Journal of
eISSN: 2574-9943


Case Report Volume 9 Issue 1
1Dermatologist and assistant professor of dermatology at the University Hospital of the State University of Londrina – Londrina – Paraná (PR), Brazil
2Resident doctor in dermatology at the University Hospital of the State University of Londrina – Londrina – Paraná (PR), Brazil
3Pathologist at a private clinic – Londrina – Paraná (PR), Brazil
Correspondence: Rogério Nabor Kondo, Clinical Medicine Department, Dermatology - State University of Londrina, 60 Robert Koch Avenue, Londrina (Paraná), Brazil, Tel 55 43 99972-5668
Received: December 30, 2024 | Published: January 16, 2025
Citation: Kondo RN, Junior CB, Gubert M, et al. Balanitis pseudoepitheliomatous keratotic and micaceous of Civatte: case report of an atypical dermatosis. J Dermat Cosmetol. 2025;9(1):1-3. DOI: 10.15406/jdc.2025.09.00281
Keratotic and micaceous pseudoepitheliomatous balanitis is a rare dermatosis that presents as a whitish plaque in the region of the glans penis in men over 60 years of age who have been sexually active, in which the involvement of the human papilloma virus (HPV) is suspected. We report the case of a young patient, with no history of sexual activity and vaccinated for HPV as a teenager.
Keywords: pseudoepitheliomatous hyperplasia, keratotic and micaceous pseudoepitheliomatous balanitis, balanitis, glans penis
Keratotic and micaceous pseudoepitheliomatous balanitis (KMPB) of Civatte is a dermatosis that presents with a pseudoepitheliomatous response to inflammation or chronic infection, considered a rare condition that affects the glans penis of men over 60 years of age.1
There are less than 100 cases reported in the world literature and, to our knowledge, none published in Brazil, the country in which this case is reported. Some authors consider KMPB to be a pre-malignant lesion due to cases that progressed to squamous cell carcinoma.2–6 Its etiology is unknown, although there is a suspicion of the involvement of the human papilloma virus (HPV).2
Carrying out an early diagnosis is important to start treatment and avoid complications such as possible malignancy.7 We present an atypical case report, as it affects a young patient, without an active sexual life and immunized against HPV, with the aim of publicizing this rare entity.
An 18-years-old male, with a history of a lesion that initially appeared as a leukodermic papule, on the dorsal surface of the penis, just below the crown of the glans, which appeared one year ago. An incisional biopsy and partial resection were performed after 1 month, showing a lesion without atypia and without koilocytosis on pathology. Three months after the onset of these interventions, total excision was performed, however, the lesion developed early recurrence. He denied active sexual life, previous sexual relations or exposure to sexually transmitted diseases. Vaccinated for HPV at 11 and 12 years old.
On clinical examination 9 months after recurrence, he presented a leukoplastic lesion measuring approximately 1.5 cm in diameter, hyperkeratotic, with a micaceous appearance and irregular edges, discreetly infiltrative in the dorsal region of the glans penis, without inguinal lymphadenopathy (Figure 1A & 1B).
The patient had negative serology for HIV, hepatitis B, hepatitis C and syphilis.
A new biopsy showed hyperkeratosis, hypergranulosis, papillomatosis and marked irregular acanthosis, showing a pseudoepitheliomatous pattern, without dysplasia or viral cytopathic changes. Dermis with dilated and congested capillaries, accompanied by a slight lymphocytic infiltrate (Figure 2A– Figure 2C).
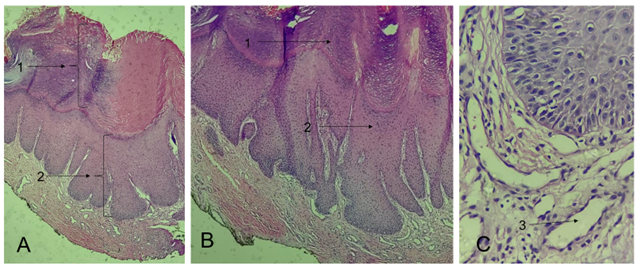
Figure 2 A. Panoramic view: hyperkeratosis (arrow 1), parakeratosis, acanthosis (arrow 2), straight and elongated ridges. B. Details of hyperkeratosis (arrow 1) and acanthosis with pseudoepitheliomatous pattern (arrow 2). C. Dilated vessels (arrow 3).
KMPB was first described by Jacob and Civatte in the mid-1960s, presenting as a thick hyperkeratotic plaque with scaling similar to mica adhered to the glans penis (Figure 3A & 3B).1
The pathogenesis of the disease is uncertain, but it is hypothesized that it is a form of bacterial infection, HPV infection or a pseudoepitheliomatous-type response to an external agent.1–5 Initially, it was understood that the lesion was benign or had reserved malignant potential. However, in 1987 Beljaards, Van Dijk and Hausman reported 2 cases that progressed to verrucous carcinoma and later to squamous cell carcinoma,4 contradicting the study by Corbeddu et al.6
The patient in this case was a virgin and had received two doses of the HPV vaccine at the age of 11 and 12. Polymerase chain reaction (PCR) followed by Reverse Molecular Hybridization with a universal probe for 35 genotyping showed low oncogenic risk HPV in the biopsy, but HPV can be found in 4.2% to 18% of virgin male patients, whose main hypothesis is inoculation through self-masturbation.8
There are still no reports on the dermoscopic description of KMPB, but we observed in our patient a central keratotic plaque with white scale, with areas of erythema and dilated vessels on the periphery of the plaque (Figure 4).
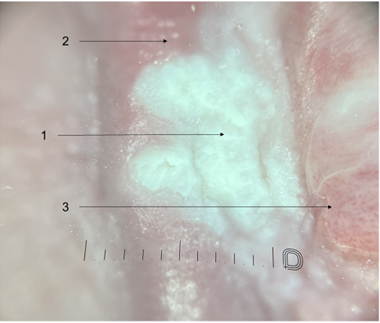
Figure 4 Central keratotic plaque with white scale (arrow 1), with areas of erythema (arrow 2) and dilated vessels (arrow 3) on the periphery of the plaque (Dermatoscope Dermlite DL5, 10 x).
On histopathological examination, KMPB presents nonspecific findings, with pseudoepitheliomatous acanthosis, hyperkeratosis, papillomatosis, capillary dilation and mixed inflammatory infiltrate,² as in the present case (Figure 2).
The main differential diagnoses are: erythroplakia of Queyrat, condyloma acuminatum, verrucous carcinoma, squamous cell carcinoma and other conditions of the penile glans region.1
Table 1 shows the clinical, dermoscopic and histopathological findings of KMPB, comparing with Erythroplasia of Queyrat and condyloma.9,10
|
Erythroplasia of Queyrat |
Condyloma |
KMPB |
|
|
Clinical findings |
Erythematous, velvety, well-defined, shiny plaque on the glans |
Papule or plaque, normochromic or erythematous, with a cauliflower appearance |
White plate with the appearance of Mica stone |
|
Dermoscopic findings |
Brown dots arranged in a linear fashion, hypopigmented central area without structure and glomerular vessels |
White, regular, clustered rounded structures (flat warts) or grouped bulbous projections of similar diameter and length (exophytic lesions) or separate digitiform projections, with different lengths (papillomatous lesions) |
Keratotic central plaque with white scale Areas of erythema on the periphery of the plaque Dilated vessels on the periphery of the plaque |
|
Histopathological findings |
Dysplastic and atypical cells, characteristic of carcinoma in situ |
Presence of koilocytes (cells surrounded by a clear halo, pyknotic nuclei and often with increased volume and on the periphery of the cell) |
Hyperkeratosis and acanthosis with pseudoepitheliomatous pattern |
Table 1 Clinical, histopathological, dermoscopic findings
Most cases of KMPB are asymptomatic, as in our patient, but fissures, maceration and local irritation may occur. Initially, the lesion evolves into a hyperkeratotic leukoplaque with a micaceous appearance on the glans penis. Diagnosis is based on clinical examination and local biopsy.2,3
Treatment is based on the degree of hyperkeratosis of the lesion and the lesional stage, with therapeutic options including topical 5-fluorouracil, electrosurgery and cryosurgery. In cases with evidence of malignancy, surgical excision should be recommended.3,5
There is a report of a patient with a satisfactory response to the use of oral acitretin. The drug in question is a second-generation retinoid that acts on keratinocytes and has been studied in keratinization disorders and other pre-malignant conditions such as actinic keratosis, xeroderma pigmentosum and epidermodysplasia verruciformis.1,7
This report is of great importance for dermatological and urological knowledge, due to the interface between the two specialties and because it is an uncommon entity. In this case, it is even more atypical, as it affects a young patient, with no active sexual life and no exposure to sexually transmitted diseases. Although hybridization highlights low-risk serotypes, the authors question whether HPV plays a fundamental role in its etiology.
None.
The authors declared that there are no conflicts of interest.
None.

©2025 Kondo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.