eISSN: 2574-9838


Research Article Volume 6 Issue 3
Department of Pain Clinic, Center of endosurgery and lithotripsy (CELT), Russia
Correspondence: AG Voloshin, Department of Pain Clinic, Center of endosurgery and lithotripsy (CELT), Moscow, Russia, Tel +79037742231
Received: April 01, 2021 | Published: May 14, 2021
Citation: Voloshin AG. The efficacy of epidural pulsed radiofrequency on radicular pain refractory to dorsal root ganglion pulsed radiofrequency treatment. Int Phys Med Rehab J. 2021;6(3):61-65. DOI: 10.15406/ipmrj.2021.06.00283
Background: Radicular pain is one of the most common types of pain, with an approximate prevalence ranging from 13 to 40%. The most common cause of radicular pain is a herniated disk or degenerative stenosis in the paramedian zone of the spinal canal, with damage to the nerve root above the foramina.
Objective: The aim of this retrospective study was to evaluate the efficacy of epidural pulsed radiofrequency (PRF) in the treatment of radicular pain after failed epidural steroid injection (ESI) and dorsal root ganglion pulsed radiofrequency (DRG-PRF) attempts.
Methods: Epidural pulsed radiofrequency was performed on seven patients suffering from radicular pain in L3-S1 dermatomes with anatomical causes, which correlated with the clinical evaluation and radiological findings. PRF was applied in monopolar mode with the following characteristics: frequency 2 Hz (20 ms pulse, 480 ms pause), amplitude 65V, exposure time 360 sec, temperature in the action zone not exceeding 42 degrees Celsius.
Results: The effect duration lasted from 4 months to more than one year in 4 patients. The minimum time to relapse was less than 2 weeks, with a maximum duration of more than a year. The absence of pain allowed responders to discontinue basic analgesic therapy. Increasing the activity, rated by them as "substantial" (3 QoL points or more) a month after the procedure, was noted by 5 patients.A year later, the improvement was maintained in 4 patients.
Limitations: The main limitation of this study is the small sample size of heterogeneous patients and the absence of a comparison group.
Conclusions: Our findings suggest that the epidural PRF is a useful option for treating radicular pain after unsuccessful attempts of the ESI and PRF of DRG for long-term effects. Efficacy of an ePRF can depend not only on the stimulation parameters but also on the point of action.
Keywords: radicular pain, epidural pulsed radiofrequency, dorsal root ganglion radiofrequency, RCE-electrode
DRG-PRF, dorsal root ganglion pulsed radiofrequency; ePRF, epidural pulsed radiofrequency; ESI, epidural steroid injection; PRF, pulsed radiofrequency; QoL, quality of life; RFA, radiofrequency ablation
Radicular pain is one of the most common pathologies for consulting pain specialists worldwide. The approximate prevalence is from 13 to 40%, depending on the clinical profile.1 The highest frequency of reported impairment is in the lumbar region, which is most often affected by degenerative changes.2 One of the most frequent manifestations of radicular pain is neuropathic pain in the corresponding dermatome, which manifests itself in certain positions or is provoked by certain movements.3 Radicular pain is most often subjected to surgical treatment, based on the mechanistic principle of treatment, which after a few years often turns out to be untenable.4
On the other hand, conservative treatment often does not provide significant pain relief for patients. The most commonly used nonpharmacological treatment methods, such as traction, physical therapy, and lifestyle modification, have very little effectiveness and a long duration of onset of effect. Additionally, NSAIDs and similar drugs have low efficiency due to missing the point of pathogenetic action. Anticonvulsants, drugs that are used for neuropathic pain, are usually poorly tolerated due to frequent side effects. Moreover, most of these drugs are not recommended for use in the elderly because of the high risk of serious adverse events. The most frequent patients of pain clinics are elderly patients who are burdened by comorbid pathologies.5
The standard of treatment for radicular pain in pain clinics is epidural steroid injection (ESI).6 The most commonly used transforaminal access is somewhat less intralaminar. Targeted therapy with the application of steroids has a pathogenetically sound rationale and has shown a good clinical effect with good tolerability.7 However, clinical practice patterns suggest that only up to 3-4 injections may be used for acute radicular pain syndromes. At the same time, the total dose of methylprednisolone should probably not exceed approximately 3 mg/kg of body weightto prevent excessive salt and water retention.8 This contradiction confuses many practitioners in terms of the safe total dose and frequency of injections for patients and can widely restrain the use of ESI for radicular pain treatment.
A relatively new promising method of pulsed radiofrequency (PRF) of the dorsal root ganglion has appeared, which is based not on the pharmacological effect but on the application of an electromagnetic field.9 Unlike traditional thermal radiofrequency ablation (RFA), the structure of the nerve fiber is not damaged, but only the functioning of the nerve is changed, which potentially brings substantial pain relief to patients for a long time. The clinical application of this method demonstrates encouraging results that are, at least, comparable to those of traditional interventional treatment, epidural steroid injections, and PRF has a better safety profile.10 The typical point of application of PRF is the dorsal root ganglion (DRG-PRF), in which classic transforaminal access is achieved.11 Thanks to the work of many researchers, we imagine how the electromagnetic field spreads around the tip of the cannula, so we can confidently assume that the zone of influence of the electromagnetic field involves the dorsal ganglion root in the coverage area.12 Nevertheless, for greater accuracy in the complete processing of such a relatively large structure as the spinal ganglion, some researchers suggest using bipolar mode PRF.13,14 Unfortunately, the most common cause of radicular pain is a herniated disk or degenerative stenosis in the paramedian zone of the spinal canal, with damage to the nerve root above the foramina. Insulated foraminal stenosis with clinical manifestations in direct causes of radicular pain is found in only 8-11% of cases.15
The aim of this study was to evaluate the efficacy of epidural PRF in the treatment of radicular pain after failed ESI and DRG-RPF attempts.
All patients were informed verbally about the study experimental protocol and written informed consent was obtained. The patients were recognized as pharmacoresistant and were denied the surgical procedure or they themselves categorically refused surgery. The procedure was remained the only pain relief method for these patients. This retrospective study protocol was approved by the local ethics committee of the Center of endosurgery and lithotripsy (CELT) Moscow, Russia in accordance to the Declaration of Helsinki. Informed written consent was obtained from the patients for participation in this study and publication of these accompanying images.
The patient selection criteria for this treatment were as follows:
Contraindications to the procedure were standard contraindications for spinal interventional procedures, such as the patient’s refusal, the patient’s inability to understand and agree to the essence of the procedure and the intended intervention, hypocoagulation of any reason, infection, and the presence of a psychiatric disease that impedes the procedure.
All procedures were performed in the operating room using all aseptic techniques for spinal and catheterizing procedures with real-time fluoroscopy. All procedures were performed by personnel with sufficient experience in performing spinal catheterization procedures in pain management. The patient was placed on a transparent X-ray table in a prone position. The ground pad was placed on the abdomen of the patient.
On the assumption of localization of the affected roots, we used classic caudal access to locate the introducer. From paramedian access, a puncture was performed in the hiatus sacralis; the Tuohy 16G introducer was placed at a level not higher than S3. The RCE electrode was moved through the introducer in the direction of the lumbar roots through the dorsal epidural space (Figure 1). There was no special protocol of fluid administration for hydrodissection or facilitating electrode conduction. The working tip of the electrode (15 mm) was located in the projection of the lateral canal opposite the exit zone and just dorsal to the affected nerve root, at the exact location of the determined nerve impairment or slightly proximal (Figure 2). After placement of the electrode, sensory stimulation was performed at 50 Hz, in the range of 0.3-0.5 V, and a typical sensation response was obtained that accurately overlapped the painful area of the patient. Because theventral and dorsal branches are very close in the impact zone, motor stimulation with 2 Hz was often also effective, but with a slightly higher voltage, most often within 1 V. Provided that the impedance in the impact zone corresponded to a normal value (200–400 Ohm), the PRF was started in monopolar mode with the following characteristics: frequency 2 Hz (20 ms pulse, 480 ms pause), amplitude 65V, exposure time 360 sec, temperature in the action zone not exceeded 42 degrees Celsius. After the procedure, a water-soluble steroid was administered (dexamethasone, 8 mg) through the catheter (Figure 3). Patients remained in the hospital for at least 2 hours, upon expiration of the control period, and in the absence of warning signs, they were discharged home.
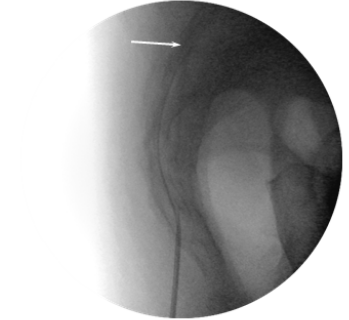
Figure 1 Lateral view. Introducer and RCE electrode in the sacral canal. Arrow – tip of the electrode.
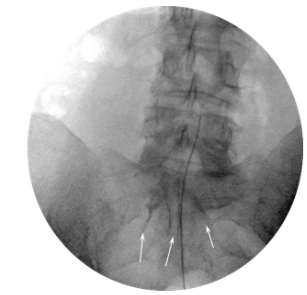
Figure 2 AP view. RCE electrode in lateral canal above the L5 nerve. Arrows – contrast material shown in the epidural space.
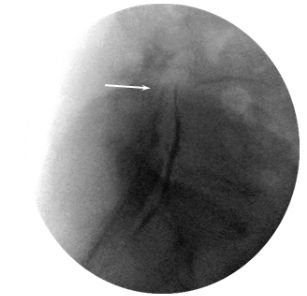
Figure 3 Lateral view. Contrast material spread into the dorsal and ventral epidural space. Arrow – tip of the RCE electrode.
Outcome measures
The follow-up duration after the procedure was 12 months. In our opinion, an important goal was to not only reduce the intensity of pain and pain relief by 50% or more but also to increase the duration of the effect, which is not a lesser and sometimes is a more momentous criterion of the efficacy of treatment. Thus, pain intensity at rest and during activity was measured with a 0-10 numeric rating scale (NRS), but the primary endpoint was not pain intensity and not pain relief, but the duration of the period with more than 50% NRS pain relief. A substantial effect of interventional treatment for chronic pain is not only a decrease in the intensity of pain but also an increase in mobility and daily social activity. The quality of life and daily activity were evaluated in all patients. QoL was evaluated before the procedure and at 6 and 12 months after the procedure using the American Association of Chronic Pain QoL Scale (16).
All patients noted the complete disappearance of pain immediately after the procedure. An early recurrence of pain intensity (earlier than two weeks) occurred in 3 patients. In the other patients, the effect duration was from 4 months to more than one year. The absence of pain has allowed these patients to discontinue basic analgesic therapy. In general, four patients experienced pain of the same localization and intensity during the year. The distribution of recurrence time is shown in Figure 4.
According to our results, the minimum recurrence time was less than 2 weeks, with a maximum of more than a year.
Increasing the activity, rated by them as "substantial" (3 QoL points or more) a month after the procedure, was noted by 71% of patients. A year later, the improvement was maintained in 43% of patients. It is noteworthy that one patient, in the absence of a significant decrease in the intensity of pain, nevertheless noted an increase in social activity by 3 QoL points.
Adverse events and complications of the procedure were not recorded for any patient.
Some studies have reported the efficacy of epidural PRF for the treatment of radicular pain. The first announcement of this method was made in oncological patients, as transforaminal access was difficult due to the high risk of tumor perforation or technical problems.17,18 At the same time, in 2015, the Cologne University Clinic published the results of treatment of 188 patients over 7 years, in which ePRF was used as a patient selection stage for chronic neuromodulation and was effective in 63.8% of patients, while the frequency of complications was very low, less than 1%.19 The encouraging results of using ePRF in patients with radicular pain confirm the importance of the selection of devices and parameters for the procedure. It is very important that the effect continues for months; however, a decrease in the intensity of pain by approximately 30% from the initial intensity can be perceived by most patients as unsatisfactory.20
The mechanism of action of PRF has remained a subject of discussion from its initial application. There are several theories explaining the mechanism of action of the PRF:
Controlled heating
In the late 1980s, there was an idea that temperature fluctuations around the tip of the cannula provided enough damage to the nerve fiber, without too much damage to the nervous structure itself.21 Further studies have shown that this is not entirely true. In particular, there was evidence of the efficacy of PRF at the point of use distal to the site of injury, which required new answers.
Immune theory
After the successful use of intraarticular PRF, researchers recorded local changes in the immune system.22,23 An opinion has emerged that the analgesic effect of PRF is not connected with the effect on the nerve itself but with the local response of the immune system. While the immune system is very complex and is involved in countless pathological processes based on current knowledge, it is difficult to say how this theory is consistent.
Changes in the dorsal horn. It was found that the application of both RFA and PRF to the DRG induces the expression of c-fos in the dorsal horn of the spinal cord.24 Whether this result has clinical significance has not been fully elucidated. C-fos is a nonspecific marker indicating cellular activity. The hypothesis that these changes may affect the descending inhibitory paths of the antinociceptive system remains unconfirmed thus far.25,26
Electromagnetic field
ionic oscillations. Radiofrequency creates two types of fields at the tip of the cannula: electric and magnetic. At low frequencies, less than 500 kHz, the magnetic field strength is slight; therefore, the effect of the PRF is mainly associated with an electric field, oscillations in which cause the movement of ions with sufficient flow density and, as a result, tension on the cell membrane with uncontrolled opening of all voltage-gated channels. According to this theory, it is the E-field that, with a high density of ion flow, creates ion friction and heat, which, in turn, heats the surrounding tissues27 and leads to intracellular changes, such as mitochondrial swelling, more pronounced in C-fibers than in A-fibers.28 Therefore, this reverses the cause and effect of the first theory — it is not the heat released by the cannula that affects the cell membranes, but the ionic friction and the change in the potential of the membranes that heat the cannula. Thus, today, there are two global approaches to understanding the action of the PRF — the “destructive” mechanism that connects the main action with controlled destruction, mainly based on membrane and intracellular changes, and the “neuromodulation” aspect that binds the efficacy of the PRF with the regulatory mechanisms of nerve functioning.
Regardless of the dominant theory, it remains unclear how far waves from the point of impact can achieve a therapeutic effect. Within the concept of local controlled damage, it is likely that this zone will be very small. With local neuromodulation, the zone of initiation will also remain local, but how far are the changes spread to it? Fundamental physical and biological knowledge maintains that waves tend to fade out with distance and time. However, there is research on the clinical effect over more than 8 vertebral segments – from S3 to Th12. The authors suggest that caudal PRF may use the efferent parasympathetic pathway and the cholinergic anti-inflammatory system to achieve a long-term effect.29 These results are very promising and require more careful study, subject to more rigorously controlled studies.
In any case, there is no unambiguous or even distinct answer about the dominant mechanism of action of the PRF. It is likely that many factors play various roles, which means that a "single neuromodulation" effect, irrespective of the dominant mechanism of action, such as the effects on membrane and mitochondrial conditions or even controlled damage with an immune response, is likely to be the most practical mechanism that can be targeted as close as possible to the point of nerve impairment. It is likely that the ePRF zone should cover either the area of nerve damage or be located proximal to the damaged area.
Why is "single-shot" modulation and do not chronic neuromodulation used for treating radicular pain? All patients had indications for spinal cord stimulation, such as 1. The presence of pharmacoresistant neuropathic pain; 2. The absence of contraindications for implantation of a neuromodulation system; 3. The presence of "organic" pain; or 4. The presence of well-localized pain in the area of dermatomes. However, these patients also had relative contraindications for spinal cord stimulator implantation such as:1. Age presents a very relative, but in the opinion of patients, significant contraindication, which is associated with their fear of new devices due to the inability to control them. 2. Indications for "anatomical" treatment, such as an surgery that could determinate the cause of the pain, may seem more attractive. 3. Dynamic pain, which has a clear relation with the position of the body, is a significant limitation, which echoes the previous one and can significantly worsen the prognosis of chronic spinal cord stimulation. Given the importance of the patient's opinion before implanting any devices, it was decided to refrain from chronic spinal cord stimulation.
The main limitation of this study is the small sample size of heterogeneous patients and the absence of a comparison group.
After our study, it is not clear enough whether the effect of the ePRF on the nervous structure is dominant or whether a locally administered steroid has a prominent effect, the advantage of which is in more targeted localization than with the intralaminar or transforaminal administration. It can only be noted that previous steroid injections were not successful.
Additionally, due to the small number of procedures performed, it is not fully understood whether repeated procedures are sufficiently safe due to the potential risk of hemorrhagic complications because procedures that require catheterization of the epidural space involve a high risk of hemorrhagic complications, and it may be unsafe to perform them unnecessarily or frequently.30
Our findings suggest that theepidural PRF is a useful option for treating radicular pain after unsuccessful attempts of the ESI and PRF of DRG for long-term effects. Efficacy of an ePRF can depend not only on the stimulation parameters but also on the point of action.
None.
The authors declare no conflict of interest.

©2021 Voloshin. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.