Journal of
eISSN: 2373-4396


Case Report Volume 18 Issue 1
1Department of Radiodiagnosis and Imaging, Postgraduate Institute of Medical education and Research, India
2Department of Cardiology, Advanced Cardiac Centre, Postgraduate Institute of Medical education and Research, India
Correspondence: Dr. Manphool Singhal, Professor, Department of Radiodiagnosis and Imaging, PGIMER, Chandigarh, India, 160012 , Tel +91 9417308300
Received: May 06, 2025 | Published: May 20, 2025
Citation: Sharma A, Chauhan E, Dahiya N, et al. Unilateral pulmonary artery atresia: Imaging findings with diagnostic considerations. J Cardiol Curr Res. 2025;18(2):25-26. DOI: 10.15406/jccr.2025.18.00620
Unilateral pulmonary artery atresia is a rare condition requiring high index of suspicion for diagnosis. It occurs more frequently on the right side which is usually isolated in contrast to the left sided pulmonary atresia which is commonly associated with other congenital cardiac abnormalities and right aortic arch. Multimodal imaging is often required to make an accurate early diagnosis. Timely management is crucial for preventing complications and improving patient outcomes.
DORV, double outlet right ventricle; VSD, ventricular septal defect; PS, pulmonary stenosis; ASD, atrial septal defect; SVC, superior vena cava; RA, right atrium; PA, pulmonary artery; UAPA, Unilateral absence of pulmonary artery
A 22-year-old female patient presented with dyspnoea on exertion and cyanosis. On examination, clubbing of the fingers and cyanosis were observed. A chest radiograph showed left lung volume loss with areas of reticular thickening. Transthoracic echocardiography revealed double outlet right ventricle (DORV), ventricular septal defect (VSD), pulmonary stenosis (PS), and an additional atrial septal defect (ASD). CT angiography (Figures 1-4) confirmed the findings of DORV, VSD, and PS. Additionally, it showed the presence of a large ostium secundum ASD with a double superior vena cava (SVC); the right SVC was seen draining into the right atrium (RA), while the left SVC drained into the RA via the coronary sinus. A side-by-side relationship of the great arteries was observed, with the aorta positioned to the left of the pulmonary artery (PA). A left-sided aortic arch with a normal branching pattern was identified. The main and right PA were visualized; however, the left PA was not seen. Multiple collaterals were observed in the mediastinum, arising from the bilateral subclavian arteries, the left internal mammary artery, the descending thoracic aorta, and the left lateral thoracic artery (Figure 2B). Hilar reformation of the left PA was seen via collaterals. The affected left lung showed volume loss with areas of interstitial thickening. An anomalous origin of the left anterior descending artery was noted from the anterior coronary sinus, showing a common ostium with the right coronary artery.
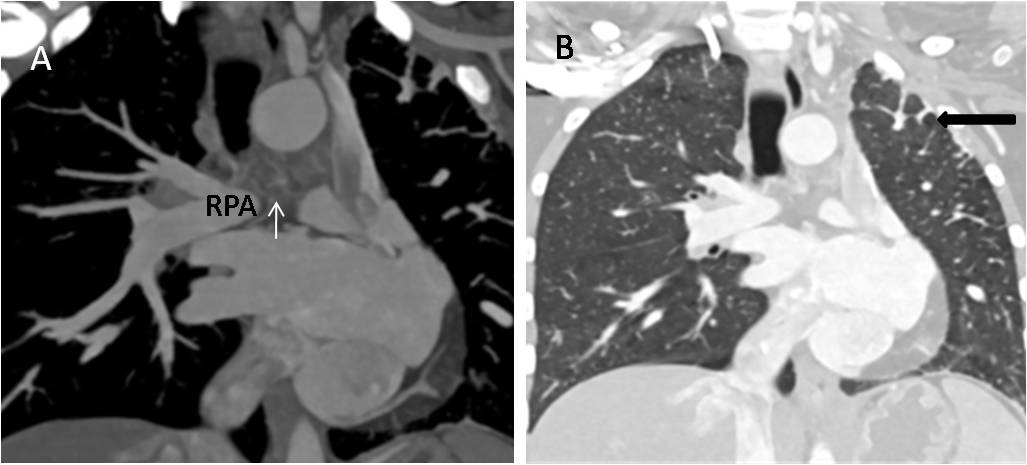
Figure 1 (A) Maximum intensity projection (MIP) coronal CT image showing right pulmonary artery (RPA) with non-visualized left pulmonary artery and presence of collaterals (arrow). (B) Coronal CT image in lung window setting demonstrating left lung hypoplasia with interstitial thickening (marked by black arrow).
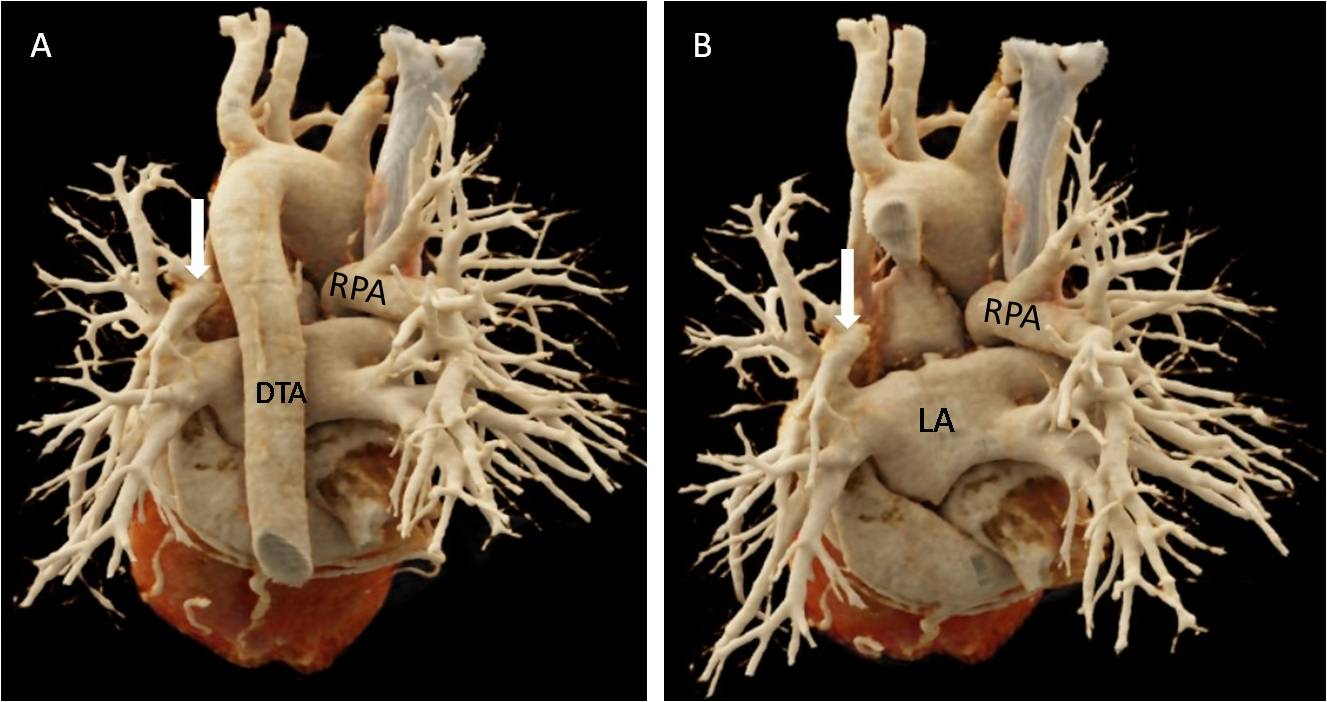
Figure 2 (A) and (B) Volume rendered CT images showing normal right pulmonary artery (RPA) with atresia of left pulmonary artery (LPA) and its hilar reformation (marked by white arrow). DTA-descending thoracic aorta, LA-left atrium.
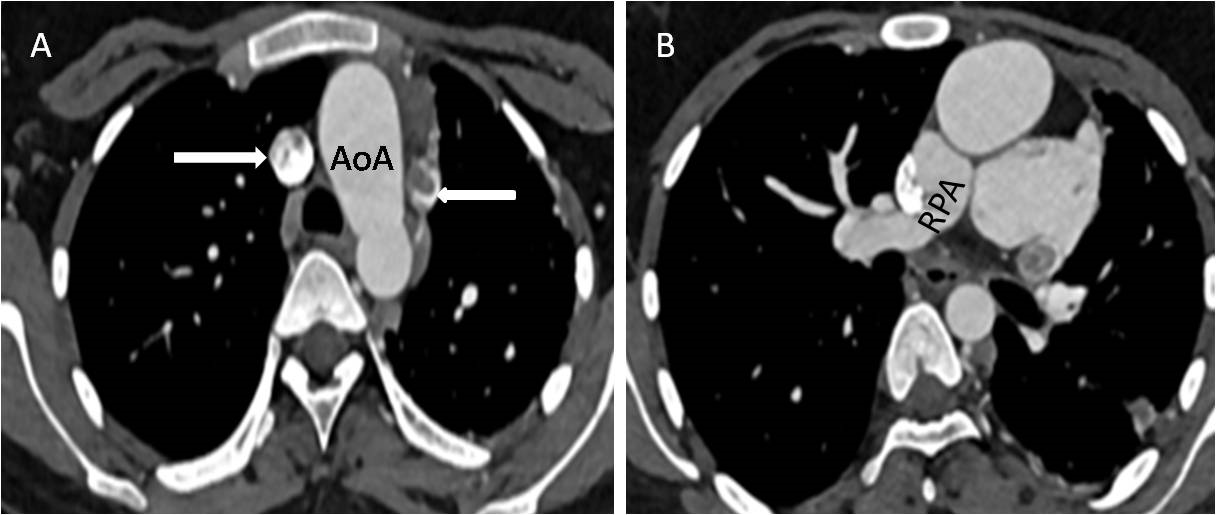
Figure 3 (A) CT angiography axial image showing left sided aortic arch (AoA), double superior vena cava (SVC) (marked by white arrow). (B) Axial CTA image depicting right pulmonary artery (RPA) with non-visualized left pulmonary artery.
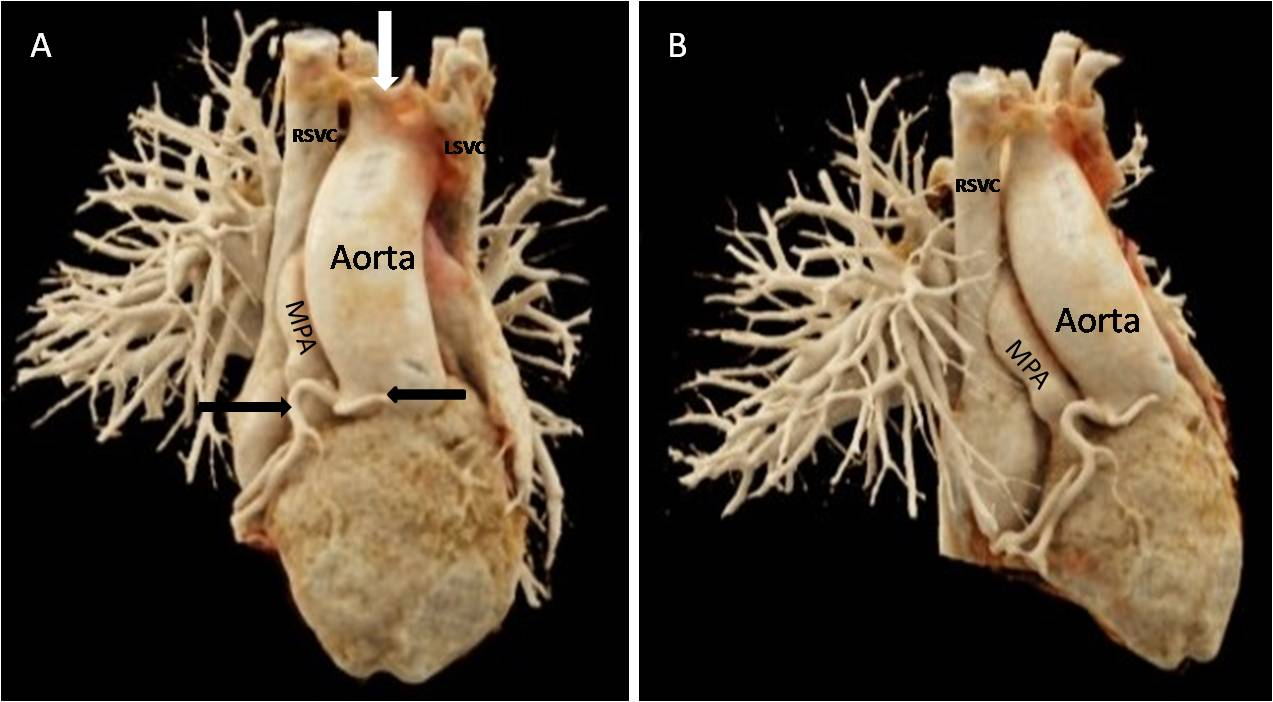
Figure 4 (A) and (B) Volume rendered CT images showing double superior vena cava (SVC) with intervening connecting vein (marked by white arrow), origin of main pulmonary artery (MPA)and aorta from right ventricle with common origin of right coronary artery and left anterior descending artery (marked by black arrows).
Unilateral absence of the pulmonary artery (UAPA) is a rare congenital heart defect characterized by the absence or severe underdevelopment of one pulmonary artery, leading to reduced blood flow to the corresponding lung. Embryologically, extrapulmonary pulmonary arteries develop from the proximal part of the embryological sixth aortic arch, while intrapulmonary pulmonary arteries develop from the lung buds. UAPA is believed to arise from the involution of the embryonic sixth aortic arch at the proximal level.1 It occurs more frequently on the right side. Left-sided pulmonary atresia is commonly associated with other congenital cardiac abnormalities such as tetralogy of Fallot, transposition of the great arteries, septal defects, and truncus arteriosus, and is referred to as non-isolated type pulmonary agenesis. Right-sided pulmonary artery agenesis is usually not associated with cardiac anomalies and is referred to as isolated unilateral pulmonary artery agenesis.2,3 A right-sided aortic arch is usually present with an absent left PA, whereas those with an absent right PA typically have normal anatomy.4 Due to inadequate blood supply to one of the lungs, collaterals develop in the thorax from multiple sources, including bronchial arteries, phrenic arteries, internal thoracic arteries, and subclavian arteries. These branches can sometimes lead to the reformation of the distal branches of the affected artery.5 Patients typically present with congestive heart failure or pulmonary hypertension in infancy, and with dyspnoea, chest pain, recurrent pulmonary infections, and haemoptysis in adulthood.
Diagnosis is usually made using a combination of radiological investigations and echocardiography. A chest radiograph typically reveals a small affected hemithorax with an absent hilar vasculature shadow and hyperinflation of the contralateral lung. On cross-sectional imaging, the pulmonary artery is absent, with termination within 1 cm of its origin. Intact peripheral pulmonary artery branches, multiple collateral formations, and parenchymal changes such as volume loss, interstitial changes, bronchiectatic alterations, or bullae formation can be seen as secondary findings.5,6 Therapeutic approaches are typically based on the patient's symptoms. No treatment is needed if there is no cardiopulmonary dysfunction. Medical management is focused on pulmonary hypertension. Surgical interventions depend on the development of the intrapulmonary arteries. Primary anastomosis with the central PA is performed when intrapulmonary arteries are well-formed, while a modified Blalock-Taussig shunt is used when intrapulmonary arteries are small. In cases of massive haemoptysis, selective embolisation of systemic collaterals may be required. For patients with severe recurrent pulmonary infections, lobectomy or pneumonectomy might be considered.
UAPA is a rare and challenging condition requiring a high index of suspicion for diagnosis. Timely recognition and management are crucial to preventing complications and improving patient outcomes. Multimodal imaging is often essential for anatomical localization, diagnostic accuracy, and surgical planning.
Authors confirm that the manuscript is solely submitted to the journal and not submitted/ being considered anywhere else .
Authors declare no conflicts of interest.

©2025 Sharma, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.