International Journal of
eISSN: 2381-1803


Review Article Volume 18 Issue 3
Department of Nutrition, Exercise and Sports, University of Copenhagen, Denmark
Correspondence: Kaj Winther, Department of Nutrition, Exercise and Sports, Rolighedsvej 26, 1958, University of Copenhagen, Denmark
Received: May 01, 2025 | Published: May 16, 2025
Citation: Agergaard CK, Nielsen CC, Winther K. Can terpenes and/or terpenoids replace paracetamol and NSAID’s when treating pain in osteoarthritis – a review. Int J Complement Alt Med. 2025;18(3):87-95. DOI: 10.15406/ijcam.2025.18.00732
Background: Terpenes and terpenoids, naturally occurring compounds derived from plants, have shown potential in various therapeutic applications due to their anti-inflammatory, antioxidant, and analgesic properties. This review tries to elucidate the potential of terpenes and terpenoids in managing pain for patients with osteoarthritis in the knee and/or hip, and whether they can function as alternatives to conventional painkillers including paracetamol and NSAID’s.
Methods: A systematic literature review was conducted, resulting in the inclusion of ten studies, each either examining different classifications of terpenes and terpenoids alone or in combination with other bioactive compounds through various experimental designs. These studies were primarily assessed for their impact on pain reduction and secondary for possible impact on joint stiffness, activity of daily living and consumption of rescue medication.
Results: In eight out of ten studies, plant extracts containing terpenes and terpenoids significantly decreased overall pain, resulting in improvement in outcome measures such as WOMAC, VAS and LFI scores. A decline in joint stiffness and inflammation was observed in the remaining studies. It is proposed that cyclic triterpenoids, in particular, because of anti-inflammatory properties, may play a crucial role in pain management in osteoarthritis. It is also suggested that monoterpenes, diterpenes, and sesquiterpenes alone or in combination with other bioactive compounds, can have significant impact on pain.
Conclusion: Because of the variability in study design, dosages, duration of treatment and the fact that there at present are no human studies focusing on “pure” terpenes and/or terpenoids, it is difficult to conclude that a specific classification of terpenes and terpenoids would be effective. However, our findings emphasizes that terpenes and terpenoids should be further investigated as they in the future may partly replace rescue medication.
Keywords: pain, osteoarthritis, terpenes, terpenoids, anti-inflammation, rescue medication
The term terpenes originate from the word turpentine (lat. Balsamum terebinthinae) which is known as the strong smell that follows when cutting or carving the bark off of pine trees.1 About 30.000 terpenes, and their oxidized derivatives terpenoids, are known in the literature.1 Terpenes and terpenoids originate from various plants such as coriander, eucalyptus, lemon grass, lavender, peppermint, rosemary, rose-hip and many more. Terpenes and terpenoids play a big role in everyday life and appears as fragrances in perfumes, colors in our vegetables and fruits, and flavors in our spices or herbs. They can create bitter tastes to deter animals that might feed on them or can be used as medicaments for a variety of diseases.1 An interesting part of terpenes and terpenoids are their medicinal properties which also include their anti-inflammatory properties. As the majority of the middle aged and elderly population struggle with arthritis, see the description of osteoarthritis later, there is a widespread use of rescue medication including painkillers like paracetamol and NSAID’s. Unfortunately, paracetamol and NSAID’s have been linked to liver and kidney injury as well as cardiovascular and upper gastrointestinal complications.2–6 Such side-effects are not only a problem for the individuals who suffer from them, but they are also a problem and a cost to society.
To avoid the side effects from conventional painkillers, scientists have been studying plants to identify bioactive compounds such as polyphenols alkaloids, terpenes and terpenoids, which may offer pain relief comparable to paracetamol and NSAID’s producing less side effects. Although terpenes and terpenoids have recently garnered significant interest for their potential anti-inflammatory, anti-cancer, antioxidant, and antibacterial properties,7 many studies focus on plants containing multiple bioactive components, so it is possibly worth focusing on terpenes and terpenoids as monotherapy. Animal studies, either administering terpenes or terpenoids orally as monotherapy or through injections and also in vitro studies examining chondrocytes in both rats and humans, found that terpenes and terpenoids are able to mitigate chondrocyte injury, mediate anti-inflammatory signaling to exhibit chondroprotective activity, inhibit pro-inflammatory mediators and overall show promising antioxidant effects.8–12
Osteoarthritis and inflammatory mediators
Osteoarthritis (OA) is a common joint disease which affects the elderly and cause significant daily problems. It is defined as the deterioration of articular cartilage which leads to inflammation in the synovial cavity, found in synovial joints such as the knee, the elbow, the shoulder, and the hip.13 The main symptoms of OA are pain, stiffness, joint impairment, and reduced physical function.13 The reason for pain is still not completely understood, but include, increased intra-osseus (within the bone) pressure, ligament damage, capsular tension, or meniscal injury.13 Aging itself also modify the mechanical properties of the cartilage, including rearrangement of the cartilage matrix including aggrecan and collagen production and diminished hydration leading to increased degeneration of the cartilage.13 In mild OA, proliferation of chondrocytes dramatically accelerates because of the loss of matrix. As OA progresses, caused by either cartilage damage, inflammatory response or mechanical stresses, an extensive degradation and loss of cartilage matrix occurs. Some cytokines involved in OA are interleukin-1 (IL-1), IL-6 and IL-8 and tumor necrosis factor-α (TNF-α). These stimulate the production of proteases, nitric oxide (NO), and eicosanoids such as prostaglandins and leukotrienes, through macrophages or chondrocytes.13 The more production of these inflammatory mediators, the more cartilage damage, inhibition of matrix synthesis, and promotion of cellular apoptosis occurs.
Other inflammatory mediators in OA are proteases. Here matrix metalloproteinases (MMP’s) play a major role. MPP’s of importance in OA are MMP-1 and MMP-13 which are collagenases, an enzyme that degrade the collagen in the articular cartilage and MMP-3, also called stromelysin, which targets various components including collagen, proteoglycans, and glycoproteins in the cartilage tissue. ADAMT-4, known as aggrecanase, is also an enzyme that can degrade aggrecan.13 The cytokines IL-1 and TNF-α, can increase MMP expression and suppress MMP enzyme inhibitors.13
Lastly, the pro-inflammatory enzymes involved in OA are inducible NO synthase (iNOS), which can generate the free radical NO, the enzyme cyclooxygenase-2 (COX-2) which produces prostaglandin-2 (PGE2), and the enzyme 5-lipoxygenase (5-LOX) which converts arachidonic acid (AA) to eicosanoids.14 Additionally, the primary effect of TNF-α is to induce the cascades that express pathway genes such as NF-κB. This gene promotes the production of the abovementioned pro-inflammatory enzymes, as well as IL-1 which further stimulates the production of both PGE2 and NO which can contribute to cartilage damage by upregulating MMP`s.13,15 C-reactive protein (CRP) has also been associated with inflammation and OA progression.16 CRP is synthesized in the liver as a response to the secretion of inflammatory cytokines, such as IL-1, IL-6 and TNF-α.17 These proinflammatory cytokines increase the amount of CRP which will consequently support the inflammatory process.18 To get an overview of all inflammatory and anti-inflammatory mediators mentioned see Table A1 in Appendix.
Terpenes – Chemical structure and pathways
Terpenes and terpenoids are naturally occurring compounds built from isoprene units (C₅H₈), often referred to as isoprenoids, which is the foundation of the skeleton of terpenes.1 Structurally, they are categorized based on the number of isoprene units they contain: monoterpenes (C₁₀), sesquiterpenes (C₁₅), diterpenes (C₂₀), triterpenes (C₃₀), and tetraterpenes (C₄₀). When terpenes are modified by oxidation or structural rearrangement, they become terpenoids.19
Biosynthesis occurs through two main pathways in plants:
Among the various classes, diterpenes and triterpenes, particularly cyclic triterpenoids, have shown the most promising anti-inflammatory and pain-relieving effects, especially in relation to OA.
These compounds are typically found in:
While monoterpenes (e.g., limonene, myrcene, α-pinene) also exhibit anti-inflammatory effects, their efficacy in pain relief appears less pronounced than that of di- and triterpenes in current OA research (Figure 1).
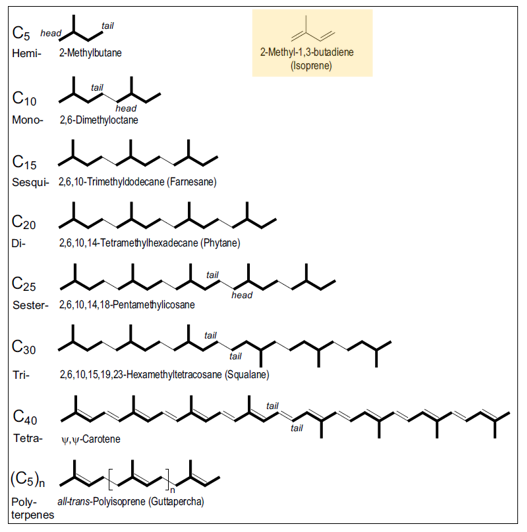
Figure 1 Categorization of terpenes and their structures.
Picture from Breitmaier, E. (2006)1. Terpenes: Flavors, fragrances, pharmaca, pheromones. WILEY-VCH Verlag GmbH & Co. KGaA, p.2. The basic carbon structure for terpenes, also called an isoprene unit, is given in the yellow box.
According to the isoprene rule, all terpenes and terpenoids are derived from the precursors isopentenyl pyrophosphate (IPP) and dimethylallyl pyrophosphate (DMAPP). These precursors are used for biosynthesis of terpenes and terpenoids with functions in growth and development.21
Terpenes and terpenoids in daily foods and their properties
Monoterpenes represent most fragrance in all classes of terpenes and terpenoids and can be found in various flowers, fruits, and leaves and is used in essential oils and fragrances.7 One of the main roles of monoterpenes is to attract pollinators to plants or to repel other organisms from feeding off the plants.7s
Types of monoterpenes found in natural plants are pinenes (both α-pinene and β-pinene), myrcene and limonene.7
Diterpenes are known for their physiological active groups such as vitamin A and is used as plant growth hormones as they influence and regulate crucial plant processes such as germination, flowering, and the transition between reproductive cycles.7
Sesquiterpenes are commonly found in the zingiberaceae family, which includes over 1400 species and has been widely used in Chinese and Indian medication to prevent and treat a wide range of pathologies.22 Among others, turmeric and ginger are known for their potent antioxidant and anti-inflammatory capacity.22
Turmeric features a complex and diverse composition, primarily consisting of terpenoids and phenolic compounds.22 The bioactive compounds in turmeric are predominantly curcuminoids which are also known for giving turmeric its yellow color, while they also have antioxidant properties and are crucial in combating oxidative stress and preventing various chronic diseases.22 Furthermore, the non-curcuminoid compounds such as the sesquiterpenes turmerones, elemene, bisacurone, curdione, germacrone, furanodiene and curcumol also exhibit significant biological activities.22
Additionally, it has recently been found that the extraction of Curcuma longa L, also known as white turmeric, contains high amounts of the diterpenoid labdane, especially the derivatives labdane 8 and 12-diene-15, and 16-dial.23 This is in contrast to the classic yellow turmeric, low in curcumin content and has an 80-100 times higher content of this diterpene.23 White turmeric has demonstrated anti-inflammatory properties just as ginger and yellow turmeric.23 Lastly, the primary bioactive compounds of ginger are the phenolic compounds such as gingerol and the sesquiterpenes, zingiberene, β-bisabolene, α-curcumene, α-farnesene, and β-sesquiphellandrene.22 Many beneficial properties have been attributed to ginger including treatments for pain or muscles aches.22
Triterpenes: The medicinal use of triterpenes has been investigated by researchers, and their properties seem to include both antioxidant and anti-inflammatory.7 Some common medicinal plants containing triterpenes are Boswellia serrata, Ginseng root and rose-hip.
Cyclic triterpenes as Boswellia serrata also known as Salai or Sali guggul, is a moderately large branching tree belonging to the Burseraceae family, which thrives in dry mountainous regions of India, Northern Africa, and the Middle East. The gum resin extracted from the Boswellia species has been used in traditional Ayurvedic medicine in India for centuries as a remedy for the treatment of chronic inflammatory diseases.16 The resins contain monoterpenes (α-thujene), diterpenes (macrocyclic diterpenoids such as incensole, incensole oxide, iso-incensole oxide, a diterpene-alcohol serratol), and triterpenes such as α- and β-amyrins, pentacyclic triterpenic acids (boswellic acids), and tetracyclic triterpenic acids (tirucall-8, 24-dien-21-oic acids).24 Especially the pentacyclic triterpenoids 3-acetyl-11-keto-𝛽-boswellic acid (AKBBA), 11-keto-𝛽-boswellic acid (BBA) and 3-acetyl-𝛽-boswellic aid (ABBA) are interesting due to their anti-inflammatory properties.
Anti-inflammatory mechanisms of terpenes and terpenoids
Limonene and myrcene. The anti-inflammatory effects of D-limonene and myrcene has been studied to explore whether these monoterpenes could reduce/inhibit production of pro-inflammatory mediators. One study showed that at non-cytotoxic concentrations, myrcene and limonene inhibited IL-1-induced NO production.10 These monoterpenes also function as anti-osteoarthritis drugs, by having the ability to inhibit NF-κB activation. Myrcene showed to be more effective than limonene in preventing other inflammatory and catabolic responses in human chondrocytes, namely expression of iNOS, MMP-1 and MMP-13 induced by IL-1.10 Myrcene also prevented the increase in collagen I induced by IL-1. Collagen I is increased in OA and in association with chondrocyte dedifferentiation.10 Therefore, myrcene may be more effective in decreasing inflammatory and catabolic processes directly involved in cartilage destruction.10
α-pinene also seem to have different inhibiting functions. α -pinene, (+) α-pinene, (-) α-pinene have been tested for anti-inflammatory effects.10 (+) α-pinene demonstrated to be the most potent inhibitor of IL-1-stimulated inflammatory and catabolic pathways, mostly of NF-κB, and of inflammatory mediators such as iNOS and MMP-1 and -13. Furthermore, α-pinene proved to significantly reduce IkB-α degradation, which is an inhibitory protein, but when phosphorylated is part of the pathway that leads to NF-κB activation.25 Another study also showed that α-pinene could effectively reduce the production of IL-6 and TNF-α in rat macrophages.26
Boswellia serrata extract has been studied for its capability to decrease pain symptoms in OA patients. Boswellia serrata containing AKBBA seems to have inhibitory effects on 5-LOX.16 The effect is triggered by boswellic acids binding to the enzyme and is one of the key enzymes responsible for the synthesis of leukotrienes, which have been shown to promote cartilage degradation, by inducing MMP’s.16 An inhibition of 5-LOX is therefore sought after, to reduce OA pain symptoms.16
Bioavailability and processing of terpenes and terpenoids
The term bioavailability is used to “indicate the fraction of an orally administered dose that reaches the systemic circulation as intact drug, taking into account both absorption and local metabolic degradation”.27 Sensitive compounds like terpenes and terpenoids and phenolic compounds can be lost during processing or consumption due to factors such as heat, air, light, pH, water content, and natural enzyme systems.28 The impact of processing, storage, or cooking of terpenes and terpenoids is very limited and we only know that certain terpenoids (other than carotenoids) are unstable in chilled storage compared to room temperature and certain saponins are unstable in traditional cooking and in canning.28 It is therefore important to explore how external factors affect their bioavailability.27–30
As terpenes and terpenoids are abundant in nature and seem to offer potential anti-oxidative capacity, the focus of this review is to investigate the potential effects of terpenes and terpenoids on pain in the knee and/or hip in patients with osteoarthritis (OA). We must agree that up till now, there are only animal studies proving that terpenes and terpenoids alone, can work. But because studies in humans where terpenes and terpenoids are suggested to be an important part, have never been reviewed together and commented on, this was the topic of this review.
Literature search strategy
The systematic literature search was conducted using keywords related to the theme of this review and especially used for the first part to cover the relevance of the background and theoretical framework. Comprehensive searches were conducted with PubMed, and the “advanced” function was used to ensure the inclusion of a broad range of studies. Keywords were used as either free text words or Medical Subject Headings (MeSH) terms. These can be categorized into: Specific classifications of terpenes and terpenoids of interest, analgesic functions of terpenes and terpenoids in connection with OA in the knee and/or hip, plants/foods such as turmeric, ginger or boswellia, and terpenes vs. painkillers including NSAID’s (Table 1).
|
Terpenes and terpenoids of interest |
Analgesic/pain reducing functions in connection to OA in the knee and/or hip |
Plants/foods containing terpenes and terpenoids |
Terpenes vs. painkillers including NSAID’s |
|
MeSH terms: Terpen [MeSH] Terpenoids [MeSH] Medicinal terpenes [MeSH] |
Mesh terms: Osteoarthritis [MeSH] Inflammation [MeSH] |
MeSH terms: Terpene containing plants [MeSH] Nutraceuticals [MeSH] Natural remedies [MeSH] |
MeSH terms: Rescue medication [MeSH] NSAIDS’s [MeSH] Painkillers [MeSH] Side effects [MeSH] |
|
Free text words: |
Free text words: |
Free text words: |
Free text words: |
|
“Monoterpenes and terpenoids” |
“Anti-inflammatory” |
“Boswellia” “Ginger” “Turmeric” |
“Ibuprofen” “Paracetamol” |
|
“Diterpenes and terpenoids” “Triterpenes and terpenoids” “Labdane” |
“Inflammatory mediators” “Anti-inflammatory mediators” “Pain relievers” |
“Rosehip” “Shea nut oil” |
“Inhibition of inflammatory mediators” |
|
“Boswellic acid” |
“Chondrocytes” “Analgesic” |
Table 1 Used MeSH words and free text words as part of the systematic literature review and search for this review
Final study selection. After conducting a systematic literature search, 30 available studies were identified. To ensure the relevance and quality of the selected studies, we established inclusion and exclusion criteria that guided and focused our selection process. For details see Table 2. This methodology led to 10 usable papers as the remaining 20 papers did not meet our criteria.
|
Inclusion criteria |
Exclusion criteria |
|
- Experimental study. |
- Osteoarthritis in other body parts than knee and/or hip. |
|
- Osteoarthritis in the knee and/or hip. |
- Cannabis/cannabinoids. |
|
- Other treatments for OA, such as placebo or use of painkillers including NSAID’s. |
- In vitro. |
|
- Anti-inflammatory terpenes and terpenoids. |
|
|
- Human and animal in vivo studies. |
|
|
- Measurements of pain symptoms through WOMAC, VAS, LFI, and 6-minute walking test etc. |
|
|
- If inflammatory mediators were discussed in studies, relevant mediators were IL-1, 6- and 8-, MMP-1, -3 and -13, iNOS, COX-2, 5-LOX, and CRP (high sensitivity CRP (hs-CRP)). |
Table 2 Table overview of inclusion and exclusion criteria made to find relevant studies for analytical purposes
Evaluation of the papers
Among the included ten papers, four are human in vivo double-blinded, randomized, placebo-controlled clinical trials.23,31–33 One study by Karlapudi et al.,34 studies both humans and rats through in vivo double-blinded, randomized, placebo-controlled clinical trials. Two articles, Majeed et al.,16 and Stebbings et al.,35 are human in vivo pilot, randomized, double-blinded, placebo-controlled clinical trials. Another article is a human in vivo double-blinded, randomized-controlled clinical trial.36 A study by Farì et al.,37 is a human in vivo double-blinded prospective case-control study, while the tenth article, by Chen et al.,38 employs in vivo model studies with rats (Table 3).
|
Study |
Terpene/terpenoids in studies |
|
1. Winther et al.,23 |
Monoterpene:Pinene <5% Diterpenoids: <2% labdane and <0.3% alfa tocopherol Sesquiterpene: <8% dehydrocurdione, <6.5% curdione, <10% curzerenone Sesquiterpenoid:<7% curcomenone |
|
2. Chen and Wong,38 |
Triterpenoids: α-amyrin, 𝛽-amyrin, butyrospermol, lupeol(concentrations not given) |
|
3. Majeed et al.,16 |
Triterpenoids: <30% 3-acetyl-11-keto-𝛽-boswellic acid (AKBBA) 𝛽-boswellic acid (BBA), 11-ketoboswellic acid (KBBA) and 3‐acetyl‐β‐boswellic acid (ABBA) (concentrations not given) |
|
4. Farì et al.,37* |
Monoterpene:<2.84% 𝛽-myrcene Bicyclic sesquiterpene: <6.62% 𝛽-caryophyllene |
|
5. Sengupta et al.,32 |
Triterpenoid: <30% 3-acetyl-11-keto-𝛽-boswellic acid (AKBBA) |
|
6. Karimifar et al.,36* |
Triterpenoid: <60-70% 𝛽-boswellic acid (BBA) and <3% 11-ketoboswellic acid (KBBA) |
|
7.Karlapudi et al.,34* |
Triterpenoid:<0.6% 3-acetyl-11-keto-𝛽-boswellic acid (AKBBA) |
|
8. Winther et al.,31* |
Triterpenoids: Oleanolic acid, ursolic acid, and betulinic acid 1(concentration not given) Tetraterpene: All-trans-𝛽-carotene, All-trans-lycopene, cis-𝛽-carotene, and cis-lycopene (concentrations not given)2 |
|
9. Stebbings et al.,35 |
Sesquiterpenoid: Artemisinin (concentrations not given) |
|
10. Altman and Marcussen33 |
Tetraterpene: 𝛽-carotene (concentrations not given) |
Table 3 Overview of relevant terpenes and terpenoids studied in the selected analyzed articles
Green = terpenes, and blue = terpenoids
*Combination with phenolic compounds and/or other bioactive compounds.
Results regarding efficacy (in vivo human studies)
Regarding the outcome measure on WOMAC pain, stiffness, and physical function scores as a result of active treatment, seven out of nine human studies16,23,31–35 found statistically significant improvements in at least one of the three parameters. For further details see Figure 2, 3 and 4.
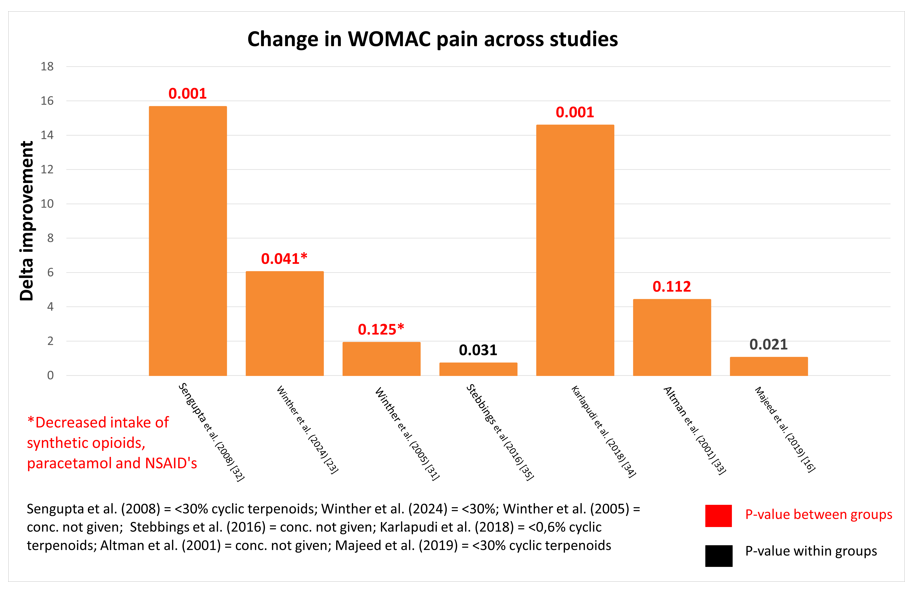
Figure 2 Change in WOMAC pain across studies.
WOMAC pain scores for seven included studies using terpenes. At the bottom is provided a description of contents in capsules in the different treatment groups, as well as definitions of p-values. *indicate a significant decline in the consumption of rescue medication over time.
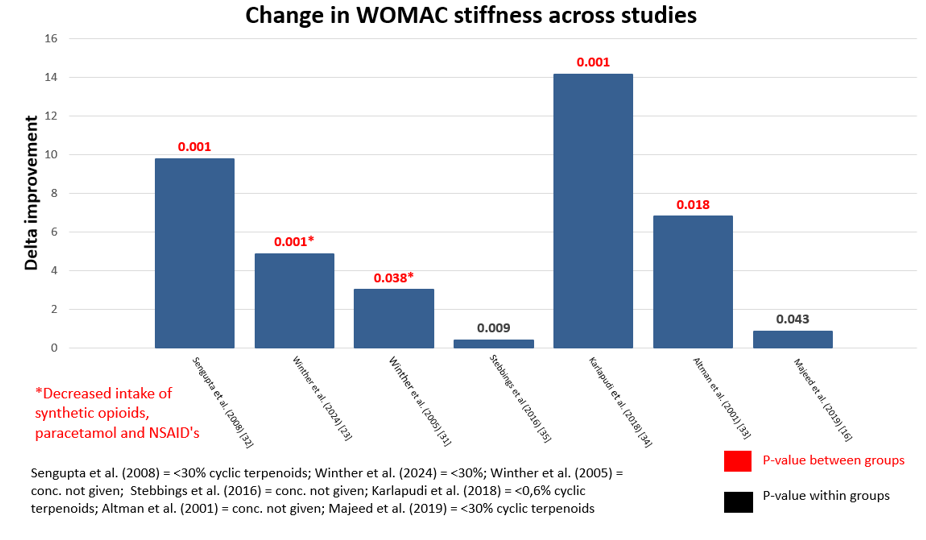
Figure 3 Change in WOMAC stiffness across studies.
WOMAC stiffness scores for seven included studies using terpenes. At the bottom is provided a description of contents in capsules in the different treatment groups, as well as definitions of p-values. *indicate a significant decline in the consumption of rescue medication over time.
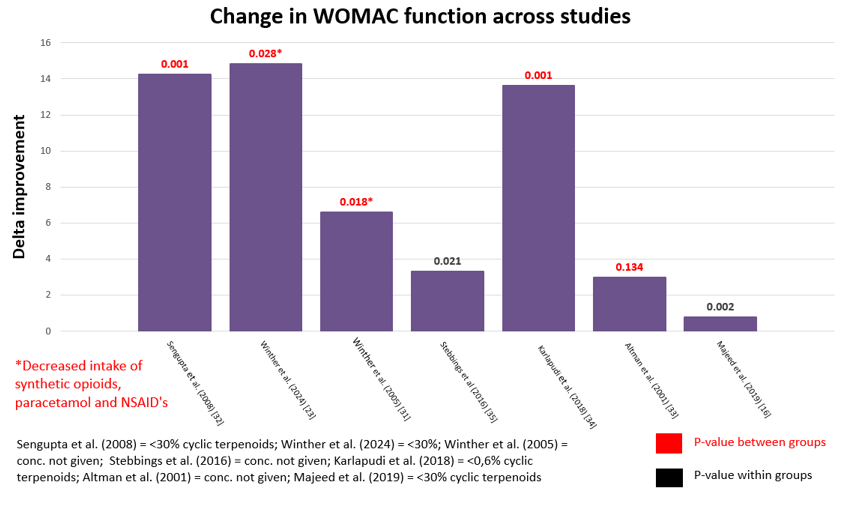
Figure 4 Change in WOMAC function across studies.
WOMAC function scores for seven included studies using terpenes. At the bottom is provided a description of contents in capsules in the different treatment groups, as well as definitions of p-values. *indicate a significant decline in the consumption of rescue medication over time.
Farì et al.,37 and Karimifar et al.,36 did not use the WOMAC outcome measures and one study was an animal study.
Six studies found that both VAS pain scores and/or Lequesne’s Functional Index (LFI) improved between groups as well,16,32–36 with exception to Stebbings et al.,35 who only found significant changes within groups, and Winther et al.,31 who only found significant results in the first three weeks of the study. However, in Winther`s study there was a significant decline in the consumption of rescue medication, such as paracetamol and synthetic opioids, when evaluated over a three month period. Details in study design and treatments is summarized in Table 4.
Consumption of rescue medication was followed in seven out of the ten studies. Winther et al.,23,31 found a statistically significant decline in the consumption of rescue medication as the result of active treatment. Karlapudi et al.,34 and Sengupta et al.,32 found that the placebo groups had either a higher intake or a higher request for rescue medication. Karimifar et al.,36 found no significant difference between groups, which showed that all interventions (terpene vs. ibuprofen) had equal effects on outcome measures. This may indicate that in that study terpene was equal to ibuprofen. And two studies, Farì et al.,37 and Altman and Marcussen33 found that there was no significant distribution among participants and their intake of rescue medication.
Results regarding safety
A modest increase in milder gastrointestinal side effects, as the result of treatment, was reported in one of the reported studies.33 In all the other studies side effects in placebo and active treatment groups were comparable. In all the studies mentioned above, vital signs such as heart rate and blood pressures was not altered by treatment.
In vivo – Animal studies
Chen and Wong38 found that the swelling of the OA induced knee joint was reduced and that degeneration of cartilage decreased in the active treatment group, while Karlapudi et al.,34 found that the paw oedema improved in the groups being actively treated. Both these findings indicate anti-inflammatory property.
The general trend is that in all nine human studies where extracts containing terpenes or terpenoids are a main part of treatment, there is some evidence that symptoms from osteoarthritis may decline as the result of treatment. And in two animal studies (one of the ten studies was testing animals as well as humans) there was anti-inflammatory capacity. There are, however, many precautions to be taken. Before a conclusion (if any) can be drawn, it is also important to focus on the study treatments, dosage, and duration of the studies along with which terpenes and terpenoids seem to be the most effective. In addition, in the studies reviewed other active ingredients than terpenes/terpenoids can have played a role.
Though the number of participants vary from around 30 to 247 people, in the clinical studies reviewed, the studies managed to find significant results from treatment and a very low level of side effects, suggesting that an intake of terpenes and/or terpenoids can improve symptoms of OA, including pain. Stebbings et al.,35 did not find significant improvements in WOMAC pain scores. The reasons for these results could be explained by the sample size, as it was estimated that 13 participants per group was needed to provide an 80% power. Subjects withdrew from the study before completion, resulting in groups ending up with only 9 and 11 participants. The results were therefore not so easy to interpret.
As mentioned in the analysis, Farì et al.,37 did not find significant distributions among patients in an intake of painkillers including NSAID’s. These results might be caused by the fact that they did not do at placebo-controlled trial but instead choose to do a prospective case-control study, creating limitations such as recall bias, as the subjects were to self-report, potentially leading to inaccuracies in data collection and outcome measures as participants may have difficulties in recalling past exposures or events.
The duration of the studies are also an important factor, as herbal remedies does not necessarily work “over night”.
The shortest study was by Karimifar et al.,36 lasted four weeks but still managed to find significant reduction in pain. In comparison, the longest study, made by Winther et al.,23 lasted six months, and tended to be more powerful as time went on. Explanations for finding similar results, despite the differences in duration, may be caused by the fact that Karimifar et al.,36 used a dose of the cyclic triterpenoid that was around 400 times higher than Winther et al.,23 who used a diterpenoid.
The varying concentrations used in the different studies can also affect the interpretation of the results. The lowest precise amount known was used by Winther et al.,23 who used capsules containing a minimum of 0.22 mg/capsule labdane. The highest amount used was by Majeed et al.,16 who used capsules containing 87.3 mg of total Boswellic acids. This would roughly result in a daily intake of a minimum of 39.6 mg of labdane for six months or 20.952 mg boswellic acids for four months, respectively. Both studies find significant pain management results, suggesting that the different terpenes and terpenoids may act differently, even at low or high doses. It would therefore be interesting to compare the different treatments at the same concentrations to determine which kind of terpene or terpenoids has the most effective outcome or if a combination would prove even more effective.
Most effective terpenes and terpenoids
As mentioned previously the studies comprise a variety of active terpenes and terpenoids. Every kind of terpene from mono- to tetraterpenes are researched. And on top of this, terpenes and again terpenoids are not the only active ingredients in the treatments. In many animal studies, treatment with terpene or terpenoids are used as monotherapy using high concentrations to determine the function. Such studies8,9,11,12 have provide further evidence to this review, as they show that terpenes and terpenoids alone have important effects on managing inflammation and pain in OA.
It turns out the most researched kinds of terpenes in the ten studies are the terpenoids. In fact, only Farì et al.,37 studied terpenes. Five out of the ten studies researched cyclic triterpenoids.16,32,34,36,38 This does not imply that these terpenoids are exclusively the most effective, as numerous of other studies explore various types of terpenes and terpenoids, but it can be assumed from the ten studies, that this type of triterpenoid might play an interesting role in pain management and is especially relevant for future studies. All the studies find results showing anti-inflammatory efficacies and analgesic properties of terpenes and terpenoids, however the knowledge about underlying mechanisms is still relatively limited. Different mechanisms have been mentioned in this review, such as inhibition of inflammatory mediators or the synthesis of anti-inflammatory cytokines.
Phenolic compounds and terpenes and terpenoids
Four out of the ten selected studies examined the use of a combination of bioactive compounds in pain relief and management of knee OA.33,34,36,37 Karlapudi et al.,34 found that their herbal formulation, containing both phenolic compounds and a triterpenoid extract from the Boswellia plants, had significant effects managing pain, improving physical function and joint discomfort, while Karimifar et al.,36 using boswellic acids and phenolic compounds from plant extracts, discovered that active treatment showed non-inferiority results compared to the ibuprofen group. Altman and Marcussen33 found that their purified ginger extract containing triterpenoid-like compounds such as gingerols, and 1-8-cineol, had a statistically significant effect on reducing symptoms in OA, while Farì et al.,37 using β-caryophyllene and myrcene also found improving results on pain management. However, it is uncertain whether the benefits are primarily due to synergistic interaction or if one class of compounds plays a more dominant role in these therapeutic effects.
Further research isolating each component is needed to fully understand their individual vs. combined impacts. With the support from the four studies, reviewed, it is suggested that combining phenolic compounds with terpenes or terpenoids could offer a potential medicinal alternative to painkillers including paracetamol and NSAID’s. This could reduce both side effects and pain in patients with OA.
Potential advantages of using terpenes instead of rescue medication
Painkillers including Paracetamol and NSAID’s are commonly used to treat symptoms in patients with OA in the knee and/or hip.2–6 NSAID`s exerts their therapeutic effects by inhibiting the enzyme COX-2 responsible for the production of prostaglandins. COX-2, induced by inflammatory cytokines, contribute to the pain and swelling associated with inflammation.39 NSAID’s have been linked to an increase in upper gastrointestinal complications, including bleeding and perforation amongst other.6 Due to these risks, a search for alternative bioactive compounds that can alleviate pain without causing serious side effects is well warranted.
Studies included in this review demonstrate that herbal remedies, with a certain amount of terpenes and terpenoids can reduce pain and also improve stiffness and daily activity in patients with knee and/or hip OA. Since terpenes and terpenoids are natural compounds, they are often perceived as more holistic and in harmony with the natural body process, which can be appealing to some patients seeking more alternative therapies. One of the most prominent advantages of terpenes and terpenoids are the lower risks of severe side effects and the fact that they might contribute to a healthier/safer option for long-term use, which is relevant for OA patients.
Further experimental research would be necessary to provide evidential data of efficacy and safety, directly comparing terpenes and terpenoids with established painkillers including paracetamol and NSAID’s. For regulatory approval, the use of these complex bioactive compounds must meet stringent and standardized safety and efficacy requirements, in order to create data for future purposes. Making specific extract through standardized methods, ensuring uniform quality and concentration of these active compounds, is essential.
Through a systematic literature review, ten studies all testing herbal remedies in which terpenes and/or terpenoids were an essential part, were analyzed. The results indicated a significant reduction in OA related symptoms including pain and stiffness and an improvement in physical function. In only one of the nine studies there were reports on milder uncomplicated side effects. The tenth study, an animal study, showed improved anti-inflammatory capacity. Possible underlying mechanisms for pain management were suggested to be caused by a reduction of pro-inflammatory cytokines such as IL-1, IL-6, and TNF-α and the inhibition of NF-κB and 5-LOX. Various types of terpenes and terpenoids, including mono-, di-, sesqui-, and triterpenes and terpenoids, have shown efficacy in pain management. It is important to state that from the present data it cannot be concluded that a specific classification of terpenes and terpenoids would be the more effective, as many other factors such as bioavailability or other bioactive compounds could play a role. In conclusion terpenes and terpenoids, offer a possible promising natural alternative for OA pain management, potentially reducing the intake of conventional painkillers having their associated side effects. However, more comprehensive studies are needed to validate these findings.
None.
Five out of ten studies declared no conflict of interest,23,31,35,37,38 while four studies does not comment on any form of conflict of interest.16,33,34,36 Sengupta et al.,32 was funded by Laila Impex R&D Center in India. Three of the authors were employees of this research center. The three authors of this paper have no conflicts of interest.
Kaj Winther was the supervisor for Caroline Krogh Agergaard and Christina Chinchay Nielsen who did all the practical work including the search for papers, creating the main text as well as tables and figures. Kaj Winther actively participated in writing the abstract, the discussion and conclusion strength and limitations.
There was no funding for writing this review.

©2025 Agergaard, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.