eISSN: 2576-4497


Case Report Volume 8 Issue 3
Otorhinolaryngologist, Plastic Surgery, Santa Paula Medical Group, Venezuela
Correspondence: Casas Ocando Julio, Otorhinolaryngologist, Plastic Surgery, Santa Paula Medical Group, Caracas, Venezuela, Tel +1 7864633750
Received: August 15, 2025 | Published: August 28, 2025
Citation: Julio CO. Ethmoid polyposis in a pediatric patient: a case report. Hos Pal Med Int Jnl. 2025;8(3):54-55. DOI: 10.15406/hpmij.2025.08.00272
Nasal polyps are benign growths of the sinonasal mucosa. Their incidence is low in the pediatric population (<1%), and they often serve as a clinical marker for underlying systemic conditions, such as cystic fibrosis, primary ciliary dyskinesia, and allergic or chronic inflammatory diseases. Ethmoid polyposis is particularly uncommon in young children and demands a thorough diagnostic investigation. We report the case of a 6-year-old female patient with pansinusitis and a complication of preseptal cellulitis. During a Functional Endoscopic Sinus Surgery, polyps were unexpectedly discovered and removed from the right ethmoid sinus. Histopathological analysis confirmed the diagnosis of ethmoid polyposis. This finding, rare for her age, highlights the crucial link between chronic rhinosinusitis and allergic rhinitis in the pathogenesis of pediatric polyps. The patient showed excellent recovery, and a 24-month follow-up confirmed no recurrence, demonstrating the efficacy of combined surgical and long-term medical management. This case underscores the importance of a high index of suspicion for polyposis in pediatric patients with severe or refractory rhinosinusitis.
Keywords: pediatric nasal polyps, chronic rhinosinusitis, ethmoidal polyps, fess, allergic rhinitis
Nasal polyps are benign, inflammatory lesions of the sinonasal mucosa, defined by a significant infiltration of inflammatory cells, including eosinophils. While the precise etiology remains unclear, in children under 10 years of age, their presence often indicates underlying comorbidities. These include cystic fibrosis (CF), which is present in up to 86% of affected children, along with primary ciliary dyskinesia, chronic rhinosinusitis (CRS), and allergic rhinitis (AR).1,2 The synergistic relationship between CRS and AR is particularly relevant, as it creates a persistent inflammatory environment that fosters polyp development and complicates long-term management.3,4 The discovery of ethmoid polyps in a young child is a rare clinical event. This report details the case of a 6-year-old female patient whose ethmoid polyposis was found incidentally during surgery for a sinus infection complication. We emphasize the clinical importance of this finding and the success of a combined surgical and medical treatment approach.
A 6-year-old female presented to the emergency department with a 72-hour history of fever and swelling of the right eyelid. Previous outpatient antibiotic treatment had failed (amoxicillin and ceftriaxone). Physical examination revealed periorbital erythema and edema, without any restriction of extraocular movements. Nasal endoscopy showed significant turbinate enlargement (inferior and middle) and purulent discharge from the right middle meatus. Laboratory results indicated a high white blood cell count (18.0 K/mm³) with a neutrophilic predominance (82%). The patient was admitted for intravenous antibiotics (meropenem, vancomycin) and steroid therapy. A CT scan of the paranasal sinuses revealed opacification of the frontal, ethmoid, and maxillary sinuses, with sphenoid mucosal inflammation. There was also obstruction of the osteomeatal complex, hypertrophy of the inferior and medial turbinates, and enlargement of the adenoids (Figure 1); there were no signs of intracranial extension. Based on these findings, a diagnosis of pansinusitis complicated by preseptal cellulitis was established.
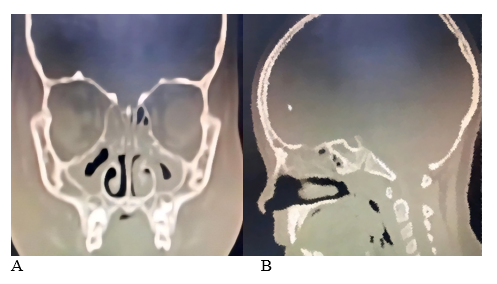
Figure 1 CT scans (A; coronal, B; sagittal) show increased opacity in the frontal, ethmoid, maxillary, and sphenoid regions, along with blockage of the osteomeatal complex and enlargement of the adenoid.
After 72 hours, the periorbital inflammation improved, and the patient underwent FESS under general anesthesia. During the procedure, a bilateral antrostomy and ethmoidectomy were performed. Mild purulent material was drained from the right anterior ethmoid sinus. Unexpectedly, several polyps were identified and removed endoscopically from the roof of the right ethmoid cavity (Figure 2). The excised polypoid tissue was submitted for histopathological examination. Hemostasis was verified, and intranasal irrigation was performed; bacitracin was applied instead of anterior nasal packing to optimize patient comfort and recovery. The histopathological report describes fragments of a polypoid lesion lined with respiratory epithelium. The subepithelial stroma is loose and edematous, containing an inflammatory infiltrate composed of lymphocytes, plasma cells, eosinophils, neutrophils, and mast cells (Figure 3). The final diagnosis was ethmoid polyposis associated with chronic rhinosinusitis and allergic rhinitis, resulting in a satisfactory postoperative outcome and symptom improvement within the first week. Postoperatively, the patient was managed with nasal saline rinses, intranasal corticosteroids, and oral antihistamines. She was discharged with significant symptom improvement. She remains symptom-free at 24 months.
The discovery of ethmoid polyps in a young child presenting with an acute complication like preseptal cellulitis is a rare but significant finding. This case highlights the intricate link between chronic rhinosinusitis, allergic rhinitis, and the development of nasal polyps in the pediatric population.4 Unlike in adults, pediatric nasal polyposis is a distinct entity often linked to a more complex inflammatory profile. Our patient's successful outcome demonstrates that, even in cases of rare presentation, a combined therapeutic approach is highly effective. While medical management is the initial approach for most pediatric rhinosinusitis cases, surgical intervention via FESS was essential here to resolve the acute complication and remove the underlying polyps. Furthermore, our findings support the consideration of adenoidectomy as an initial step in children under seven years of age with persistent CRS. Long-term observational studies have demonstrated that adenoid hypertrophy can act as a chronic inflammatory reservoir, and its removal can improve CRS outcomes, thus reducing the likelihood of polyp recurrence.5 This observation represents a crucial component of a holistic treatment strategy. The lack of recurrence over 24 months underscores the importance of a comprehensive strategy that includes both surgical debulking and long-term medical management of the inflammatory triggers (e.g., allergic rhinitis).6,7 This case highlights the long-term effectiveness of this combined approach for rare patient profiles.
Ethmoid polyps are an uncommon finding in children under 10 years of age and may signal an underlying systemic pathology. This case demonstrates that these polyps can be an incidental finding during surgery for severe chronic rhinosinusitis. The excellent long-term outcome in our patient validates the effectiveness of a multidisciplinary approach, combining FESS for surgical debridement and adenoidectomy when indicated, with sustained medical management of associated inflammatory conditions. This strategy can lead to durable symptom improvement and prevent polyp recurrence, ultimately enhancing the patient's quality of life.
None.
The author declared that there are no conflicts of interest.

©2025 Julio. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.