Journal of
eISSN: 2373-4345


Case Report Volume 2 Issue 1
Department of Prosthodontics, University of Athens, Greece
Correspondence: Sava Kosmin, Makrygianni 2 Elefsina, 19200, Greece, Tel 302000000000, Fax 302000000000
Received: October 22, 2014 | Published: February 12, 2015
Citation: Kosmin S, George P, Phophi K, et al. Advantages of combined cemented and screw-retained implant supported prosthesis. a clinical report. J Dent Health Oral Disord Ther. 2015;2(1):19-24. DOI: 10.15406/jdhodt.2015.02.00037
Cemented and screw-retained implant prostheses offer distinct advantages and limitations. Prosthesis retrieval is challenging with cemented restorations. A method to facilitate the retrieval of the prosthesis is described for both a multiple unit implant and multi tooth retained telescopic restoration. Management of a patient over 5years is described that involves a situation requiring use of the retrieval design described.
Keywords: implant prosthesis, passive fit, dual retention, retrievability
FDP, fixed dental prosthesis; A.C.P.P.D.I, american college of prosthodontics prosthodontic diagnostic index; CT, computerized tomography
Implant supported restorations can be (a) retained with screws or (b) cemented to suitable abutments. Screw-retained implant restorations have an advantage of predictable retrieval, but they also require precise implant placement for optimal location of the screw access hole.1–3 Creating passive fit for screw-retained frameworks is challenging due to dimensional discrepancies inherent in the fabrication process. Cementation of implant restorations eliminates unaesthetic screw access holes and helps compensate for discrepancies in fit.4,5 The primary difference between the two modalities is that a screw-retained prosthesis can be recovered and replaced as needed, while a cemented restoration is not designed for retrieval. Retrieval was a key concern in early stages of osseous integrated implant use before there was extensive documentation on implant biomechanics and good confidence in long term survival.1–3 This report describes a method to fabricate multiple unit cement retained and screw retained telescopic restoration supported by implants and teeth. It is intended for cases in which prosthesis retrieval, optimal esthetics and passive fit are all very important for success.
Diagnosis
A 50-year-old male patient with no history of medical problems presented for a consultation in order to receive osseous integrated implants. The patient reported mastication problems and desired an option of fixed implant supported prostheses (Figure 1A-1C). All relevant diagnostic information was collected including dental history, preliminary diagnostic casts and intraoral photographs. Radiographic evaluation included full mouth periapical radiographs and a panoramic radiograph. Clinical and radiographic examination revealed generalized advanced periodontitis, decayed areas of the upper right second premolar and canine, the upper left premolars and lower left second molar and first premolar. Periapical lesions were present at upper right lateral, upper left first premolar and lower left premolars (Figure 2). Occlusal disharmony was evident that was attributed in part to the size and lack of anatomy of the mandibular partial fixed dental prosthesis (FDP). This prosthesis included open margins and two molar cantilevers.
Risk assessment
The patient’s periodontal condition required that most teeth had to be extracted. Removable dental prostheses (although offered as a treatment option) were not acceptable to the patient. His general health condition involved no risks for implant placement. He was not a smoker. A major improvement in oral hygiene status was mandatory prior to planning any surgical procedure. Nevertheless, there was always a risk of losing some or all of the remaining teeth if the oral hygiene status did not remain optimal. For that reason, implants were placed in “strategic” locations, allowing survival of the prosthesis in the event that one or all of the abutment teeth were lost over time. For the same reason the prosthesis had to be retrievable, allowing modifications or repairs.
Treatment planning
On the basis of the general oral status, the periodontal and occlusal status, posterior over closure and need for preprosthetic adjunctive treatment, the patient was categorized as class IV according to the A.C.P.P.D.I. (American College of Prosthodontics Prosthodontic Diagnostic Index). The treatment sequence included several steps. Hopeless teeth were extracted. Interim prostheses were placed to re-establish occlusal harmony and occlusal vertical dimension in centric relation. The periodontal condition of the remaining teeth was improved and a highly improved oral hygiene status for the patient was verified over time. When these were established, rehabilitation was started with placement of implants, a healing period, and the definitive prosthetic rehabilitation. The patient was placed on a 4-month recall schedule, initially, and later a 6-month recall.
Surgical treatment
All teeth with hopeless prognosis were extracted. Remaining teeth were maxillary canines and central incisors and mandibular canines and the first premolar on the right side. They were used as abutments for interim restorations. For the maxilla a metal acrylic, teeth and tissue supported restoration was fabricated.6,7 For the mandible a multiple tooth supported restoration with cantilevers was created (Figure 3A & 3B). The patient was referred for a computerized tomography (CT) (Figure 4A & 4B).
Six implants (Xive Implants; Friadent GmbH; Dentsply, Germany) were placed in the maxilla corresponding to the positions of the laterals, second premolars and first molars. Three months later 4 implants were placed in the mandible corresponding to the positions of the first premolars and first molars. All were pre-established with careful presurgical planning (Figure 5). Three of the mandibular implants had an internal connection platform (Xive Implants; Friadent GmbH), while the most posterior one, on the right side (corresponding to the lower right first molar) had an external connection platform (Osseotite; BIOMET 3i; Palm Beach Gardens, Fla). The interim restorations were cemented again to the abutment teeth since they were not in contact with the surgical fields. All implants osseointegrated favourably with no signs of mobility, inflammation or bone loss. Remaining teeth, except for the mandibular premolar that had to be extracted, presented with a stable periodontal condition with no further bone or attachment loss and class I mobility. They were selected as abutments for the definitive prostheses.
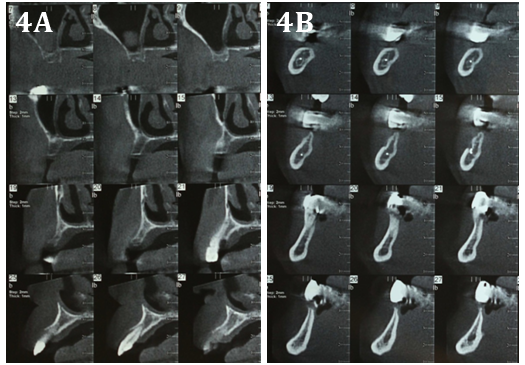
Figure 4A Part of the computerized tomography of the maxilla and mandible.
Figure 4B Implants were placed in positions represented by cuts 14 and 20 for the maxilla as well as 14 for the mandible.
Restoration fabrication
Retrievability was a main goal in the planned design for these prostheses because of the concern of creating abutments on periodontally involved teeth in combination with osseointegrated implants. Telescopic copings have been used previously for these situations with good results.8–13 Prefabricated abutments were planned for all implants. For abutment teeth a combination of retention modalities was used. Primary copings were permanently cemented. Definitive prostheses were luted with temporary cement. For the mandibular prosthesis dual retention (cement as well as screw) was used. The teeth and most of the implants were used as telescopic abutments. One posterior implant was used as a screw retained abutment.
Prosthodontic rehabilitation
Implant-level impressions were made using polyvinyl siloxane in custom trays. The impressions of the abutment teeth were made at the same time and were poured in die stone to produce master casts. Occlusion rims were constructed on master casts. Face bow record and a centric relation record were made with a vinyl polysiloxane material. Six prefabricated titanium abutments were attached to the maxillary master cast and modified to create a common path of placement with the primary copings. Finish lines of the abutments were placed just below the gingival margin to achieve ease of cement removal. Three titanium abutments were attached to the mandibular master cast and modified in a similar fashion (Figure 6A & 6B).
Four primary copings on the maxillary cast and two more in the mandibular cast were fabricated for the abutment teeth. Passive fit is a key requirement for the longevity of such restorations. To accomplish that, verification indices were fabricated in low shrinkage acrylic resin (Pattern Resin LS; GC America Inc; Alsip, Ill) on the master casts and evaluated intra orally to guarantee accurate transfer of the implant abutments and the primary copings (Figure 7).
Next, the secondary framework was fabricated. The mandibular framework waxing up included a castable abutment and a screw access hole for the implant placed in position of the lower right first molar. Frameworks were cast in base metal alloy (Remanium; Dentaurum; Ispringen, Germany) and were returned for try-in. A centric relation record between the metal frameworks of the opposing arches was produced using an anterior programming device in order to confirm the correct relationship of the master casts (Figure 8).
Metal ceramic prostheses were fabricated using standard laboratory protocols. At the delivery appointment, primary copings were permanently cemented onto abutment teeth using resin modified glass-ionomer cement (FujiCEM; GC Corporation; Tokyo, Japan). Titanium abutments were attached to the implants. After radiographic evaluation of their fit, each one was tightened to the manufacturer’s suggested torque (Figure 9).
The definitive maxillary prosthesis was cemented with temporary cement (Integrity Temp Grip; Caulk; Dentsply; Milford, Del). The mandibular restoration was cemented with temporary cement and simultaneously the retaining screw was tightened following manufacturer’s recommended torque (Figure 10A & 10B). The patient was given hygiene instructions and a recall schedule was established.
The restorations were placed in 2005 and so this is a 5-year report. The mandibular restoration had to be removed once after 3years for the left natural canine to be endodontically treated (Figure 11).
It was replaced on the abutments without further modification, proving the main concept of this fabrication design, which was the potential for retrieval. The patient’s compliance with the recall schedule was good and he missed only one appointment in 5years. His oral hygiene was acceptable but certainly not optimal (Figure 12).
Nevertheless, his overall periodontal status was good with no signs of deterioration at the abutment teeth and no signs of peri-implantitis. There was no evidence, clinical or radiographic, of decay around the abutment teeth. Occlusion was stable with no signs of wear or fractures of the porcelain. A small fracture was present at the margin of the secondary crown on the upper left canine at the 4-year recall. It was considered insignificant, because it did not compromise the clinical or aesthetic results. There were no other problems associated with the prosthesis such as debonding, prosthesis or abutment screw loosening, speech or aesthetic problems or history of pain.
The major advantage of dual retained restoration was the option for retrieval. Most of the retention was offered by the retention screw of the posterior abutment. The telescopic ones were luted with temporary cement in order to avoid food leakage and microbial colonization. The restoration could be easily retrieved if the retaining screw was removed. Another advantage was the ability to combine implant and teeth abutments using telescopic crowns on the teeth. This option, although it did not affect retrievability, allowed for the natural teeth to be retained and be splinted in one bilateral restoration. Several studies have demonstrated the feasibility of using a combination of implants and natural teeth in a FDP. There are some clinical situations that may indicate the use of combined teeth-implant supported fixed dental prostheses, such as bone deficiency restricting strategic positioning of implants and financial constraints limiting the number of implants. The majority of the failures of combined teeth-implant prostheses are not due to implant success or survival, but primarily related to prosthetic complications and tooth intrusion when teeth and implant are connected with no rigid connection.14,15
The fabrication of the prostheses, although involving a complex list of procedures, was not much more difficult than for most fixed telescopic restorations. It demanded good knowledge of basic prosthodontic principles and commitment to a specific planed treatment sequence. The major disadvantage of dual retained prostheses was the significant increase in cost. Chair side and laboratory time were increased due to the complicated procedures involved. For the screw-retained abutment, the use of internal connection was almost impossible as a common path of insertion among the telescopic abutments and the internal anatomy of the implant had to be achieved. For that reason external connection was used on the most posterior implant. Alternatively, special abutments offered by most implant companies might be used to allow screw-retained multiple unit restorations to be fabricated over implants with an internal connection platform. The access hole for the retaining screw could be on either surface of the corresponding crown since aesthetics were not compromised when using the most posterior implant. Use of implants with an external connection platform for the screw-retained part of the restorations is no longer recommended since the time this particular restoration was completed. Retrieval of a dual retention restoration is usually uncomplicated. The retaining screw needs to be removed. Then the restoration can be debonded using any crown remover with light force. Retrieval could become difficult or even impossible if the abutment’s axial walls are absolutely parallel, the abutment height is greater than 6 mm, or permanent luting agent is used.
Possible reasons requiring retrieval of the restoration are damage to the prosthesis, need for endodontic or periodontal abutment treatment, or loss of an abutment. The prosthesis can be replaced after necessary modification, treatment or removal of problematic abutments. There are only a few clinical situations in which dual retention restorations cannot be used. Extreme inclination of the definitive abutment could make placement and retrieval of the restoration very difficult. Use of the technique on anterior restorations could create esthetic problems. In most other clinical situations, including short span posterior FDP’s or unilateral prostheses, dual-retention restorations have been used successfully.
A technique is described for fabricating a multiple unit implant and multi tooth retained telescopic restoration. Subsequent retrieval of the prosthesis is described. Fabrication of the prostheses, while including a complex list of procedures, is not much more difficult than for placement of most fixed telescopic restorations. The major advantage of dual retained restoration is retrieval if the retaining screw is removed. This facilitates necessary modification of the prosthesis or the need for endodontic or periodontal treatment of an abutment.
None.
None.
Authors declare that there is no conflict of interest.

©2015 Kosmin, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.