Journal of
eISSN: 2373-4345


Case Report Volume 16 Issue 2
1Department of Oral Surgery, University Hospital Farhat Hached Sousse, Tunisia
2Research Laboratory LR 12SP10, Functional and Aesthetic Rehabilitation of Maxillary, Tunisia
3Pathology Department, Farhat Hached Hospital, Medicine University, Tunisia
Correspondence: Chaouachi Wided, Department of Oral Surgery, University Hospital Farhat Hached Sousse, University of Sousse, Tunisia
Received: April 14, 2025 | Published: May 8, 2025
Citation: Chaouachi W, Bouslama G, Ghanmi F, et al. Conservative management approach of a large maxillary odontogenic keratocyst: a case report. J Dent Health Oral Disord Ther. 2025;16(2):46-49. DOI: 10.15406/jdhodt.2025.16.00642
The odontogenic keratocyst (OKC) is one of the most aggressive odontogenic cysts, primarily due to its high recurrence rate and potential for local tissue invasion. Originating from remnants of embryonic dental tissues, OKCs are mainly located in the jaw and often remain asymptomatic for extended periods, which can lead to delayed diagnosis. The optimal management of OKCs remains a subject of ongoing debate, with no universally accepted treatment protocol. In this report, we present a case of a 43 years old female patient with no significant medical history that presented with a large OKC in the maxilla diagnosed through clinical, radiological, and histological aspects. The lesion was managed with two-step approach consisting of decompression followed by enucleation. The patient was monitored over an 18-month period, with CBCT evaluations conducted at 6 and 18 months, showing no signs of recurrence. This case highlights the benefits of the two-step procedure in the management of OKCs.
Keywords: odontogenic keratocyst, maxilla, decompression, enucleation, case report
The odontogenic keratocyst (OKC) is one of the most aggressive odontogenic cysts, primarily due to its high recurrence rate and potential for local tissue invasion. Originating from remnants of embryonic dental tissues, OKCs are predominantly found in the jaw and often remain asymptomatic for extended periods, leading to delayed diagnosis.1
Historically, OKCs were classified as benign neoplasms rather than conventional cysts due to their aggressive behavior, high recurrence rates, and genetic associations, particularly mutations in the PTCH1 gene, which is linked to Gorlin-Goltz syndrome. However, in 2017, the World Health Organization (WHO) reclassified OKCs as odontogenic cysts, citing insufficient evidence to support their designation as a distinct neoplastic entity.2 This classification was reaffirmed in the 2022 WHO update, wherein OKCs were categorized under "Developmental Odontogenic Cysts," maintaining their nomenclature as “odontogenic keratocysts”.3
The optimal management of OKCs remains a subject of ongoing debate, with no universally accepted treatment protocol. For large OKCs, enucleation as a single-step procedure may result in substantial aesthetic and functional morbidity, adversely affecting the patient's quality of life. Alternatively, decompression-a conservative approach- aims to reduce cyst size but carries inherent limitations, such as the risk of recurrence due to retained microcysts and the necessity for prolonged treatment and patient compliance. A two-stage approach, incorporating initial decompression followed by surgical enucleation, has emerged as a promising alternative. This strategy facilitates cyst size reduction, promotes bone regeneration, and enables less invasive removal of residual cystic tissue. By mitigating recurrence risks while preserving anatomical structures, this approach enhances treatment efficacy and improves patient outcomes.
This case report presents the diagnosis and staged management of a large OKC in the maxilla, highlighting the advantages of a two-step therapeutic approach.
A 43-year-old female patient was referred to our oral surgery department for evaluation of a well-defined radiolucent lesion in the anterior maxillary region, incidentally discovered during a radiological examination (Figure 1). The patient was in good general health, with no significant medical or family history.
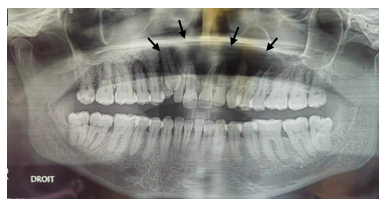
Figure 1 Panoramic radiograph: image of radiolucent cystic appearance, well limited, extended of 12 to 26.
Clinical examination revealed a mild, soft swelling in the left vestibular region without any signs of pain or infection, raising suspicion of vestibular cortical bone perforation. All teeth in the affected region were vital and free from caries. A fine needle aspiration was performed, yielding a whitish, caseous material rich in keratin, effectively ruling out an inflammatory cyst. Orthopantomogram imaging revealed a well-defined radiolucency extending from the maxillary incisor region to the contralateral right premolar-molar area.
A cone beam CT scan (CBCT) confirmed a well-defined hypodense lesion in the maxillary region. The vestibular cortical bone was displaced and ruptured in several areas, with evidence of compromised integrity of the nasal and sinus floor (Figure 2).
Based on the patient's medical history, clinical evaluation, radiological findings, and aspiration cytology, a provisional diagnosis of OKC was established.
Regarding the large extension of the lesion associated to cortical rupture of the sinus and nasal floor, a staged surgical approach was undertaken, involving cyst decompression with drain placement (Figure 3). A biopsy of the cystic lesion was obtained and sent for histopathological examination. Microscopically, the specimen revealed a cystic cavity lined by stratified squamous keratinized epithelium with a dense connective tissue wall. At low magnification, the cystic lumen was observed to be lined by parakeratinized stratified squamous epithelium. The epithelial lining consisted of five to seven cell layers, consistent with the characteristic thickness of OKCs. Palisading of the basal cells was noted, further supporting the diagnosis. These histopathological features confirmed the final diagnosis of parakeratinized OKC.
The patient was instructed to irrigate the cystic cavity daily through the decompression device using a saline solution.
A radiological follow-up after four months revealed the onset of bone trabeculation at the cystic periphery, along with the formation of a thin bony capsule at the nasal and sinus floor (Figure 4), which was the primary decompression goal.
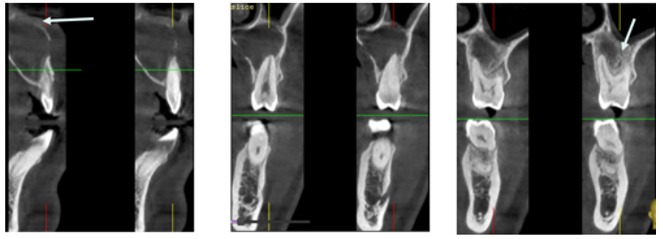
Figure 4 CBCT 4 months after decompression showing formation of a thin bony layer at the nasal and sinus floor.
The enucleation procedure, associated with peripheral osteotomy, was then performed (Figure 5) to remove the pathological tissue and significantly reduce the risk of recurrence.
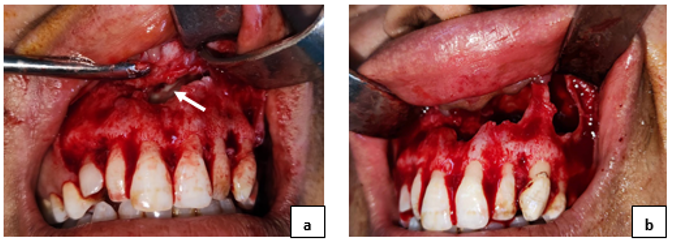
Figure 5a and 5b Intraoral view
b. Intraoperative aspect of the lesion after enucleation.
Histopathological analysis revealed metaplastic transformation of the keratocyst's parakeratinized epithelium into stratified squamous epithelium. At six months postoperatively, clinical and radiological assessments demonstrated satisfactory mucosal (Figure 6) and bone healing (Figure 7).
OKC previously known as the epidermoid cyst, originates from the remnants of the dental lamina or the proliferation of epithelial rests. It accounts for 10–20% of all jaw cysts.4 This condition is most commonly observed in individuals during their second and third decades of life, though it may appear earlier when associated with basal cell nevus syndrome. While OKCs can develop anywhere in the jaws, they predominantly occur in the ascending ramus of the mandible.5 The present case describes a rare occurrence of OKC in the maxillary incisor region, crossing the midline.
Clinically, OKCs are often asymptomatic and are typically detected during routine radiographic examinations. However, they may present with pain, swelling, tooth displacement, or loss of pulpal sensitivity. A key feature of OKCs is their tendency to grow along the internal aspect of the jaws, resulting in minimal cortical expansion.6 In this case, slight cortical expansion was observed, with the lesion extending mesiodistally into the sinus and nasal floor.
Several theories explain the growth pattern of OKCs, including intraluminal hyperosmolality, active epithelial proliferation, collagenolytic activity of the cyst wall, and interleukin-1 and -6 synthesis by keratinocytes, which stimulate osteoclastogenesis and bone resorption.1
Radiologically, the lesion appears as a well-defined radiolucent area, either unilocular or multilocular, sometimes associated with an impacted tooth. Although radiological examinations provide diagnostic guidance, they are nonspecific, as dentigerous cysts, lateral periodontal cysts, radicular cysts, ameloblastomas, adenomatoid odontogenic tumors, ameloblastic fibromas, and plasmacytomas can exhibit similar radiographic features.7
Definitive diagnosis requires histopathological analysis, revealing a stratified squamous epithelium of regular thickness (5–8 cell layers) with an undulating surface and hyperkeratosis, which may be orthokeratotic or focally parakeratotic. The epithelial layer is bordered by a straight basal layer of cuboidal or columnar basophilic palisaded cells with reverse polarization. Mitoses are frequently observed in the suprabasal layers. A key characteristic of OKCs, found in approximately 20% of cases, is the presence of daughter (satellite) cysts within the fibrous cyst wall or adjacent to the main lesion, contributing to the high recurrence rate. Variable amounts of keratin can be observed in the cystic lumen.8
OKCs are classified into parakeratinized and orthokeratinized subtypes. The parakeratinized variant, which accounts for 80% of cases, is more aggressive and has a higher recurrence rate than the orthokeratinized form.9
OKCs may present in two forms: a non-syndromic solitary cyst or multiple cysts associated with syndromic conditions. The syndromic form, characterized by multiple OKCs, is commonly linked to Gorlin–Goltz syndrome and other clinical manifestations such as: numerous basal cell carcinomas, along with skeletal, ophthalmic, and neurological abnormalities.10 However, the present case involved a non-syndromic solitary OKC.
The therapeutic approach for maxillary OKCs depends on their location, extent, recurrence status, and biological behavior. Treatment options range from conservative methods, such as simple enucleation, to more aggressive procedures like radical resection.11 Despite their aggressive nature, advancements in genetic and molecular research have led to a shift toward less invasive management. Marsupialization or decompression, with or without subsequent enucleation, has gained support as a strategy to minimize recurrence while preserving surrounding structures.12
A systematic review conducted in 2017 by Mayara Santos de Castro et al. assessed the clinicopathologic features and outcomes of conservative surgical treatments for non-syndromic odontogenic keratocysts. Through meta-analysis, it was demonstrated that among conservative surgical approaches, decompression followed by enucleation yielded the lowest recurrence rate (11.9%), followed by marsupialization with enucleation (17.8%). In contrast, enucleation alone had a higher recurrence rate of 20.8%.13
In our case, enucleation was performed four months after decompression, allowing for a reduction in cyst volume and the formation of a bony shell at the nasal and sinus floor. This approach minimized the risk of significant nasal or sinus communication and tooth mobility following enucleation. The early timing of intervention was influenced by the patient's decreasing motivation, ensuring a more controlled, less invasive procedure while reducing potential complications and improving overall outcomes.
Histological examination revealed epithelial changes following decompression, with the cyst lining undergoing transformation into stratified squamous epithelium resembling oral mucosa. August et al. proposed that exposure of the OKC lining to the oral environment may induce epithelial dedifferentiation, converting the keratinized cystic lining into non-keratinizing epithelium, which is considered a less aggressive form.14 Additionally, evidence suggests that decompression facilitates cystic capsule expansion, enhancing complete surgical removal. This approach also reduces levels of IL-1α and cytokeratin-10, biomarkers associated with cyst growth, supporting the efficacy of conservative treatment.15 These epithelial and biological alterations likely contribute to the lower recurrence rates observed in OKCs treated with decompression followed by enucleation.
In our case report, no signs of recurrence were observed, both clinically and radiographically, 18 months after decompression followed by enucleation. We will continue to monitor the patient over time
The staged surgical management of odontogenic keratocysts, involving initial decompression followed by cyst enucleation, offers a conservative yet effective alternative to radical resection by minimizing recurrence risk, preserving vital anatomical structures, and improving patient recovery and long-term prognosis, especially in cases of large lesions.
None.
The authors declare that there are no conflicts of interest.

©2025 Chaouachi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.