinical and radiologic characteristics of an odontogenic cyst, but in histologic examination, show a typical ameloblastomatous epithelium lining part of the cyst cavity with or without luminal and/or mural tumor proliferation. Prior to the report by Robinson and Martinez, this variant had been referred to as a mural or intraluminal ameloblastoma. Recognition of this growth pattern is very important because of its Unicystic radiographic appearance, histologic findings, association with an unerupted tooth, occurrence in the mandible of younger patients, and a recurrence rate after conservative surgical treatment lower than that of its conventional counterpart.5 We present a case of a Unicystic ameloblastoma in a 10-year-old child patient who reported with a complaint of swelling of her right lower jaw.
A ten year old female child came with a complaint of swelling on right lower side of her jaw since one month which was insidious in onset and got gradually progressed to present size. It was associated with severe, intermittent and dragging type of pain which radiates to right ear. Pain relieved with medication. It was also associated with extra oral swelling since15 days. On Extraoral examination facial asymmetry was seen in the right lower third of the face. On Intra oral examination, a solitary diffuse swelling was seen in the buccal vestibular region of 85 and 46, extending anteroposteriorly from middle third of 85 to distal surface of 46. Superoinferiorly 0.5cms below the marginal gingiva of 85 and 46 extending into the buccal vestibule with vestibular obliteration. Sinus opening with pus discharge was seen on the attached gingiva of 85 (buccal or lingual). On palpation, swelling was tender, hard in consistency, non-compressible, non-reducible. Expansion of buccal cortical plate was felt irt 85 and 46. Based on the history and clinical examination a provisional diagnosis of ameloblastoma was made. Under differential diagnosis ameloblastic fibroma, odontogenic keratocyst was considered. IOPA, Occlusal view, Orthopantanogram and CT scan was taken. IOPA taken irt 85 and 46 (Figure 1) showed diffuse radiolucency distal to 46 with absence of 47 tooth bud. OPG (Figure 2) view showed a solitary, well defined radiolucency of size 3x2cms extending anteroposteriorly from mesial root of 46 to 1cm from the posterior border of ramus of the mandible, superoinferiorly 1cm below the sigmoid notch to inferior border of mandible thinning the inferior cortical margin. Internal structure was radiolucent with the displaced tooth bud of 47 in the ramus region. Panoramic CT section (Figure 3) and Sagittal CT section (Figure 4) is showing hypodense area of size 2.5x3cms surrounding the developing tooth bud of 47. Axial CT section (Figure 5A) showing tooth within the hypodense area and axial CT section (Figure 5B) showing buccal cortical plate expansion with breakdown of lingual cortical plate. An incisional biopsy was done and it showed epithelial lining with ameloblast like cells and adjacent connective tissue stroma. There was no luminal proliferation of epithelium, suggestive of intra luminal ameloblastoma (Figure 6). Following the diagnosis, the parents were informed about the condition and proposed treatment. Surgical enucleation along with chemical cauterization with Carnoy’s solution (Figure 7) was done under general anesthesia along with extraction of 47 (Figure 8) considering age of the patient. Patient is under follow up, with no functional or aesthetic complaints. 6 months post treatment OPG shows signs of new bone formation (Figure 9).
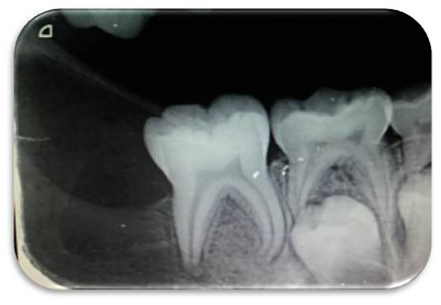
Figure 1 Intraoral periapical radiograph showing diffuse radiolucency distal to 46 with the absence of 47 tooth bud.
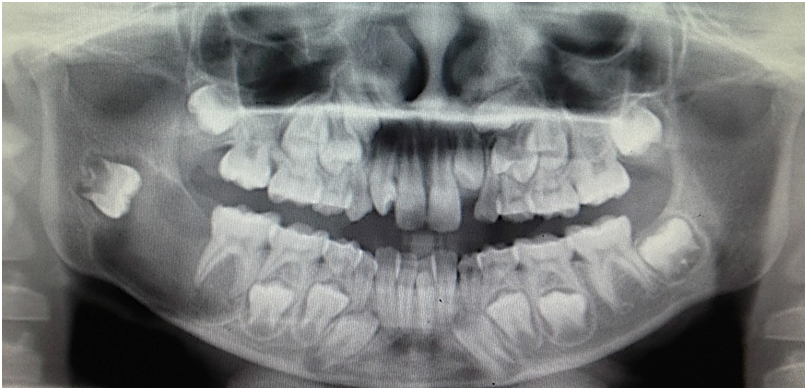
Figure 2 Pre-op OPG showing solitary, well defined radiolucency of size 3x2cms surrounding the crown of 47 tooth bud which got displaced into the ramus region with thinning of inferior border of mandible.

Figure 5 (A) Axial CT section showing tooth within the hypodense area.
Figure 5 (B) Axial CT section is showing buccal cortical plate expansion with breakdown of lingual cortical plate
UA accounts for 6% to 15% of all intraosseous ameloblastomas.1 It is less aggressive, usually occurs in an earlier age group than the solid or multicystic with about 50% of the cases occurring in the second decade of life. As in the present case more than 90% are located in the mandible.6 In most cases UA are associated with impacted tooth, mandibular third molar being the most common.7 The term unicystic is derived from the macroscopic and microscopic appearance, the lesion being essentially a well-defined, often large monocystic cavity with a lining, focally but rarely entirely composed of odontogenic (ameloblastomatous) epithelium.8 The pathogenesis of cystic ameloblastomas remains obscure. Some investigators believe that UCA arises from pre-existing odontogenic cysts, in particular a dentigerous cyst, while others maintain that it arises de novo. The reason why some ameloblastomas become completely cystic may be related to epithelial dysadhesion (e.g., defective demosomes) or, more likely, to the intrinsic production of proteinases (e.g, metalloproteinases, and serine proteinases); enzymes that normally degrade the central zone of the enamel organ after tooth development.9 Radio-graphically, the unilocular: multilocular ratio is 13:3 when the lesion is associated with an impacted tooth. For the `non-dentigerous' variant this ratio changes to 8:7. Further, the `dentigerous' type occurs on average 8 years earlier than the `non-dentigerous' variant. Lastly, the mean age for unilocular, impaction-associated UAs is 22 years, whereas the mean age for the multilocular lesion unrelated to an impacted tooth is 33 years.7 Ackerman et al.,10 classified unicystic ameloblastoma into three types with prognostic and therapeutic implications.
Group I: Luminal UA (tumor confined to the luminal surface of the cyst).
Group II: Intra luminal/plexiform UA (nodular proliferation into the lumen without infiltration
of tumor cells into the connective tissue wall).
Group III: Mural (invasive islands of ameloblastomatous epithelium in the connective tissue wall not involving the entire epithelium).
The microscopic pattern that exhibits mural invasion in UA suggests a more aggressive potential.11
Another histologic subgrouping by Philipsen & Reichart12 has also been described as follows:
The Unicystic Ameloblastomas diagnosed as subgroups 1 and 1.2 can be treated conservatively (enucleation), whereas subgroups 1.2.3 and 1.3 showing intramural growths require radical resection, as for a solid or multicystic ameloblastoma. Following enucleation, vigorous curettage of the bone should be avoided as it may implant foci of ameloblastoma deeper into bone. Chemical cauterization with carnoy’s solution13 is also advocated for subgroups 1 and 1.2. Subgroups 1.2.3 and 1.3 have a high risk for recurrence, requiring more aggressive surgical procedures.14 Recurrence rates for Unicystic Ameloblastoma after conservative surgical treatment (curettage or enucleation) are generally reported to be less than 25%. For intraluminal and plexiform type of Unicystic Ameloblastoma recurrence rate was found to be as low as 10.7%.15 Recurrence rates for Solid Multicystic Ameloblastoma was found to be about 50 to 90%. The present analysis included only publications in English. All well-documented publications during the last 20 years were collected, and several clinicopathological features of each case were studied. The following data were recorded: age (less than or equal to 10 years), sex, location, clinical features/symptoms, histological type, radiographic appearance, treatment. Included only reports of Unicystic ameloblastoma in children less than 10 years confirmed by histological analysis with all the data required for tabulation were included and the Articles not having enough information were excluded (Table 1).
S. no |
Year |
Author |
Sex |
Age |
Location |
Clinical features |
Histological features |
Radiological features |
Treatment |
1 |
1998 |
Li et al.16 |
10 |
F |
Mandible |
Mild fullness over the cheek |
Unicystic ameloblastoma |
UL |
Enucleation |
2 |
2000 |
Li et al.17 |
5 |
M |
Maxilla (premolar to second molar) |
Cystic lesion |
Mural type |
INA |
Enucleation |
3 |
2003 |
Al-Khateeb & Ababneh18 |
9 |
F |
Mandible |
Painless swelling |
Unicystic ameloblastoma |
UL |
Enucleation plus peripheral ostectomy |
4 |
2007 |
Huang et al.19 |
9 |
M |
Body–angle of the mandible |
INA |
INA |
UL |
Enucleation and peripheral ostectomy |
5 |
2008 |
Qureshi et al.20 |
10 |
F |
Mandible |
Mild fullness over the cheek |
Unicystic ameloblastoma |
UL |
Enucleation, curettage |
6 |
2008 |
Gulten U et al.21 |
8 |
M |
Right Mandible |
painless hard swelling |
unicystic ameloblastoma |
UL |
Enucleation and extraction of related teeth |
7 |
2011 |
Chacko & Kuriakose22 |
9 |
M |
Mandible |
Pain and swelling in relation to the right side of the lower jaw |
Plexiform unicystic ameloblastoma |
UL |
Enucleation,curettage |
8 |
2011 |
Kalaskar et al.23 |
9 |
M |
Right maxilla |
Painless swelling |
Unicystic Ameloblastoma with Intra luminal proliferations |
UL |
Enucleation+ Carnoy’s solution and extraction of related teeth |
9 |
2011 |
Ponniah24 |
8 |
F |
Left ramus of the mandible |
Painless swelling on the left side of the mandible |
Unicystic ameloblastoma |
UL |
Enucleation then segmental resection |
10 |
2011 |
Sudhakar K Reddy et al.25 |
6 |
F |
Anterior mandible |
Slow growing painless swelling |
Unicystic ameloblastoma |
UL |
Enucleation and extraction of related teeth followed by application of Carnoy's solution |
11 |
2012 |
Scariot et al.26 |
9 |
F |
Right mandibular body |
Painless swelling |
Plexiform unicystic ameloblastoma |
UL |
Curettage with extraction of two adjacent teeth |
12 |
2013 |
Bhutia O et al.27 |
5 |
M |
Right Mandible |
painless hard swelling |
type 1 unicystic ameloblastoma |
UL |
Enucleation of the cyst with extraction of the involved teeth followed by application of Carnoy's solution |
13 |
2013 |
Arora S et al.28 |
3 |
F |
Left Maxilla |
Bony hard swelling |
Unicystic ameloblastoma (Type 1.2) |
UL |
Enucleation of the cyst with extraction of the involved teeth |
14 |
2014 |
Present case |
8 |
F |
Right Mandible |
Swelling with mild pain |
Unicystic ameloblastoma |
UL |
Enucleation with chemical cauterization |
Ameloblastomas in children differ from adults with a higher percentage of unicystic tumors. Unicystic ameloblastoma is a tumor with a strong propensity for recurrence, especially when the ameloblastic focus penetrates the adjacent tissue from the wall of the cyst. Although enucleation has been claimed to give acceptable recurrence rates in unicystic ameloblastoma, there are no large series with long follow-up in children. The histologic pattern that exhibits mural invasion in unicystic ameloblastoma suggests that more aggressive surgery is necessary. Present case was treated with Carnoy’s solution along with the enucleation, which suggests a possible benefit against recurrence.
None.
The author declares that there is no conflict of interest.

©2018 Sabirova, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.