Journal of
eISSN: 2373-4345


Case Report Volume 6 Issue 4
Department of Oral Health Practice, University of Kentucky College of Dentistry, USA
Correspondence: Mohanad Al Sabbagh, Department of Oral Health Practice, University of Kentucky College of Dentistry, 800 Rose Street, Lexington, KY 40536-0297, USA, Tel 859-257-3003, Fax 859-257-8878
Received: November 19, 2016 | Published: February 15, 2017
Citation: Al Sabbagh M, Damm DD, Thomas MV. Body nasopalatine duct cyst modified. J Dent Health Oral Disord Ther. 2017;6(4):94-96. DOI: 10.15406/jdhodt.2017.06.00204
This article aim to introduce the study process and outcome of Maxillary Midline Diastema formation after Nasopalatine Duct Cyst (NPDC); which is the most common non-neoplastic, non-odontogenic maxillary cyst. In this report we present a 24-year old male student recently experienced the formation of a maxillary midline diastema. The maxillary central incisors exhibited less than 1 mm of buccolingual mobility and less than 2 mm of attachment loss. Panoramic and periapical radiographs showed a radiolucent lesion located in the premaxilla, between the maxillary central incisors. A cone-beam computed tomography (CBCT) scan suggested that the radiolucent lesion was confluent with the incisive canal. A presumptive diagnosis was Nasopalatine Duct Cyst (NPDC) and the cyst was surgically excised via palatal approach. Surgical enucleation is usually the treatment of choice, although marsupialization also has been used for larger lesions. On the basis of the clinical, radiographic, and histopathologic features, the diagnosis of NPDC was confirmed. The spontaneous appearance of an MMD in an adult patient should suggest the possibility of pathology. The differential diagnosis should include periodontal attachment loss and expansile lesions, most notably the nasopalatine duct cyst. The review is to show the relationship between Maxillary Midline Diastema and Nasopalatine Duct Cyst.
The nasopalatine duct cyst (NPDC) is a developmental, non-neoplastic cyst arising from degeneration of nasopalatine duct and is considered the most common non-odontogenic maxillary cyst.1 It arises within the nasopalatine canal and often presents as a painless swelling in the area of the incisive papilla. Frequently, it is asymptomatic and is discovered by routine radiographic examination; on radiographs, it appears as a well-defined heart-shaped radiolucency in the premaxillary region between the central incisors and they must be larger than 0.6 cm to be distinguished from the incisive foramen. Many studies have reported that this lesion exhibits a predilection for males, but this has not been a universal finding. We report a case with the initial presentation of a maxillary midline diastema (MMD).
A 24 year-old male dental student sought care from one of the authors after attending a lecture in which the evaluation of Maxillary Midline Diastema (MMD) was discussed. The student informed the lecturer that he had recently experienced the formation of such a diastema and wished to rule out the presence of periodontitis or other pathology. Clinical examination detected a Maxillary Midline Diastema (MMD). The maxillary central incisors exhibited less than 1 mm of bucco-lingual mobility and less than 2 mm of attachment loss. Panoramic and periapical radiographs showed a radiolucent lesion located between the maxillary central incisors. A cone-beam computed tomography (CBCT) scan suggested that the radiolucent lesion was confluent with the incisive canal (Figures 1–3). The presumptive diagnosis was Nasopalatine Duct Cyst (NPDC), and surgical excision was recommended. The patient accepted the treatment plan, and the cyst was enucleated via a palatal approach with the patient under local anesthesia and conscious sedation (Figure 4). A labial flap was not elevated so that the loss of interdental soft tissue could be avoided. Measurements taken at the time of surgery indicated that the patient was at high risk of loss of the interdental soft tissue. The defect was filled with medical grade calcium sulfate before flap closure. The patient tolerated the procedure well, and healing was uneventful. The interdental soft tissue remained largely intact (Figure 5). The excised tissue was submitted to the Oral Pathology Service of the University of Kentucky College of Dentistry for examination. Histopathologic analysis showed a cyst-like structure that was partially lined by thin stratified squamous epithelium. The wall of the structure consisted of dense fibrous connective tissue with scattered vascular channels and neural bundles. On the basis of the clinical, radiographic, and histopathologic features, the diagnosis of NPDC was confirmed.
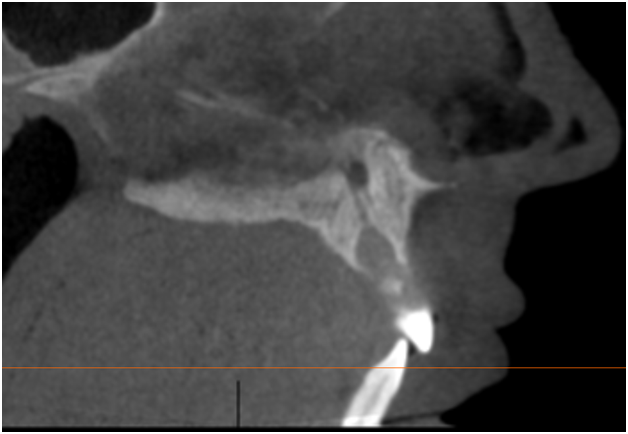
Figure 1 Sagittal cone-beam computed tomography image shows a well-defined expansile low-density lesion in the inferior portion of the incisive canal.
We undertook a literature review using PubMed. The first search used the search terms “nasopalatine” and “diastema” in the “Title/Abstract” field. The search was limited to reviews in English. The second search used the search terms “maxillary” and “diastema” and was, again, limited to English-language publications. A third search used the search terms “incisive canal” and “diastema.”
The first search returned no results, leading the authors to believe that MMD formation has not been reported as a complication of NPDC. The second search returned 35 results, 7 of which were not in English and were discarded, leaving a total of 28 reports. These reports had been published between 1968 and 2006. On the basis of a review of abstracts or of the full publication, we determined that none of these publications was relevant to the current case. The third search yielded no citations.
The Nasopalatine Duct Cyst (NPDC) was first described by Meyer (1914), who described it, as a “supernumerary paranasal sinus”.2 These cysts are the most common non-odontogenic cyst found in the mouth and are usually diagnosed when patients are in the fourth to sixth decades of life. A recent review of published case series reported a male-to-female prevalence ranging from 1.2:1 to 3.4:1.1 Many cases are asymptomatic and are discovered upon routine examination. When present, the most common symptoms are pain and swelling related to the expansile nature of the lesion. The NPDC is believed to arise from epithelium-lined tubes within the bony incisive canal.3–6 A precipitating cause usually cannot be identified, although infection and trauma have been suggested as possible etiologic agents.1 Surgical enucleation is usually the treatment of choice, although marsupialization also has been used for larger lesions when there is concern about postoperative fistula formation.1–5
The presentation in this case is unusual because of the initial finding of MMD. A review of the biomedical literature yielded no additional reports of cases of NPDC exhibiting this clinical feature (although this scarcity is surely the result of underreporting). It is important for the clinician to consider pathology in the case of an MMD that forms de novo in an adult patient. Long-standing stable diastemata may reflect an underlying discrepancy between tooth size and arch length or be due to congenitally missing teeth.7 Causes of unstable diastemata in the maxillary anterior sextant include poor oral habits, posterior bite collapse or other occlusal factors, and loss of periodontal attachment. Periodontal disease is a common cause of diastema formation in the anterior dentition.8 The clinician must rule out pathology when a Maxillary Midline Diastema (MMD) occurs in an adult patient.
The spontaneous appearance of a Maxillary Midline Diastema (MMD) in an adult patient should suggest the possibility of pathology. The differential diagnosis should include periodontal attachment loss and expansile lesions, most notably the Nasopalatine Duct Cyst (NPDC).
None.
The corresponding author dedicates this work to the memory of Dr. Mark V Thomas, longtime colleague and friend.
The authors declare that there is no conflict of interest.

©2017 Al, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.