International Journal of
eISSN: 2381-1803


Research Article Volume 17 Issue 6
1Medicine Course, FTC University Center, Salvador, Bahia, Brazil
2FTC University Center, Salvador, Bahia, Brazil
3Faculty of Medicine, FTC University Center, Salvador, Bahia, Brazil
4Imagepat - Pathological Anatomy Laboratory – Salvador, Bahia, Brazil
Correspondence: Luiza Helena Castro Souza Lopo, Medicine Course, FTC University Center, Salvador, Bahia, Brazil
Received: December 10, 2024 | Published: December 27, 2024
Citation: Lopo LHCS, Paixão LS, Reina FN, et al. Clinical and epidemiological profile analysis of patients submitted to hepatic transplantation in a reference pathological anatomy laboratory in Salvador-ba. Int J Complement Alt Med. 2024;17(6):273-276. DOI: 10.15406/ijcam.2024.17.00716
Introduction: Liver Transplantation is a surgical procedure that consists of exchanging a diseased liver for a healthy one, from an organ donation, whose main objectives are to prolong and improve the patient's quality of life. According to the Brazilian Transplant Registry in 2020, liver transplants decreased by 9%. The Northeast is one of the regions that represented the highest rate of reduction, around 33.7%. Several clinical conditions meet the criteria for Liver Transplantation. Among them are Liver Cirrhosis, especially from alcohol drinking and hepatitis B and hepatitis C viruses; Acute Liver Failure; Primary Liver Neoplasms such as Hepatocellular Carcinoma (HCC); Biliary Atresia; Autoimmune Hepatitis; some Metabolic Diseases capable of severely altering hepatobiliary function (such as Wilson's Disease, Hemochromatosis, alpha 1- Antitrypsin Deficiency); among others.
Objective: To describe the clinical and epidemiological profile of patients undergoing liver transplantation in a reference pathological anatomy laboratory in Salvador-BA, in the period 2011-2020.
Methods: This is an observational, descriptive, and cross-sectional epidemiological study. The review of medical reports with a time frame of 2011 to 2020 was used as a data source.
Results: It was shown that, of the 270 medical records, only 79 patients underwent liver transplantation - among which 86.08% were male, 53.96% were between 65 and 79 years old, 87.34% had undergone a biopsy through the private medical service, and 43.04% had not provided information about the municipality of residence. Conclusion: The characterization of the profile of transplanted patients makes it possible to intensify the care service for this Risk Group, allowing for the taking of necessary measures for health care, and intervention in this matter.
Keywords: liver transplantation, liver disease, epidemiology, salvador
Liver transplantation (LT) is a surgical procedure that consists of exchanging a diseased liver for a healthy one from a donor, with one of the main objectives being to prolong and improve the quality of life of patients with advanced liver disease.1,2 Liver transplantation is currently a therapeutic modality used in patients with terminal liver disease or in patients who develop severe acute liver disease.3 Liver transplantation has always fascinated mankind, with reports in literature dating back to ancient civilizations. On March 1, 1963, Starzl described the first unsuccessful attempt on humans. In Brazil, the pioneering transplant attempt took place in 1968, at the Hospital das Clínicas of the Faculty of Medicine of the University of São Paulo4 - the patient died 7 days after the procedure, secondary to an infectious process and rejection of the graft.1 The refinement of surgical techniques, the development of effective organ preservation methods5 and the presence of powerful immunosuppressive drugs have significantly reduced organ rejection.6 HT then became a medical therapy, leaving the experimental field, enjoying wide acceptance, and being used for individuals of practically all ages.7,8
Brazil has one of the largest public organ and tissue transplant programs in the world.9 According to a study carried out by the University of Brasilia, Ceilândia faculty, data on actual solid organ transplants between 2001 and 2017 was evaluated. This study found that liver transplants were the second most common, accounting for 22.1% of all procedures carried out in this period.10 According to the Brazilian Transplant Registry, in 2020, there was a 9% decrease in liver transplants, with the Northeast being one of the regions that accounted for the highest rate of reduction, around 33.7%.11 The number of patients on the waiting list for liver transplants is steadily increasing. One of the biggest challenges in the area of HT is the insufficient number of donors for the growing demand of candidates for this surgical procedure.10
In 1997, through Decree Law No. 2,268, the Ministry of Health created the National Transplant System (SNT) and the Organ Notification, Procurement and Distribution Centers (CNCDO) (5). In 2018, there were 7 authorized centers in the state of Bahia.10 A new policy for allocating patients who to undergo liver transplantation was adopted, starting with Ordinance no. 1,160 (on May 29, 2006). The MELD (Model for End-Stage Liver Disease) scale was introduced for adults and adolescents over 12 years of age, and the PELD (Pediatric End-stage Liver Disease) scale for children under 12. As a result, the waiting list for the procedure was organized according to the severity of the patient, instead of the order of registration.5,12 Currently, Ordinance No. 2600, of October 21, 2009, governs the liver transplant system, and aims to remedy the inequalities in distribution between the units of the Federation. It is important to note that, although the national registry is a single one, the distribution of organs donated due to brain death was initially done at state level and later by macro-regions.12,13
In addition to the MELD scale, the Child Turcotte-Pugh (CTP) classification helps establish priority for liver transplantation, disease prognosis, predict survival and mortality after transplantation, and can serve as a parameter for assessing health-related quality of life.14 There are a number of clinical conditions that lead patients to the liver transplant queue. These include liver cirrhosis, especially due to alcohol consumption and the hepatitis B and C viruses; acute liver failure; primary liver neoplasms, such as hepatocellular carcinoma (HCC); biliary atresia; autoimmune hepatitis; some metabolic diseases capable of seriously altering hepatobiliary function (such as Wilson's disease, hemochromatosis, alpha-1-antitrypsin deficiency); among others.15,16 In view of this problem, the aim of this study is to describe the clinical and epidemiological profile of patients undergoing HT, considering the samples collected through the anatomopathological study of a reference laboratory in Salvador. The aim is to outline the profile of the main risk groups involved in this procedure.
This is an observational, descriptive, cross-sectional epidemiological study. The data source used was a review of medical reports from 2011 to 2020.
This study was carried out at IMAGEPAT SALVADOR, a pathological anatomy laboratory located in the Linus Pauling Medical Dental Center, at 119 Altino Serbeto de Barros Street, Itaigara district, in the city of Salvador, Bahia. The study population consisted of patients who had undergone a liver transplant procedure and whose biological material had been sent to IMAGEPAT SALVADOR within the time frame of interest. As an inclusion criterion, all the reports of patients with liver alterations who underwent biopsy or immunohistochemical examination were selected, with a total of 323 reports referring to 270 patients. Of these, only 79 underwent HT, and this was the study sample.
The sample was selected intentionally, according to the group of interest: all patients who underwent the liver transplant procedure and who requested pathological analysis within the time frame defined in the methodology. The sample size was calculated taking into account a population expectation of 3001 patients undergoing liver transplantation in Bahia, according to the Brazilian Transplant Registry (RBT), with a sampling error of 5% and reliability of 95%, estimating 341 patients. The variables considered included gender, age group in the SINAN (Information System for Notifiable Diseases), funding for the anatomopathological examination of the biopsies, municipality of residence, and post-perfusion biopsy.
The medical reports were assessed individually by the study's researchers. The data collected was transferred to a virtual form, developed by the authors of this study, with the variables of interest. This information was stored and tabulated in Microsoft Excel version 16, for descriptive statistical analysis and the preparation of tables/spreadsheets, according to the absolute and relative results. The information collected was preserved without exposing the names of the patients. In this way, the confidentiality of the holders of the medical records participating in this research was promoted. This study required the consent of IMAGEPAT, the pathological anatomy laboratory, and only began after authorization from the Ethics Committee of the UniFTC University Centre. A waiver of the ICF (Informed Consent Form) was requested, given that only data obtained from the study of material already collected was used. Therefore, there was no direct contact with the patients.
The total study sample consisted of 323 reports with some suspicion of liver alteration, from 2011 to 2020, at the IMAGEPAT SALVADOR Pathology Laboratory, corresponding to 270 patients analyzed. Graph 1 shows that 79 (29.6%) of these patients underwent liver transplantation, while the other 191 (70.74%) did not.
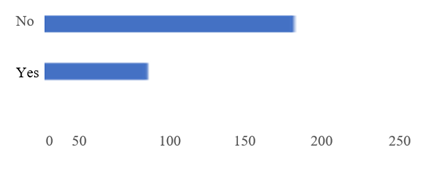
Graph 1 Regarding post-perfusion biopsy.
Source: own elaboration, based on data collected from the laboratory imagepat.
Graph 2 shows that 68 patients (86.08%) are male and the remaining 13.92% (11 patients) are female.
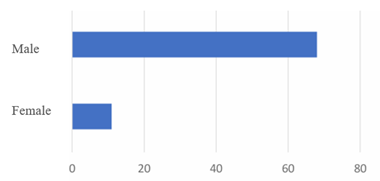
Graph 2 Regarding the sex of the patients transplanted.
Source: own elaboration, based on data collected from the Laboratory Imagepat.
Based on the information in Graph 3, which refers to the age range in the SINAN, there were no transplants among the patients: 1 to 19 years old; 20 to 34 years old, only 1 patient underwent this procedure (1.27%); 30 to 49 years old, 2 patients were transplanted (2.53%); 50 to 64 years old, 28 patients underwent this surgery (35.44%); from 65 to 79 years old, 45 patients underwent transplantation (56.96%); and 80 years or older, there were no transplanted patients. Of all the medical records analyzed, 3 did not have this variable recorded (3.80%).
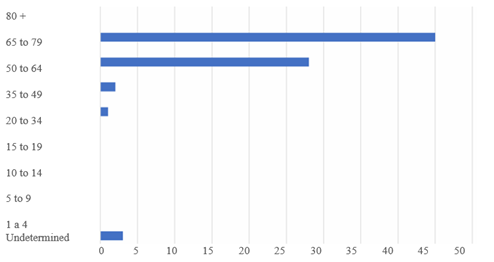
Graph 3 Regarding the divisions between the ages of SINAN and two transplant patients.
Source: own elaboration, based on data collected from the Laboratory Imagepat.
In view of the data shown in Graph 4, regarding the type of funding for the anatomopathological examination of the biopsies of transplant patients, 69 patients (87.44%) underwent this procedure through a private service, while only 10 patients (12.66%) were sponsored. There were no patients with biopsies sponsored by the Unified Health System in the sample studied.
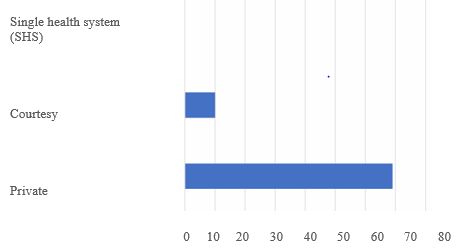
Graph 4 financing of the anatomopathological examination.
Source: own elaboration, based on data collected from the Laboratory Imagepat.
According to Table 1, 28 of the patients lived in Salvador (35.44%); another 17 lived in the countryside (21.52%); and 34 patients did not have this variable recorded (43.04%). Table 2 shows that 62.22% of the patients were from the capital and the other 37.78% were from the countryside.
|
Column 1 |
Column 2 |
Column 3 |
|
City of residence |
Quantity (n) |
Percentage(%) |
|
Salvador |
28 |
62,22% |
|
Countryside |
17 |
37,78% |
|
Total |
45 |
100% |
Table 1 Regarding the city of residence of transplant patients, removing those without data in the medical records
Source: own elaboration, based on data collected from the Laboratory Imagepat
|
Column 1 |
Column 2 |
Column 3 |
|
City of residence |
Quantity (n) |
Porcentage (%) |
|
Salvador |
28 |
33,44% |
|
Countryside |
17 |
21,52% |
|
No data |
34 |
43,04% |
|
Total |
79 |
100% |
Table 2 Regarding the city of residence of transplant patients
Source: own elaboration, based on data collected from the Laboratory Imagepat
Obtaining information from transplant patients' medical records was difficult due to incomplete records. Socioeconomic data, patient habits, skin color/race, level of education, profession, marital status, blood type and clinical history were all missing from the medical records. This limited a more complete epidemiological delineation of these patients.
Among the data found in this study, there was a higher prevalence of male patients (86.06%), in line with studies carried out in Ceará, with 62 patients, where 79% were men;17 and in the northwest of São Paulo, with 60 patients, where 80% were male.18 This result is probably due to certain particularities relating to the male population, such as the type of liver disease that affects them more; their lower demand for medical care; the fact that they are the target gender for alcoholism; the fact that they are more prevalent among injecting drug users; and the fact that they have more promiscuous sexual activity. These factors contribute to their increased exposure to viral diseases and alcoholic liver disease.19
Although liver transplantation is a treatment available to all age groups, in this study it was possible to see a greater predominance of this procedure in the 65-79 age group (56.96%), followed by the 50-64 age group (35.44%). According to an epidemiological study in Roraima20 and the Acre region,21 the most prevalent age group was 46 to 60 years old, representing 45.6% and 45% respectively in these states. This demonstrates the generally chronic and slow evolution of liver disease.19
As this study was conducted in a private laboratory, 87.34% of the biopsy reports came from private services and only 12.66% were courtesy reports. This variable has not been discussed in other literature.
As for the municipality of residence, 34 medical records did not record this variable, corresponding to 43.04%. Those that did (56.96%) were distributed as follows: 28 records, corresponding to 62.22%, in Salvador; and 17 records, totaling 37.7%, in the interior of the country. This information is in line with data from transplants carried out in Acre, where 81% of these patients lived in the capital Rio Branco.21 This can be explained by the need for periodic exams to update the MELD scale score on the transplant list. Patients with difficult access to the tests do not have their data updated and may be removed or remain inactive on the waiting list. In this way, the prevalence of reference centers located in the capitals highlights the panorama of inequality in relation to patients from the countryside.13
The pandemic scenario created by SARS CoV-2, decreed by the World Health Organization in 2020, has directly affected the global health system.22 With regard to the transplant community, there has been a reduction in the number of procedures performed and an increase in the waiting list. This unfavorable scenario may be linked to some situations: intensive care unit (ICU) beds being directed to patients infected with the new coronavirus; teams responsible for transplant operations being redirected to care for respiratory symptomatic patients, which has hampered the logistics of obtaining and transplanting organs; and some transplant programs having been suspended, as occurred, for example, in France.23
In Brazil, according to the Brazilian Organ Transplant Association, although the liver was the second largest solid organ transplanted before the pandemic (2009-2019), it was the least affected, with only a 10.8% decrease in 2020 (1506 cases), compared to 2019 (1620 cases). The biggest drop occurred in the Northeast region (37.1%). On average, in this same period, there was a 22% decrease in France, and 25% in the USA.23
Through the descriptive study of medical records carried out in this study, it was possible to construct an epidemiological overview of patients undergoing liver transplantation in Bahia, noting the predominance of males, aged between 65 and 79, from the capital, and who received help for the procedure from the private health system. However, these data may not reliably reflect the population of Bahia, since there was a shortage of current bibliographic sources in this region, a small sample available for collection, and because this was a study in a private laboratory in Salvador. The epidemiological profile is intended to help the health service develop strategies to promote public policies involving educational campaigns, social support measures to reduce alcohol abuse, among other measures aimed at preventing and treating the risk group.
None.
Author declares there are no conflicts of interest.

©2024 Lopo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.