eISSN: 2576-4497


Case Report Volume 8 Issue 2
Prince of Asturias University Hospital, Madrid, Spain
Correspondence: Ana Isabel Cillero, Prince of Asturias University Hospital, Madrid, Spain, Tel +34 626465577
Received: May 02, 2025 | Published: May 16, 2025
Citation: Cillero AI. Application of portable topical oxygen therapy: a case report. Hos Pal Med Int Jnl. 2025;8(2):26-29. DOI: 10.15406/hpmij.2025.08.00267
Diabetic foot ulcers often have difficulty healing due to low tissue oxygenation, which affects their regenerative capacity. Topical oxygen therapy is a novel tool for wound treatment in patients with diabetic foot because it promotes wound healing by increasing angiogenesis, fibroblast activity, and collagen synthesis.
The objective: It is to describe the evolution of a dehiscent wound in a diabetic patient.
Methodology: A clinical case describes the approach to treatment and the application of the continuous transdermal oxygen therapy device.
Results: In five weeks we have achieved a reduction in the size of the lesion and its re-epithelialization.
Conclusions: The supplemental oxygen provided with this therapy has helped us increase angiogenesis, accelerating wound perfusion, epithelialization, and wound closure.
Keywords: continuous transdermal oxygen therapy, oxygen, diabetic foot, wound healing, wound care, vascular ulcers, hypoxia, infection, diabetic foot ulcer, pain, non-healing wound, wound size
Diabetic foot ulcers are one of the most common and serious complications of diabetes mellitus.1 It can be stated that between 40 and 70% of lower limb amputations occur in diabetic patients.2,3 Oxygen is essential for the healing of these wounds. Its absence, or hypoxia, can delay this process, especially in individuals with comorbidities. Blood oxygen levels are frequently insufficient in patients with chronic wounds due to poor circulation, vascular disruption, and vasoconstriction, which reduces the healing capacity.4 Supplemental oxygen accelerates angiogenesis5 by increasing wound perfusion and epithelialization.
Aim
Specific objectives
We present the case of a diabetic patient who was referred to our clinic for evaluation of a dehiscent post-surgical wound that had developed three months earlier, following a right infracondylar amputation.
Medical record: Type II diabetic, Dyslipidemia, Poorly controlled high blood pressure, chronic lower limb ischemia. He underwent femoropopliteal bypass surgery on his right lower limb. He suffered a worsening of ischemia due to obstruction and deterioration of the bypass, necessitating an infracondylar amputation of that limb. Active drinker and smoker.
Physical condition: Totally dependent. Uses a wheelchair for mobility.
Exploration
Three-month postoperative dehiscent wound in a patient with a right infracondylar amputation.
Size: 1.3 x 1 cm.
Size: 2 x 2.3 cm
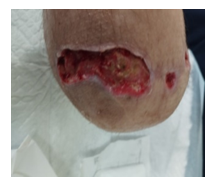
Figure 1 It presents 70% granulation tissue in the bed and 30% devitalized tissue, well-defined borders, with moderate serous exudate and no foul odor. There are no signs of infection. The perilesional area is intact.
For several months, no progress has been observed with conventional topical treatments. Due to the lack of progress in wound closure, with the likelihood of continued wound hypoxia due to small vessel disease, chronic inflammation, etc., it was decided to initiate local transdermal oxygen therapy. Before starting treatment, a holistic and thorough assessment of both the patient and the wound was performed. It is vitally important to properly prepare the wound so that there is full contact between the oxygen therapy device and the wound bed. The use of the acronym TIME (moist healing) allowed for a comprehensive approach to the different factors that can delay the healing process. (Control of devitalized tissue, Achieving bacterial control and optimal moisture management).6,7
Once the wound bed was free of devitalized tissue, there were no obvious signs of infection, and exudate control was achieved, and local oxygen therapy was administered to stimulate wound healing.

Figure 4 The system was covered with a hydropolymeric dressing with silicone adhesive edges, sealing the edges to capture oxygen generated by the system.
Using the device at home allowed for patient empowerment by involving them in the treatment. The wound had progressed significantly, managing to reduce its size (Figure 6 & 7). A decrease in the dehiscent area was observed, with an increase in granulation tissue, complete absence of devitalized tissue and decreased pain (VAS scale: 1). (Figure 8)
Continuous transdermal oxygen therapy has proven to be an effective treatment in the clinical case described. Significant benefits were observed, including a reduction in wound size, acceleration of the healing process, and an improvement in the patient's quality of life, with a reduction in the number of dressings (one per week), reduction in pain during dressings (VAS scale), and fewer trips to the hospital.
Diabetic patients often experience complications that hinder the healing process. Diabetes negatively affects blood circulation, resulting in decreased blood flow to the extremities. This compromises the delivery of nutrients and oxygen to wounds, thus prolonging the healing process and increasing the risk of complications, such as infections and chronic ulcerations. Providing oxygen directly to the ulcer area promotes cell proliferation, facilitates the formation of new blood vessels and connective tissue, and helps fight infection, which accelerates the healing process. In diabetic patients, wounds resulting from amputations are very difficult to treat due to the lack of distal blood flow. In this situation, the use of local oxygen therapy has been a viable, safe, reproducible, and successful alternative.6
It has been proven to be an effective therapy for treating hard-to-heal wounds, offering new hope for patients suffering from these chronic and debilitating conditions. As we progress, we're likely to discover even more applications and benefits of this therapy in the medical field. Therefore, we must continue working in this line and generate more scientific evidence of the application of this therapy and continue to disseminate it continuously so that nursing professionals can apply it to our patients, improving their care.7 Evidence-based recommendations support the effectiveness of topical oxygen therapy (TOT) in the management of diabetic foot ulcers, which is revolutionizing treatment approaches worldwide.8 There are studies that have documented that topical oxygen therapy in wounds is useful in rescuing ischemic lower limbs. It is vital to approach each case individually and with a multidisciplinary approach to maximize the benefits of this therapy. Considering these aspects will allow for comprehensive and personalized care, thus optimizing the outcomes of chronic wound treatment for patients.
Diabetic foot requires a multidisciplinary approach, as the limb can undergo many changes. Numerous studies show that without adequate tissue oxygen levels, wounds are very difficult to heal. Adding supplemental topical oxygen can help initiate the healing process in these types of injuries. Topical oxygen therapy, included in multidisciplinary treatment, increases the patient's functional capacity and reduces social costs. It should be considered as an adjuvant treatment for patients with difficult-to-heal wounds.
None.
This study is conducted in accordance with the Declaration of Helsinki, good clinical practice principles, and the Universal Declaration of Human Rights. The respect, confidentiality and anonymity of the participant were guaranteed in accordance with the provisions of Regulation (EU) 2016/679 of April 27 on the protection of natural persons with regard to the processing of their personal data and with Organic Law 3/2018 of December 5 on the Protection of Personal Data and Guarantee of Digital Rights10. (10. Terrón Santos D, Domínguez Álvarez JL. Regulation (EU) 2016/6 of the European Parliament and of the Council of April 27, 2016 on the protection of natural persons with regard to the processing of personal data and the free movement of such data, and repealing Directive 95/46 / EC (General Data Protection Regulation). Ars luris Salmanticensis. 2019; 7 (1): 223-8. [Links) Oral and written consent was obtained from the patient before performing any procedure related to the clinical case. The principles of nonmaleficence and beneficence established for conducting research with human subjects were followed.
The author declared that there are no conflicts of interest.

©2025 Cillero. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.