Journal of
eISSN: 2373-4345


Case Report Volume 9 Issue 5
1Department of Oral & Maxillofacial Surgery, Akhtar Saeed Medical & Dental College, Pakistan
2Department of Oral Pathology, Akhtar Saeed Medical & Dental College, Pakistan
3Department of Dental Materials, Akhtar Saeed Medical & Dental College, Pakistan
Correspondence: Muhammad Kashif, M.Phil, Assistant Professor, Department of Oral Pathology Bakhtawar Amin Medical & Dental College, Mattital road, 60000, Multan, Pakistan
Received: October 01, 2018 | Published: October 11, 2018
Citation: Haq EU, Minhas S, Asad R, et al. An unusual case of ossifying fibroma in the anterior maxilla: a case report. J Dent Health Oral Disord Ther. 2018;9(5):382-385. DOI: 10.15406/jdhodt.2018.09.00413
Ossifying fibroma is a benign bone tumor, its origin in head and neck region, is supposed to be from periodontal membrane. Large Ossifying fibroma occurring in the maxilla might have different radiographic appearances which might direct to incorrect diagnosis and treatment. Here we report a 22year old male patient with a chief complaint of swelling in the upper anterior maxilla. The patient has been conscious of the swelling since 5years. It was slow in onset, enlarged over theyears to the present size and was not associated with the history of any tooth ache or trauma in that region of the jaw. Clinical/extra oral examination revealed a giant swelling on the right side of the face, especially in the anterior jaw, leading to gross facial asymmetry. Correlating the clinical, histopathological and radiological findings, a concluding identification of ossifying fibroma was given. Treatment done was complete resection i.e. maxillectomy and reconstruction of maxilla with a reconstruction plate under general anesthesia.
Keywords: ossifying fibroma, fibro-osseus lesion, maxillectomy
Ossifying fibroma is a benign bone tumor, considered to be a type of fibro-osseous lesion. Its origin is supposed to be from periodontal membrane.1Most common site of occurrence for ossifying fibromas is the posterior region of the mandible.2‒4 It may also occur in the maxilla, usually in the area of the canine fossa and in the region of the zygomatic arch with the most common occurrence in females. 5‒7 The peak age of incidence for ossifying fibroma is the third and fourth decades of life.5,8 Sometimes, it is also associated with tooth displacement and facial asymmetry.6,9,10
On radiographic examination, the edges of the lesion are usually well demarcated, with a thin radiolucent line that represents a fibrous capsule. The inner structure shows mixed radiolucent–radiopaque appearance, with an outline that depends on the form and quantity of the calcified material that is present.6,9,10
Histologically, ossifying fibroma is a well- circumscribed lesion comprising of fibroblastic stoma having lamellar bone and plexiform patterns in addition to acellular mineralized material.11
Ossifying fibroma also contains hypercellular fibrous tissue with the random presence of islands of bony tissue or cementiform calcifications. Mineralized masses of tissue conforming to osteoid material or cementum can also be seen inside fibrous stroma along with dystrophic calcification.12 The well demarcated nature of lesion usually permits enucleation of the tumor.2 After surgical enucleation of the lesion, reconstructive surgery might be required in order to overcome esthetic and functional complications.2
The aim of documenting this case report has been to present a first ever case of ossifying fibroma of such a gigantic size in maxilla in Lahore, Pakistan as presented in our case is rarely come in contact worldwide and to give a critical review of the current literature about the lesions of this type. Large Ossifying fibroma occurring in the maxilla might have different radiographic appearances which might direct to incorrect diagnosis and treatment. For confirmatory diagnosis histopathological assessment is required. A relationship between clinical, imaging and histopathological features is the means for the beginning of precise diagnosis. It is important to make an early diagnosis, utilize the suitable treatment and follow- up the patient over a long term. The tumour was treated by excision through marginal resection, in association with reconstruction and prosthetic rehabilitation.
A 22year old male patient reported in the Mid-City Hospital with a chief complaint of swelling in the upper anterior maxilla. The patient was conscious of the swelling since 5years. It was slow in onset, enlarged over theyears to the present size and was not associated with the history of any tooth ache or trauma in that region of the jaw. Initially the swelling was asymptomatic but a history of associated pain since 3‒4years was noted and had become painful on closure of the jaw because of the contact of the lower teeth with the lesion. The patient had no significant past medical or surgical history and all vital signs were normal.
Clinical examination/ extra oral examination revealed a giant swelling on the right side of his face, especially in his anterior jaw, leading to gross facial asymmetry (Figure 1) whereas patient had a normal mouth opening. History of loss of sensation was noted and no history of pus discharge.

Figure 1 Pre-Op Extra Oral Photograph showing exophytic growth. 30 Y male patient, painless, slowly growing exophytic bony hard swelling at anterior maxilla, no paresthesia; Occasional bleeding, ulcerated and fragile mucosa; impacted teeth associated with the lesion; Firm to hard bony mass.
Intra- oral examination revealed that the swelling was solitary, well- defined, firm in consistency, non- tender and of approximately 15×18cm in size extending from one side of tuberoses to the opposite side of tuberosity and superiorly to infra –orbital rims with a slight palatal expansion. Because of huge size lesion, patients were suffering from paraesthesia of infra-orbital nerve, difficulty in chewing, speaking and swallowing. Marked alveolar asymmetry with a gross displacement of maxillary teeth was noted. However, the associated teeth were firm, non- mobile and without any associated root resorption. The overlying mucosa was intact and normal in appearance. No evidence of lingual cortical plate expansion or perforation was noted. There were no palpable lymph nodes and infra- orbital nerves were bilaterally intact. Based on the clinical findings and history, a differential diagnosis of calcifying epithelial odontogenic tumor, osteoblastoma, ossifying fibroma and cementoblastoma were given.
Radiographic assessment with OPG and CT scan of maxilla showed a mixed radio-opaque and radiolucent lesion with disperse foci of calcifications throughout the lesion (Figure 2). On CT scan a hyperdense mass involving both maxilla and extending posteriorly up to the pterygoid plates was observed with complete destruction of normal anatomy. The patient underwent through an incisional biopsy of the lesion for histological examination.
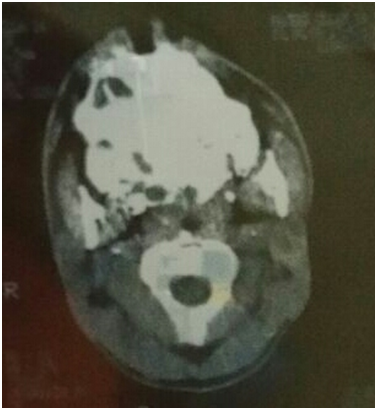
Figure 2 Axial slice at mid face region showing hyperdense mass with defined margins but no structural differentiation. Involved bilateral maxillary sinus obliteration, extending posteriorly up to pterygoid plates and interiorly to the maxillary alveolus.
Histopathological evaluation reported that the lesion had connective tissue stroma that was highly cellular with abundant collagen fibers and fibroblasts. Trabeculae of bone with plump fibroblasts and globules of calcification were distinguished Figure 3. Few endothelial lined blood vessels were also observed, giving an idea of ossifying fibroma.
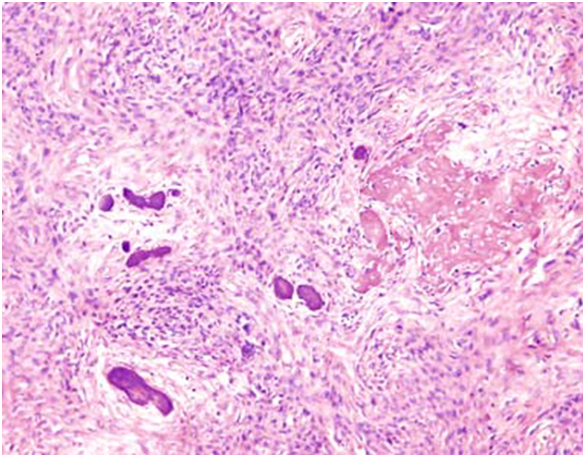
Figure 3 Connective tissue stroma was highly cellular with abundant collagen fibers and fibroblasts. Trabeculae of bone globules of calcification were seen.
Correlating the clinical, histopathological and radiological findings a concluding identification of ossifying fibroma was given. Treatment done was complete resection i.e. maxillectomy and reconstruction of maxilla with a reconstruction plate under general anesthesia. (Figures 4) (Figure 5) After one year of surgery, the defect was reconstructed with prosthetic obturator. Obturator fulfilled the desired goals, acceptable aesthetics and better chewing function. No recurrence observed on follow ups (Figure 6). Future plan is to reconstruct with free flap and the replacement of lost teeth with fixed prosthesis.

Figure 4 Post-Op Intra-Oral Defect (After Complete Healing, Clear margins visible & bed is ready for prosthesis provision.
Ossifying fibromas are initiated from the pluripotent mesenchymal stem cells, which are capable of producing cementum and bony tissues.13,14
The ossifying fibroma involves the maxilla and mandible and is a comparatively uncommon benign tumour. Even though OF emerges as a solitary, slow growth lesion [15, 16] whereas a small number of cases of several tumours have been reported.15
The reason for the formation of OF is that there may be previous tooth extraction or periodontitis that may give a stimulus16 or that the formation of ossifying fibromas might be simply linked to a disturbance of bone maturation of congenital origin.4
These lesions are more common in women as compared to males3,17 and takes place more frequently among the third and fourth decades of life18,19 which is in contrast to the present case report where the OF was reported in 19years old male.
In the present case report, huge expansile mass was observed in the maxilla, whereas, Chang et al.,15 reported that 61% of the OF cases involved the posterior region of the mandible. This deviation might be because of variations in the number of cases available in earlier series or ultimate geographic characteristic when compared with the reports available around the world.15,16,19 Whereas other studies reported that the mandible premolar and molar regions are the most frequent sites.2,20,21 However some studies reported the maxilla as the most common site of22,23 which are similar to the current case study.
Swelling in the involved region is for the most common clinical sign noted in patients with OF. They are typically painless and ultimately recognized in routine radiographic assessment24 Ossifying fibroma might be areas on for root resorption, mobility and tooth displacement in nearby teeth but is common findings in the involved teeth25,26 whereas according to some authors these are infrequent findings.8 Small lesions are asymptomatic and as they enlarge and develop they cause tumefaction i.e. regardless of significant facial asymmetry, the lesions are pain-free, thus paraesthesia and pain are infrequently related with OF.2,3 These all previous case reports clinical features are in line with the present case report where the most frequent complaint was huge swelling on the left side of the maxilla causing facial asymmetry with displaced teeth and resorbed roots.
Histologically, OF contain cellular connective tissue with mineralized material; ossicles that join to form bone trabeculae that are frequently bounded by osteoblasts and rarely by osteoclasts. Cementum-like rounded calcifications are also commonly reported and in a single lesion a combination of these two types of calcifications are frequently reported18,27 similar to be observed in this current case report.
Four radiographic criteria for ossifying fibroma are recognized, that are, ground glass appearance, sclerotic change, mixed type and cystic radiolucency. Whereas Barberi et al. stated three radiographic patterns for ossifying fibroma, that is, radiolucent (53%), mixed type (40%) and sclerotic (7%).28
Radiographically, the appearance of ossifying fibroma might be differing depending on the quantity of mineralized tissue in the tumour. OF frequently become visible as well-demarcated lesion, unilocular within consistent quantity of radiopaque foci within the lesion. As a result, a mixed radiographic picture is frequently noticed.15, 4, 26 Computerized tomography (CT) is necessary for an absolute assessment of the ossifying fibroma. For the accurate evaluation and identification of intra-osseous lesions, numerous image assessments should be utilized. Enlargement of the ossifying fibroma might expand the quantity of mineralized material within the of29
Such a huge lesion of OF is very rare worldwide. In the case described here, after exploring the tomographic and radiographic images it was observed that all the cortical bones had ruptured. On CT scan, it was observed a hyperdense mass with the involvement of both maxilla and extension up to the ptyergoid plates completely distorting the anatomy of the maxilla. The radiographic findings were uncertain. Therefore, both benign and malignant lesions were considered in its differential diagnosis.
The clinical management of ossifying fibroma still doesn't clear. To reduce the possibility of recurrence, for larger lesions an enbloc or partial resection of the jaw is ideal.8,29 When the surgical resection is wide, added restoration using implants and bone grafts can be essential because of functional and esthetic problems, particularly when teeth are removed.2,8 In the case explained here, as the lesion ruptured all the cortical bones of maxilla thus radical excision with all involved teeth was performed. Since the region that could be subject to strong muscle area was widespread, it was decided to place a titanium reconstruction plate in order to retain the maxillary outline. After one year of surgery, the defect was reconstructed with the prosthetic obturator to fulfill the functions of chewing, speaking, swallowing and acceptable aesthetic.
For such patients the significance of general evaluation needs to be highlighted. Despite of only concentrating on the assessment of their chief complaints, a thorough clinical examination should be carried out when there is dissimilarity from the normal and have any pathological changes. In this way, the patient situation can be properly diagnosed and suitable treatment plan can be planned.
Our findings explained for acceptable, adaptable and safe treatment option of, the conservative surgical excision of comes out to be a better option (Figures). The recovery was ordinary and the patient has continued as tumour-free till now. Even though OF is a benign, reactive lesion and the recurrence is quite high. Therefore, the patient is still on usual follow-up. Some authors ‘reported that OF shown no recurrence over a 17year follow-up time when they are treated by conservative surgical excision.16
This case report adds the data to the existing literature about the presentation, clinical features (pain, paraesthesia), radiographic imaging (Panorama and CT scan) with appearance of and treatment of in the maxilla, which in turn helps the clinicians for proper diagnosis and treatment. Long term follow – up are significant in the treatment of because of its violent type and increased recurrence rate.
None.
Author declares that there is no conflict of interest.

©2018 Haq, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.