Journal of
eISSN: 2373-6437


Research Article Volume 17 Issue 2
A.N. Bakulev National Medical Research Center of Cardiovascular Surgery, Moscow, Russian Federation
Correspondence: Kazaryan Artak Varuganovich, A.N. Bakulev National Medical Research Center of Cardiovascular Surgery, Moscow, Russian Federation
Received: March 05, 2025 | Published: March 20, 2025
Citation: Sigaev IY, Kazaryan AV, Starostin MV, et al. Primary and repeated coronary artery bypass grafting using minimally invasive extracorporeal circulation. J Anesth Crit Care Open Acces. 2025;17(2):36-38. DOI: 10.15406/jaccoa.2025.17.0618
Although most coronary artery bypass grafting (CABG) operations are performed through middle sternotomy using extracorporeal circulation, minimally invasive myocardial revascularization is increasingly being used in myocardial revascularization. Minimally invasive coronary artery bypass grafting is a revolutionary trend in cardiac surgery. Thanks to the use of modern high-tech means, patients with coronary heart disease undergo multiple coronary artery bypass grafting without extracorporeal circulation through a left-sided minithoracotomy. Minimally invasive cardiac surgery Coronary Artery Bypass Grafting (MICS CABG) is an attractive, possibly more suitable method than classic CABG, accompanied by minimal complications. This technique is safe, effective, and provides outstanding patient comfort and the possibility of safe re-access in the future, when myocardial ischemia returns. This technique provides good long-term results, comparable to conventional CABG. However, there is a group of patients in whom it is impossible to safely perform this operation (relative insufficiency of heart valves, cardiac arrhythmia, low ejection fraction of the left ventricle). These patients can undergo CABG using minimally invasive extracorporeal circulation.
Purpose: The aim of the study was to demonstrate the first experience of using the MiECC technique in MICS CABG with the assessment of hospital outcomes.
Material and methods: From January 2015 to January 2023, 89 mini-invasive CABG surgeries were performed in our department through left-sided mini-thoracotomy, of which seven operations were performed using a minimally invasive extracorporeal circuit of the first type.
Outcomes: In the group with MiECC in MICS CABG, there were no myocardial infarctions or deaths. Conclusion: The use of MiECC in MICS provides good in-hospital outcomes and can be used as a safe alternative for myocardial revascularization in primary and recurrent patients with CAD.
Keywords: coronary bypass surgery; thoracotomy, extracorporeal circulation, MICSCAB
The "gold standard" of coronary surgery is CABG through sternotomy in the conditions of extracorporeal circulation (ECC). The mortality rate with this technique is 1-2%, but the total frequency of postoperative complications reaches 20-25% (pneumonia, wound infection, myocardial infarction and stroke). In this regard, over the past twenty years, there has been a desire in coronary surgery to reduce surgical trauma (minimally invasive approaches) and reduce the ECC-associated systemic inflammatory response that determines hemostasis disorders and multiple organ failure.1,2 Minimally invasive coronary artery bypass grafting through left mini-thoracotomy is a relatively new CABG technology that has already shown good results.
Joseph T. McGinn and colleagues began operating in 2005, and the first results are reflected in a 2009 paper, n=450. Five years later, at a congress in Boston, the results of the operation were reported in 1038 patients with good results.3 The combination of minimally invasive cardiac surgery with a conventional contour reduces the number and severity of postoperative complications due to the integrity of the sternum, but does not save from ECC-associated complications. Performing CABG on a beating heart is not always possible and safe, and 10% of MICS CAB require ECC support.4,5 An alternative method is the technique of minimally invasive extracorporeal circulation (MIECC), which is devoid of the disadvantages of conventional ECC.
The aim of the study was to demonstrate the first experience of using the MiECC technique in MICS CABG with the assessment of hospital outcomes.
From January 2015 to January 2023, 89 MICS CABG operations were performed in our department through left-sided mini-thoracotomy, of which 48 in primary patients and 41 in previously operated patients. The mean age of patients was 62.5±6.3 years; 88.8% men, 11.2% women. Most of the cases were males over 60 years of age. According to the Canadian classification, all patients had angina pectoris III–IV f.c. Most of the patients had a history of MI (52 (58.4%), the mean fraction of expulsion of the left ventricle was 55.7±5.4%, CABG without EСС was performed in 56 (63%) patients. In 33 (37%) patients, the operation was performed with classical parallel ECC through the common femoral artery and vein.
Outcomes
In 7 patients, the operation was performed in an infrared setting using a semi-closed minimally invasive extracorporeal circuit of the first type, which consists of a venous trunk, a centrifuge pump, an oxygenator, and an arterial trunk. The cardiotomy reservoir on the venous line is semi-flowing: wound blood can periodically return to a closed circuit or to the patient's cardiovascular system after treatment in a blood separator. We used a peripheral (femoral artery-femoral vein) circuit connection under the control of ultrasound of the heart (Figure 1 and 2). These patients with multivessel lesions of the coronary bed underwent 20 anastomoses under conditions of parallel normothermic ECC with full volumetric velocities (2.0-2.2 l/min/m2) and in auxiliary mode. In all cases, the full design perfusion rate was achieved. The average time of the ЕСС was 98 minutes, during which there was no abnormal course of the procedure. After performing anastomoses and completing hemostasis, the ЕСС was turned off at therapeutic doses of inotropic support. The duration of the operation was 354±90 minutes. Intraoperative blood loss was 339±128 ml. The average time of mechanical ventilation after surgery was just over 4,5 hours. The ventilation time was 16 hours; all patients were transferred from the ICU in 24 hours to the specialized unit and discharged from the hospital on the 7th day after surgery. In the group with MiECC in MICS CABG, there were no myocardial infarctions or deaths. All patients (n=89) were admitted to the ICU after surgery, where the state of central hemodynamics, the severity of heart failure, the duration of mechanical ventilation, doses of inotropic support, and the time spent in the department were assessed. According to the results, postoperative mortality was 2.2%, the incidence of type 5 MI was 3.3%, stroke was 1.1%, acute respiratory failure and heart failure were 5.5% and infectious complications were 3.3%. In general, the course of the early postoperative period was favorable.
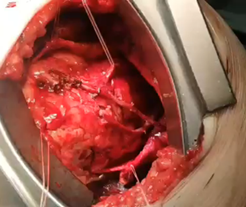
Figure 3 Redo minimally invasive cardiac surgery coronary artery bypass grafting through a left thoracotomy.
The normal course of the perfusion period indicates the safety of the technique even during the learning period. The uncomplicated course of the postoperative period in most patients indicates the effectiveness of the technique. More research is needed to establish reliable benefits.
|
|
The introduction of this method into wide clinical practice contributes to a significant reduction in wound, neurological, cardiac, vascular, respiratory complications of surgical intervention, a significant reduction in mortality, as well as a reduction in treatment costs associated with a reduction in the duration of the patient's stay in the intensive care unit and a reduction in the total bed day. The absence of total sternotomy has a positive effect on the mechanics of breathing in the postoperative period.
The MICS CAB technique with and without MIЕСС is safe, effective, provides greater comfort for the patient and in the future a safe re-access during the return of myocardial ischemia. Low trauma and high efficiency of the method allow us to consider it as a useful alternative to standard CABG.
None.
Conflict of interest is not declared.
The study did not have sponsorship.

©2025 Sigaev, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.