Journal of
eISSN: 2572-8466


Review Article Volume 11 Issue 1
Department of Biotechnology, California State University, Channel Islands, USA
Correspondence: Bill Tawil, Department of Bioengineering, UCLA School of Engineering, 420 Westwood Plaza, Room 5121, Engineering V. P.O. Box: 951600, Los Angeles, CA 90095-1600, USA
Received: January 05, 2024 | Published: January 18, 2024
Citation: Foo Suanhow, Tawil B. Future trends in endodontics. J Appl Biotechnol Bioeng. 2024;11(1):1-4. DOI: 10.15406/jabb.2024.11.00350
Since the beginning of the endodontic specialty, we see new technologies constantly being developed to help the endodontist in improving root canal therapy techniques. I have investigated some of the newer materials and technology in the field of endodontics. These include cone beam, dynamic navigation, pulp regeneration, magnetic resonance imaging, pulse oximetry, membranes and bone grafts.
Keywords: endodontics, endodontic regeneration, cone beam computed tomography, bone graft, dynamic navigation, magnetic resonance imaging, pulse oximetry
CBCT, cone beam computed tomography; MRI, magnetic resonance imaging
Endodontics is the study and techniques involved in treating a diseased root canal system.1 The dental pulp is the soft tissue in the middle of the tooth.2 The root canal contains nerves and blood vessels that support tooth function.1 When this system becomes irreversibly damaged, then a root canal therapy must be performed.1 This procedure involves cleaning, shaping, and obturation of the root canal system.1 Many students find endodontics an interesting subject.3
The idea of the root canal system dates back to the 1700s where Anton Van Leeuwenhoek described a diseased tooth as having inflammation in the pulp.4 Around thirty years later, the father of dentistry, Pierre Fauchard wrote in his book that in order to relieve the inflamed tooth, you must open the tooth to drain the pus to relieve the abscess.5 It was in 1944 that the American Association of Endodontics was created in Chicago and officially defined endodontics as an established field.6 In 1967, the American Dental Association recognized endodontics as a specialty in dentistry.6 An interesting fact about anesthesia, cocaine was used to anesthetize the maxillary incisor by Dr. Charles Nash in 1884.7 This was the first time anesthetic conduction was used in dentistry or medicine. We have come a long way since then. Dentist now mostly use amide based anesthetics.8
Success rate of root canal therapy by an endodontist
Having and endodontist perform your root canal therapy may be more costly than a general dentist.9 However, the endodontist will have a higher success rate than the general dentist.10 In a 2004 study, general dentist had a success rate of 89.7% and the endodontists had a 98.1% success rate during a 5 year follow up study.
Endodontic regeneration
Even though root canal therapy is an effective tool to save teeth that have been compromised by infection or trauma, endodontists have been looking for ways to improve the survival of teeth suffering from pulp infection.11 One of these ways is endodontic regeneration. For endodontic regeneration, the diseased tooth is disinfected with a combination of minocycline, ciprofloxacin, metronidazole. Then a mineral trioxide aggregate is placed to encourage cell growth into the root canal space. This multi visit method, allows the clinician to revitalize the tooth instead of just cleaning and filling the root canal with an artificial material.11
Regeneration works well in younger less developed teeth with larger apices,12 however recent studies show that It can work in mature dentition as well.13 Furthermore, teeth that were not formed properly during pulp regeneration tend to have better success than teeth that had suffered a trauma.14
Cone beam computed tomography
In addition to two dimensional radiographs, endodontists can use cone beam computed tomography (CBCT). These machines have shown to be more accurate in measurement than traditional radiographs.15 In studies with cadavers, it was found that CBCTs can accurately measure the volume of lesions.16 Prior to surgeries, CBCTs can help identify fenestrations.17 In studies pertaining to dental injuries, CBCTs were more accurate than intraoral radiography.18 A study using extracted teeth found that CBCTs are similar to normal radiographs when determining working length of the root canal. CBCTs were more accurate in identifying extrusive luxations, horizontal root fractures, cortical plate fractures, and lateral luxations.19 A case report demonstrated removal of excess extruded material from a previous root canal therapy using a surgical guide.20 This technique allowed a precise surgical procedure without perforating the sinus membrane (Figure 1).

Figure 1 Cone beam system.
Source: Genoray America Home Page. genorayamerica.com/dental/papaya3d_premium/.
Augmented reality and 3 dimensional dynamic navigation system
The latest technology in surgical endodontic procedures is the use of augmented reality along with 3D dynamic navigation system (DNS). This allows the operator to see in real time the position of the surgical instrument within the surgical site on a computer screen.21 Early research shows that this method improves the time efficiency for surgical procedures when compared to 3D dynamic navigation alone. DNS can help the operator locate intraosseous anesthetic injection sites and calcified portion of the root system.22 When doing an apicoectomy surgical procedure, the skilled operator can successfully perform a root resection with both the traditional method and with the dynamic imaging method.23 However, the dynamic navigation tends to benefit the inexperienced operator, which is helpful for beginners. DNS appears to be less technique sensitive and more efficient to use when compared to static imaging techniques as a guide during root end surgeries.24 Endodontic surgeries with dynamic navigation also results in smaller osteotomy sites and faster surgeries.25 For challenging tooth morphologies, the dynamic navigation system allows the operator to be more accurate and decrease preparation time for root end surgeries (Figure 2).26
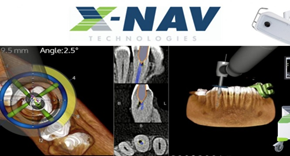
Figure 2 Dynamic surgical system.
Source: “Nav Home - X-Nav Technologies.” X, 6 Sept. 2023, x-navtech.com/.
Magnetic resonance imaging
As technology progresses, MRIs have been considered as an imaging option for endodontists. A proof of study demonstrated that one can accurately use MRIs to guide endodontic cavity access preparation.27 There is also very little difference in sensitivity and specificity between MRIs and CBCTs when used to detect vertical root fractures.28 The complex anatomy of the root system can also be visualized with MRIs without the radiation exposure.29 MRIs have the advantage of detecting soft tissue lesions and malignant spread of disease into cortical bone whereas the CBCT may have difficulties in this area.30 The MRI can be effective in not only revealing dental pathologies, but also expose intra-cranial lesions, optic nerve gliomas, retinoblastomas, and neuroblastomas.31
Membranes and bone grafts
The endodontist can also utilize membranes to keep out epithelial and fibroblast cells from invading a healing apicoectomy site to increase bone formation.32 It is believed that adding bone graft after an endodontic surgery may help accelerate bone formation in the surgical site.33 One study showed that in larger defect sites, bovine bone with a membrane healed better than without the use of membranes and grafts (Figure 3).34

Figure 3 Bone graft material.
Source: Geistlich North America Home Page. geistlich-na.com/dental-professionals/bone-substitutes/geistlich-bio-os.
There are several types of bone graft that can be used. These include xenografts, autografts, growth factors, allografts, and synthetic.35 However, autogenous bone is considered the gold standard as it is the most biocompatible.36 Researchers have also looked into teeth as possible bone grafting material based on similar properties with bone.37 Collagen membranes are not only for bone healing, but they can also be used in regenerative endodontics.38 They essentially act as a scaffold for new cells as they grow into the canal system.
Pulse oximetry in dentistry
The use of the pulse oximeter in endodontics has been ongoing for many years. We can see that it does have some potential uses. As far back as 1996, an in vitro study showed that the pulse oximeter could detect oxygen saturation in a model, starting a series of experiments leading up to clinical studies on this topic.39 A 2003 study showed that the pulse oximeter can be more effective than the traditional electrical pulp testing in that with necrotic teeth, the pulse oximeter will show decrease oxygen saturation, whereas the electrical pulp tester will have increasing readings.40 The largest problem for using pulse oximeters is creating an appropriately sized machine to fit in the mouth with ease of use.41 Another problem with using pulse oximeters is that with the varying oxygen saturation rates with each type of teeth.42 For example, the mean oxygen saturation for the central incisor will differ from the lateral incisor.
Endodontics involves the use of new materials and imaging devices to plan and create a successful outcome. Before the use of 3D imaging or microscopes, the endodontic procedure was all about x-rays and manual dexterity. The nonstop development of new technologies will only enhance the success of endodontics. However, technology cannot replace the endodontist. It is the endodontist who will make the diagnosis with the use of intuition, tests, and technologies.
Suanhow Howard Foo extends his gratitude to Dr. Tawil for the guidance provided during the fall semester of 2023, where he gained substantial knowledge in biotechnology at CSUCI. Additionally, he wishes to express his thanks to Dr. Tawil for assisting in arranging the publication of this paper.
Authors declare that there is no conflict of interest.

©2024 Foo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.