International Journal of
eISSN: 2381-1803


Research Article Volume 14 Issue 5
Department of Occupational Therapist, Pará State University (UEPA), Brazil
Correspondence: Karoline Vitória Silva Rodrigues, Faculty of Physiotherapy and Occupational Therapy (FFTO) - Federal University of Pará, Rua Augusto Corrêa, Gate 4, Cidade Universitária José Silveira Neto, Sector Saúde - Guamá, 66075-110, Belém, Pará, Brazil
Received: July 30, 2020 | Published: October 11, 2021
Citation: Rodrigues KVS, Castro YSG, Najjar ECA. Adherence to the treatment and occupational routine of patients with arterial hypertension care in a basic health unit in belém - pará. Int J Complement Alt Med. 2021;14(5):210-215. DOI: 10.15406/ijcam.2021.14.00563
Introduction: It is estimated that adherence to the treatment of Systemic Arterial Hypertension worldwide is around 8% to 50%. The occupational therapist seeks to analyze the subject's occupational routine in order to favor the adaptation to the changes necessary for the proper maintenance of health treatment.
Objective: To identify treatment adherence and the occupational routine reported by individuals with Systemic Arterial Hypertension treated at a Basic Health Unit - Belém Pará.
Method: This is a descriptive, cross-sectional study with a quantitative and qualitative approach, carried out with 47 hypertensive individuals registered in the HIPERDIA program. Identification data, cardiovascular risk factors, treatment adherence and occupational routine were collected.
Results/discussion: All individuals had at least one cardiovascular risk factor. The levels of treatment adherence were found to be medium (42.5%) and high (44.7%). However, most of them reported difficulties in adhering to care related to food (66%), physical activity (61.7%) and stress control (59.6%). Regarding the occupational routine, 72.3% reported not feeling overwhelmed with activities and 53.2% reported that the routine interferes with adherence to health care.
Conclusion: The study encourages discussion about the conditioning relationship between adherence to the treatment of a chronic disease and occupational routine. It points to the need to develop occupational therapeutic programs with individuals with chronic diseases and the importance of the occupational therapist in the Primary Health Care team.
Keywords: hypertension, patient cooperation, occupational therapy
CNCD, chronic non-communicable diseases; CVD, cardiovascular diseases; SAH, systemic arterial hypertension; DBP, diastolic blood pressure; PHC, primary health care; AMI, acute myocardial infarction; BMI, body mass index
Chronic non-communicable diseases (CNCD) are currently considered a serious public health problem. They cause changes in the mortality profile of the population, as they are responsible for more than half of the deaths worldwide. The main CNCD are Cardiovascular Diseases (CVD), cancers, chronic respiratory diseases and diabetes mellitus, characterized by their non-infectious origin, prolonged course, association with functional disabilities and various risk factors.1
According to the Pan American Health Organization,2 it is estimated that about 41 million deaths annually are caused by CNCD, and that these diseases currently represent a threat to the health and development of all nations. In Brazil, in 2015, 51.6% of the mortality of the population aged 30 to 69 years was due to CNCD.¹ In this context, Systemic Arterial Hypertension (SAH) is a serious public health problem, characterized mainly by its high prevalence and low rate of control. In 2013, the prevalence of self-reported SAH in the Brazilian population was 24.3%, affecting 60.9% of individuals aged 65 and over.3
According to the Brazilian Society of Cardiology,4 SAH is defined by systolic blood pressure (SBP) greater or equal to 140mmHg and diastolic blood pressure (DBP) greater or equal to 90 mmHg in individuals who do not use antihypertensive medication. However, for accurate diagnosis, in addition to blood pressure levels, some factors must be considered, such as the global cardiovascular risk estimated by the presence of risk factors, the presence of lesions in the target organs and the associated comorbidities.
Regarding the risk factors for SAH, age stands out, with prevalence in the elderly; sex and ethnicity, with prevalence in women and black people; overweight and obesity; salt intake; alcohol intake; sedentary lifestyle; socioeconomic factors, in which there is a higher prevalence of the disease in individuals with less education; and genetics.4
Despite its high prevalence, studies show that the adequate treatment of SAH promotes the control of blood pressure levels and the reduction of complications in a few years, being able to be mediated medically, through its control and healthy lifestyle habits. The treatment consists of drugs and dietary and behavioral care, which seek to provide the maintenance and control of the disease, as well as the prevention of its complications.3
In 2001, the Ministry of Health proposed a Plan for the Reorganization of Attention to Systemic Arterial Hypertension and Diabetes Mellitus, carried out through the HIPERDIA programmatic care model (Registration and Monitoring System for Hypertensive and Diabetics), enabling actions for continuous and high capillarity.5 This proposal aims to offer care beyond the binomial complaint-conduct, encompassing the identification of asymptomatic people, monitoring the treatment and establishing links between the health team-patients-caregivers, as well as using health education strategies, incorporating the social reality of the patient to this process.5
However, despite its importance and need, it is estimated that adherence to the treatment of hypertensive patients worldwide is around 8 to 50%, representing a challenge for the health team.6 The multiprofessional team, an essential part for the conduction and effectiveness of the HIPERDIA program, must direct its efforts towards the promotion of the adherence to the treatment and prevention of complications, focusing on the evidence that define the necessary care for the control of blood pressure and blood glucose levels, through drug treatment and lifestyle changes.7
Neglecting the treatment of SAH can have harmful consequences for the subject, given that it is an important risk factor for several other pathologies. Among these, diseases arising from atherosclerosis and thrombosis stand out, which are predominantly manifested by cardiac, cerebral, renal and peripheral vascular involvement.The American Heart Association - AHA8 points out that SAH was present in 69% of American individuals who had the first episode of Acute Myocardial Infarction (AMI) and in 77% of individuals who had a Stroke.
For the treatment of SAH to be properly carried out, the Brazilian Society of Cardiology4 emphasizes the importance of a multiprofessional team monitoring the patients with SAH, which can consist of all professionals who work in Primary Health Care (PHC) and deal with with hypertensive patients, as this is a multifactorial clinical syndrome, with several repercussions on the subject's life.
The importance of a multiprofessional team working in this sphere is evidenced, contributing not only to the medication and non-medication treatment of hypertension, but also motivating and making aware the hypertensive patients about the need for adequate maintenance of their care and the importance of self-care. Thus, it encourages the expansion of responsibilities regarding decisions about their health.9
The American Occupation Therapy Association - AOTA10 recommends that the occupational therapist, together with individuals with chronic illness, should seek to analyze their occupational routine in order to promote awareness and adaptation about the necessary changes for the promotion and proper maintenance of the treatment. He considers that occupational therapy interventions may enable better responses in the health situation, due to the expertise of these professionals who can modify harmful lifestyle habits, focusing their actions on the development of appropriate habits and a routine that contributes to the development of treatment.
AOTA10 points to a close relationship between the treatment of a chronic disease with an occupational routine, emphasizing that the man's routine can influence positively or negatively in the practice of health care. The Association highlights the role of Occupational Therapy with CNCD, emphasizing that these professionals are specialized in the prevention and modification of lifestyle, focusing their actions on the proper development of treatment. The Occupational Therapy professional, in this way, encourages the self-responsibility of people with chronic illness, to become protagonists in the management of their treatment.
Therefore, in the context of the discussion, the objective of this study is to identify treatment adherence and the occupational routine reported by individuals with Systemic Arterial Hypertension treated at a Basic Health Unit - Belém Pará.
This is a descriptive, cross-sectional study with a quantitative and qualitative approach. It consists of a section of the project financed by PIBIC Cnpq, approved by the Research Ethics Committee (CEP) of the State University of Pará (UEPA), CCBS Campus II, opinion number 099536/2014, in November 2014.
Two questionnaires with semi-structured questions were used as a data collection instrument. The first questionnaire sought to collect participants' identification data and cardiovascular risk factors, such as blood pressure levels, the presence of Diabetes Mellitus, Body Mass Index (BMI), cholesterol and triglyceride levels.
The second instrument, with 12 semi-structured questions, aimed to evaluate two dimensions: Adherence to treatment (food care, physical activity, proper use of medication, alcohol consumption, tobacco consumption and experiencing stressful situations) and Occupational Routine (work, domestic activities, leisure, interpersonal relationships, overload of daily activities and perception about the relationship between treatment and occupational routine). The instruments were initially tested with 10 users that were not participating in the study, in order to be evaluated. After this procedure, they were submitted to changes.
For the analysis of risk factors and attributes related to the Adhesion of Hypertension, the 7th Brazilian Guideline for Hypertension (2016) was used as a theoretical reference.
Data collection was carried out over a period of two months, from the approach and invitation of patients treated by the HIPERDIA program of a Basic Health Unit in Belém - Pará. 47 individuals participated in the research. Data collection was carried out individually in an office, lasting approximately 30minutes for each participant.
As inclusion criteria for participation in the study, the following information were used: being 18years of age or older, being literate, having Systemic Arterial Hypertension and being enrolled in the HIPERDIA program of the Basic Health Unit. Patients with impairment were excluded from the study regarding cognitive, with previous neurological disorders (such as stroke, brain trauma), as a result of these pathologies interfering in the responses to the questionnaires performed.
Quantitative variables were presented by distributions of absolute and relative frequencies.The analysis of the questionnaire data resulted in a score for the analyzed aspect - Adherence to Treatment. To assign the score, the answers were converted to a scale whose score ranged from 0 (zero) to 6 (six) points. The score of Zero meant the worst evaluation and the score of Six corresponded to the best possible evaluation. Results from 0% to 39.9% were classified at low levels, from 40% to 69.9% were classified at medium levels, and results from 70% to 100% were classified at high levels, according to the classification used in the study de Mazzuchello et al.11
Qualitative data were collected through the participants' reports, in which they were recorded in a field diary and analyzed according to the content analysis method. This consists of using systematic and objective procedures that analyze the material step by step in order to categorize the verbal behavior of the participants.12
The results were subdivided into categories: (1) Adherence to Treatment, which aimed to identify the development or not of food care, physical activity, stress control, correct use of antihypertensive medication and consumption of alcoholism and smoking; and (2) Occupational Routine, which sought to identify the occupational routine reported by the participants and their perception about its relationship with the treatment of SAH.
To identify the participants, we chose to use the letter P followed by a number, for example P1, P2, up to P47.
Of the 47 survey participants, 76,6% are female and 76,6% are between 56 and 75 years old. Approximately 36,2% said they had completed high school and 70,2% reported having a monthly income between 1 and 2 minimum wages, as shown in Table 1.
|
Description |
N |
% |
|
Age Range |
|
|
|
35 to 55 years |
5 |
10.6% |
|
56 to 75 years |
36 |
76.6% |
|
76 to 90 years |
6 |
12.8% |
|
Fri |
|
|
|
Male |
11 |
23.4 |
|
Feminine |
36 |
76.6 |
|
Race / color |
|
|
|
Brown |
28 |
59.6 |
|
Black |
5 |
10.6 |
|
White |
10 |
21.3 |
|
Other |
4 |
8.5 |
|
Schooling |
|
|
|
Literate |
11 |
23.4 |
|
Fundamental |
14 |
29.8 |
|
Medium |
17 |
36.2 |
|
Higher |
5 |
10.6 |
|
Family Income |
|
|
|
Without Income |
2 |
4.3 |
|
1 to 2 Minimun Wage |
33 |
70.2 |
|
3 to 5 Minimun Wage |
11 |
23.4 |
|
6 MW or more |
1 |
2.1 |
Table 1 Sociodemographic profile of the 47 participants. Belém - PA, year 2014
Source: Field research
|
Risk Factors |
N |
% |
|
Blood Pressure Levels |
|
|
|
Normal |
33 |
70.3 |
|
Changed |
14 |
29.7 |
|
Diabetes Mellitus |
|
|
|
Absent |
29 |
61.7 |
|
Gift |
18 |
38.3 |
|
BMI |
|
|
|
Normal Weight |
24 |
51.1 |
|
Overweight or Obesity |
23 |
48.9 |
|
Cholesterol |
|
|
|
Normal |
26 |
55.3 |
|
Changed |
21 |
44.7 |
|
Triglycerides |
|
|
|
Normal |
24 |
51.1 |
|
Changed |
23 |
48.9 |
Table 2 Cardiovascular risk factors of the 47 participants. Belém - PA, year 2014
Source: Field Research
Regarding the sociodemographic profile of the participants, two aspects stood out: gender and age group. Most participants were aged between 56 and 75years. Some studies have shown that blood pressure levels tend to increase with age, considering values greater than or equal to 14/9, with the prevalence of SAH above 60% in the age group above 60 years of age, as observed in the present study.4
Regarding gender, the predominant was female. The study by Silva, Araújo and Campos,13 in the analysis of 50 medical records of individuals registered in the HIPERDIA program, identified that 64% were female and 66% were between 61 and 80 years old, corroborating the findings of the present study.
In the analysis of cardiovascular risk factors, it was identified that 29,7% of the individuals had altered blood pressure levels, 38,3% had diabetes mellitus, 48,9% of the individuals had overweight and obesity (from 25 to 38.7 BMI), 44.7% had high cholesterol levels and 48,9% high triglyceride levels, according to Table 2.
It was observed that all individuals in the research had at least one risk factor. In the study by Radovanovic et al.14 with hypertensive patients, the authors found similar results, in which all participants aged 50 and over had at least one cardiovascular risk factor and of these, 40% had five or more risk factors.
Regarding BMI, cholesterol and triglycerides, it was found that about 40% of the study participants showed changes. In analysis, the biggest difficulties reported were the food care and physical activity, which considerably impact in weight loss and body fat. Panatto et al.15 emphasize that combining intervention strategies aimed at the practice of physical activity and nutritional monitoring impacts have better results in the reduction of abdominal circumference and weight / BMI - Body Mass Index.
Concerning blood pressure levels, most participants had controlled levels. It is noteworthy that the controlled blood pressure levels may be associated with the fact that approximately 66% of the participants stated that they use the antihypertensive medication correctly and only 19,14% and 4,2%, respectively, report consuming alcohol and tobacco. Cesarino et al.16 show similar results in their studies, where the average number of hypertensive patients with controlled pressure was higher than those who were unable to control their blood pressure levels.
In addition, for the aforementioned authors, factors such as treatment time, satisfaction with the medication, understanding of medical instructions, availability of the medication at the unit's pharmacy and others can contribute to adherence to drug therapy and, consequently, to control blood pressure (PAN). It is noteworthy, therefore, that the vast majority of participants in the present study have more than 10years of diagnosis and receive all medications used in the Health Unit in where they are registered.
Adherence to the treatment
From the quantitative analysis of the aspect in question, the levels of Adherence to the Treatment of SAH were identified, shown in Figure 1.
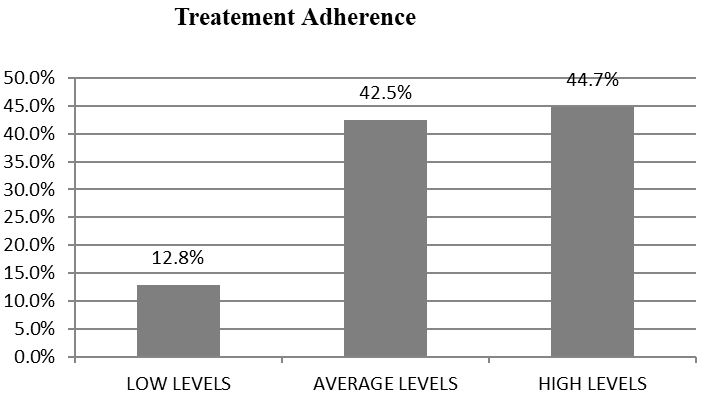
Figure 1 Levels of Adherence to Treatment of the 47 participants. Belém - PA, 2014.
Source: Field Research.
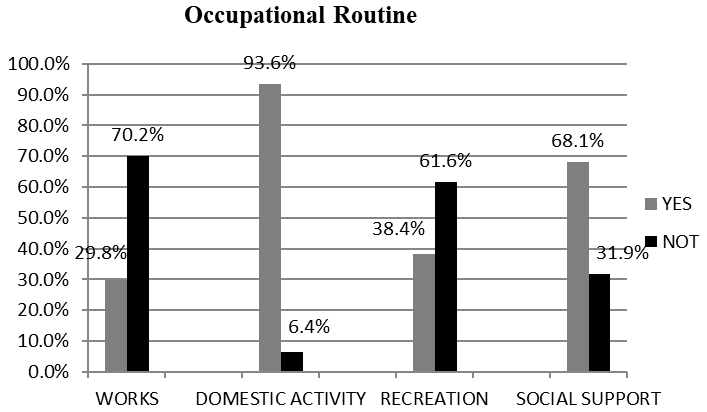
Figure 2 Work, domestic activities, leisure and interpersonal relationships of the 47 participants. Belém - PA, 2014.
Source: Field Research.
The graph points out that the levels of Treatment Adherence, according to the participants' reports, are between medium (42,5%) and high (44,7%). Standing out the care that contributed to such results, the use of antihypertensive medication developed in an appropriate and precise manner by 65,9% of the cases and the reduced consumption of alcohol and tobacco use by only 19,14% and 4,2% of participants, respectively.
These findings corroborate the study conducted by Bezerra, Lopes and Barros17 who observed a sample of 77 individuals and found that 87% were adherent to drug therapy. Likewise, Gewehr et al.18 point out that 66,2% of the participants in their study reported high adherence to treatment, with a mean age of individuals older than 64 years and with a longer time of diagnosis, compared to non-adherents.
In a qualitative analysis, it was identified that, unanimously, all participants demonstrated knowledge about the importance and necessity of using the medication and that, most of them, according to their reports, maintained the care with its use in the day-to-day. to day:
“Ah doctor, this is a care I have for sure. I do it at the right time, every day. My medicine cannot be missing.”(P 43).
“The greatest care is medication, right? You have to do it, otherwise my pressure willgo up there. It is treacherous.”(P 39).
However, it was observed that some aspects did not present such significant levels, and contributed to the impossibility of a higher score in the item Adherence to Treatment. These were characterized by food care, such as the restriction in the use of salt, fried foods and fats, in which 66% of the participants reported having difficulties; physical activity, which was not developed 61,7% of the participants; and the experience of stressful situations, reported by 59,6% of the participants.
Most of the participants reported difficulties in following the care related to food and physical activity due to the absence of these habits throughout their lives, as shown:
“It is not easy to stop eating everything I have always liked, doctor. A little bacon, a very greasy meat, my sweets... Ah! There is no way to resist sometimes.”(P 4).
“I'm not going to lie to you... I don't have that much care with food. It is difficult to stop eating what I like. Eating is the greatest pleasure in life (laughs).”(P 44).
“Oh, these exercises are a problem... I can't get out of my house. I never did, right?” (P 18).
Lindemann, Oliveira and Mendonza-Sassi19 highlight the difficulty of primary care users in achieving changes in dietary patterns. In their study of 1,264 primary care users, 31,1% reported difficulties in developing a healthy diet. Of these, 57,6% attributed the high costs of this food pattern as a reason, 49,4% pointed to the lack of desire, 41,6% highlighted the lack of interest in giving up foods considered pleasurable, 35,7% reported the lack of time, and 31,3% reported ignorance.
In the study by Mazzuchello et al.11 of the 102 participants evaluated, only 20,6% reported physical exercise at least three times a week. In a sample of 14,521 hypertensive, diabetic and / or dyslipidemic patients, only 15,1%, 13,9% and 17,8% reported adherence to the practice of physical activity, respectively, with men being more susceptible to being more active than women women.20
López-Benavente et al.21 point out that the high rates of physical inactivity in the general population are correlated to the contemporary lifestyle, characterized by the intense overload of daily activities. They report that the lack of this habit throughout life contributes to the unwillingness to start maintaining a physically active life, and that women over 65 years of age have greater difficulty in adhering to physical exercise, corroborating the findings of the present study, which showed a female prevalence in non-adherence to this care.
Regarding stress control, Aragão et al.22 evaluated the possible reasons that interfere in maintaining this care for the treatment of hypertensive and/or diabetic individuals. The results pointed to social and economic peculiarities as frequent reasons for experiencing stressful situations, indicating borderline affective support in their statistical significance and low income, corroborating for the present study, which identified economic difficulty as the most reported reason for situations experienced stressors.
Occupational routine
In respect of the Occupational Routine of the participants, the graph below shows the results related to work activities, domestic activities, leisure and interpersonal relationships:
In Domestic Activity, 70,2% of participants stated that they perform all domestic activities, which includes tidying up the house; sweep the house; wash the dishes; make food; wash clothes. In turn, 23,4% of the participants stated that they performed at least one of the activities mentioned above and only 6,4% of the patients reported that they did not perform any domestic activities.
In the item Labor, 70,2% of the individuals stated that they did not carry out paid work, but considered domestic activities as work. 82,9% of the participants indicated that they do not consider work as a source of stress and 89,3% classify this activity as pleasant (including domestic activities, for those who considered it as work).
Regarding leisure, 61,6% of them reported not doing any leisure activities. As for interpersonal relationships and social support outside the family, 68,1% reported receiving some type of support from friends or close people and 74,5% stated that they had not frequent conflicts in their family structure.
Among the factors related to experiencing stressful situations, study participants pointed to low income as the main reason, followed by the presence of family conflicts.
In the assessment of support networks, under the perception of people with diabetes and hypertension, the findings found fragile family networks and the presence of conflicts among study participants; in addition to economic difficulties and low income, corroborating the research results.22 Weak family structures, with the presence of constant conflicts, and low family income, are considered as important risk factors for experiencing stressful situations, which in turn, have a significant impact on health and the maintenance of CNCD.23
Regarding the participants' perception of the presence of overload of activities performed in the occupational routine, 72.3% stated that they did not feel overwhelmed in their daily activities. This fact may have contributed to the good results of treatment adherence presented.
In turn, in the study by Rodrigues,24 the individuals who had the highest activity overload were those who had the lowest levels of treatment adherence. Overload contributed mainly to forgetting the use of medication.
Individuals with CNCD, whatever they may be, need to assume a new routine, which includes habits that revolve around a new occupational role assumed by the individual, the role of patient. Thus, the new occupational role assumed brings with it the need to change habits, in order to promote better responses to treatment.25 In this context, Rodrigues24 points out that the overload of activities is one of the factors of the occupational routine that can negatively interfere in adherence to the treatment of chronic disease.
Participants who considered themselves overloaded with activities during their occupational routine, reported an excess of domestic activities, followed by activities of care for third parties (role of caregiver, grandchildren mainly), as observed:
“I have a lot to do at home, doctor, when I see it is already too late to go out for a walk (...)” (P35).
“I wake up early to drop him (the grandson) at school. Then I already have things at home to do, there is no time (to perform physical activity).” (P42).
Sousa et al26 highlight that active aging among the elderly is characterized by intense participation in various daily activities, which are of a physical, social, intellectual and work nature. Elderly women, in particular, assume important roles for the family configuration, with emphasis on the responsibility of domestic activities and care for third parties, especially grandchildren, which can imply overload and illness.27
Regarding the perception of the relationship between the occupational routine and adherence to the treatment of SAH, 53.2% of the participants reported that the routine interferes with the adherence to health care, which may harm or contribute to their maintenance.
Houtum, Rijken and Groenewegen28 emphasize the intimate relationship between daily life and the management of a chronic disease. The authors understand that in the same way that chronic disease interferes with the maintenance of daily activities, the occupational routine also influences, positively or negatively, the management of the disease and adherence to the necessary care for its treatment. Thus, these individuals need adequate professional support to achieve a balance in the process of becoming ill and living.
Rodrigues24 observed that the occupational therapeutic monitoring of hypertensive and / or diabetic individuals enabled a greater individual perception about the relationship between occupational routine and life habits, promoting change in health care and greater adherence to the treatment of chronic disease. With the diagnosis of SAH, it is expected that the routine of hypertensive patients will undergo some modifications and habituations for better development of care related to treatment.
In this sense, the competences of the occupational therapist in promoting and sensitizing individuals to adopt healthy habits and in favoring the maintenance of health are emphasized, through the construction or reorganization of an occupational routine that contributes to the treatment and prevents progression or complications of diseases or disabilities, considering, therefore, occupations as determinants of the health process.29
The research pointed to the presence of at least one cardiovascular risk factor among the participants, highlighting overweight /obesity and dyslipidemia as the most frequent, becoming an alert for the managers and local health professionals, due to the severity of pathology and the high prevalence of possible health complications.
Regarding treatment adherence, it was identified that the participants demonstrated medium and high levels of adherence, showing good adherence to drug therapy and low consumption of alcohol and tobacco. However, the difficulties reported regarding food care, physical activity and stress control are evident.
Concerning the analysis of the occupational routine, it was identified that financial difficulties and the presence of family conflicts were correlated with the experience of stressful situations. It was highlighted that the excess of domestic activities and care with third parties were the most performed activities during the routine and that contributed to the overload of some participants. In addition, it was observed that the report of the absence of overload of activities by most of the participants may have contributed to the good results of treatment adherence.
The study corroborates and emphasizes, in the context of Occupational Therapy, the conditioning relationship between occupational routine and health care, pointing to the need for the development of long-term occupational therapeutic programs, aimed at analysis, intervention, adaptation, reorganization and / or modification of the occupational routine of the person with chronic illness.
Therefore, the importance of the role of the occupational therapist in the PHC team is highlighted, especially with the HIPERDIA program, as a professional working in the prevention and promotion of health, with performance based on the understanding of the health-disease processes, considering the territorial conditions , social, biological and psychological factors related to occupational aspects. It also points out the performanceof this professional in understanding the importance of the subject's participation in their care process.
None.
The authors declare that they have no conflicts of interest related to the material of this manuscript.
The authors declare that they have no financial interests related to the material of this manuscript.

©2021 Rodrigues, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.