eISSN: 2373-6372


Research Article Volume 16 Issue 1
Wayne State University School of Medicine, USA
Correspondence: Paul H Naylor, Wayne State University School of Medicine Harper Hospital, 3990 John R, Detroit, MI, USA, Tel 631-243-6102 , Fax 313-745-8843
Received: January 25, 2025 | Published: February 5, 2025
Citation: Hanna A, Kim P, Wang J, et al. Racial disparity in crohn’s disease treatment in a socioeconomically challenged urban general GI clinic population. Gastroenterol Hepatol Open Access. 2025;16(1):13-20. DOI: 10.15406/ghoa.2025.16.00601
Background: Crohn’s disease (CD) is a complex entity, but most studies contain predominately non-African Americans from IBD focused practices. Further studies with diverse population are needed.
Aims: This study compares African American (AA) to non-African Americans in a general GI clinic, to assess racial disparities in disease manifestation, surgery, and therapy.
Methods: CD patients (n=136) with at least one visit between 2018 and 2020 at Wayne Health in Detroit, MI were identified. Variables obtained included endoscopic evaluations, CD relevant surgical procedures, medical therapies, medical insurance, and median income by zip code.
Results: AA patients presented with higher CRP prior to initiation of therapy, compared to non-AA patients (34 mg/L vs 20 mg/L, p = 0.048). Most surgeries occurred prior to diagnosis and treatment (90%) and were endoscopically evaluable (i.e. 95% not small bowel resections). AA patients with CD were less likely to be compliant with respect to regular visits and medication adherence as compared to non-AA (50% vs 84% p<0.005). AA patients were also more likely to be initiated on 5-ASA rather than biologic therapy (p<0.005). When current therapy was evaluated for well followed patients (i.e. treated prior to 2020 and seen in the 2021-2023 period for follow up therapy assessment). a switch from 5-ASA to biologics occurred regardless of race (34/37= 92%).
Conclusion: Racial disparities were seen in our AA compared to non-AA patients but over time the therapy differences were resolved as most patients were switched to biologic therapy.
Keywords: Crohn’s Disease, racial disparity, socioeconomical assessment, endoscopy, surgery, biomarkers
What is already known on this topic?
Crohn’s Disease manifestation and therapy is complex and variable among patients. The issue of early identification by endoscopy is hampered by the issue of ileocolonic and sigmoid colon as compared to small bowel only manifestation. Also, the increase in treatment with advanced biologics has been addressed in multiple clinical trials and large primarily non-African American databases. In both issues, the primary observations are from dedicated IBD focuses clinic and not representative of the majority of IBD patients who are identified and treated in non-IBD specialty setting.
What does this study add?
This study utilized a unique population of primarily African American and socioeconomically challenged population seen in a real-world clinic setting that is not part of a dedicated IBD clinic. The study demonstrates that an increase in the use of colonoscopy in patients suspected of CD would improve the confirmation CD in African American patients. The study also demonstrates that there has been a slow but improving increase in the use of advanced biologic therapy in this unique population but that improvement in the early use of biologic therapy remains an important goal in this population.
How might this study affect research, practice or policy?
The early referral to GI and the use of colonoscopy in patients suspected of intestinal issues should be encouraged since it would identify a significant number of CD patients for therapeutic intervention prior to the early surgical resection. The study also suggests that early use of biologic therapy in this population is needed in order to improve CD patient outcomes.
Many patients with Crohn’s disease (CD) are treated in general gastroenterology (GI) practices as opposed to dedicated inflammatory bowel disease (IBD) clinics. Complications related to Crohn’s disease are debilitating and their treatment generally requires a multidisciplinary approach, commonly including a combination of both medical and surgical therapy.1-7 Early initiation of appropriate medical therapy with a goal of avoiding surgery is preferred but may not always be possible. In addition, it is uncertain if there are racial disparities that exist in disease manifestation and if so, whether these patients require a different approach to management.8-16 The issue of surgery versus medical management is another area that has been addressed with respect to curative intent.18-22 In a study that evaluated racial disparities in surgical outcomes for IBD patients, AA patients were found to be at an increased risk of morbidity after surgery for both UC and CD.18 This raises the question of whether vulnerable AA populations face less appreciated challenges related to their IBD care.
It is imperative to identify any racial disparities that may exist regarding disease manifestation and thus therapy, to better tailor care towards these patients. In addition, given the complexity of many patients with IBD, most of the existing literature regarding therapy comes from IBD specialty physicians rather than general GI physicians, even though this may not be representative of the demographics of the patients receiving care in real clinical practice. It is valuable to have real world data available to demonstrate how to approach and manage IBD patients in a general GI practice. These types of studies can also address the differences with respect to general GI vs IBD Clinics and the use of symptomatic as opposed to endoscopic evaluation of disease activity to assess sustained deep remission. Also important is how these practices assess treat to target approaches involving assessment of inflammatory activity. Real world studies are also instructive with respect to providing treatment utilization in settings where a variety of clinical trials are not available, and insurance coverage can present significant barriers to treatment decisions.
The overall goal of this study was to evaluate racial disparity in the epidemiology and management of Crohn’s disease patients in a general GI clinic with a predominantly African American population and a significant number of socioeconomically challenged patients. Both surgical and medical therapies were evaluated. The objective was to assess not just the effectiveness of therapy, but also the methods of assessing patient outcomes with respect to mucosal healing, factors associated with need for surgical intervention, and the possibility that symptomatic clinical assessment was more predominant as compared to mucosal healing in determining patient response to treatment. Based on the assumption that increased use of biologic therapy would occur with time, we evaluated potential shifts in therapeutic treatment initiation in patients first seen between 2018 and 2020 and with a subsequent therapeutic evaluation post 2022.
Population
Wayne Health, as the medical practice of the Wayne State University School of Medicine, predominantly serves patients living in the Detroit Metropolitan area. The Wayne Health Clinics electronic medical records (EMRs) were used to identify patients with an ICD-10 diagnosis (K50.90) of Crohn’s Disease with a visit between 2018-2020.
Variables
The EMRs of the patients identified in the data extraction were used to confirm the correct diagnosis of CD. Using a case report form, we gathered variables including visits to GI and non-GI physicians, medical histories, demographics, endoscopic results, laboratory results, CD relevant surgical procedures, medical therapies, and therapeutic interventions. We also identified patients with adequate documentation to determine compliance, medical insurance (Medicaid, Medicare or other), and median income by zip code. Compliance to therapy was identified using physician notes, including appointment and medication compliance.
We required that all patients have at least one GI or surgical evaluation for documentation of their CD. Endoscopic evaluation at earliest visit and subsequent visits was scored by a single GI fellow as either mild (minimal inflammation), moderate (modest inflammation, bleeding, or ulcerations), or severe (significant inflammation and multiple ulcerations, bleeding, or fistula complications). Endoscopic change over time with respect to current therapy was scored as improved, stable, or worsening as compared to the initial staging. The date of the initial/earliest and most recent therapy in the 2018-2020 data set was determined and if unclear, the earliest visit date was used. The data was then expressed as initial treatment in each year. Potential changes in therapy were first evaluated by comparing therapy between patients at least 4 years apart in the 2018-2020 data set. To reflect more accurately on the most recent therapy and potential shifts in therapy, patients who were seen in 2018-2020 with a follow up visit between 2021 and April 2024 were further analyzed to compare earliest and most recent therapy.
Statistical analysis
Statistical analysis was performed using JMP software from SAS. Numeric variables were evaluated using ANOVA and character variables using Chi-Square Pearson Analysis. Matched Pairs analysis was used to compare early and recent changes in individual patients.
Demographics and clinical characteristics
Of the 249 patients with an ICD 10 diagnosis of CD between 2018 and 2020, we identified 136 patients with at least one well documented visit in GI. The population was predominantly AA (72%) as compared to non-AA with slightly more males (54%). The earliest year of record based on the EMR was 1988. The average age of diagnosis/first visit was 28 years with a range from 6 to 80 and quartiles of 17 to 37 (Table 1). Based on endoscopic evaluation, the most likely site of involvement was ilio-colonic with a few patients having only colon or anal involvement. The only potential racial difference was anal involvement for AA as compared to non-AA.
|
All (n=136) |
AA (n=98) |
Non-AA (n=38) |
P value (race) |
Female (n=63) |
Male (n=73) |
P value (gender) |
|
|
Male (n= 74) |
53% |
48% |
67% |
||||
|
Female (n=65 |
47% |
52% |
33% |
p<0.05 |
|||
|
Age at Date of Service (years) |
42 |
41 |
43 |
40 |
44 |
||
|
Age at Diagnosis Years) |
28 |
28 |
28 |
30 |
28 |
||
|
Earliest CRP (mg/L) |
28 |
36 |
16 |
p<0.05 |
15 |
39 |
P<0.0005 |
|
Calprotectin (n=24) (ug/mg) |
268 |
289 |
123 |
198 |
351 |
||
|
GI Visits>2 thru 2022 |
64% |
64% |
67% |
61% |
67% |
||
|
Location at Diagnosis |
n= 121 |
n=87 |
n=34 |
p=0.62 |
n = 57 |
n= 64 |
p=0.83 |
|
Ilio-colonic |
30% |
28% |
32% |
33% |
27% |
||
|
Ilio-colonic (plus other) |
22% |
21% |
24% |
21% |
23% |
||
|
Colon |
22% |
20% |
29% |
19% |
25% |
||
|
Colon (plus other) |
6% |
7% |
3% |
6% |
6% |
||
|
Anal (plus other) |
17% |
20% |
9% |
16% |
17% |
||
|
Small Bowel |
3% |
4% |
3% |
5% |
2% |
Table 1 Demographics and Lab results for all 136 patients with at least 1 GI visit
Surgical procedures
At least 1 surgery was confirmed for 65 of the 130 CD patients with sufficient documentation in our dataset (49%) with 90% (59/95) occurring prior to any treatment (Table 2). Six patients were on therapy prior to their surgery and were deemed compliant, although none were on biologic therapy at the time of surgery. Three surgery patients were non-compliant with medication after a GI visit and were included in the “non-treated” surgery group (n=59). Surgery in the untreated patients was more likely in males as compared to females (54% vs 35%, p<0.05) and AA as compared to non-AA (48% vs 39%, p=0.43). The average age of surgery was 35 years (majority between 20 and 50). For the 59 “non-treated” surgery patients, the dominant surgery was an ileocolonic procedure or small bowel with multiple additional colonic procedures (63%; Table 2). Neither race nor gender were statistically significantly different with respect to the surgical procedures, although AA and male patients were more likely to have anal fistula involvement compared to females and non-AA patients. Only 5% of patients had a resection of the small bowel with no other indication of colonic involvement. Thus, most patients had endoscopically evaluable CD (last column) and were thus candidates for early diagnosis and therapy which could be monitored via endoscopic procedures.
|
Surgery |
Small Bowel (ileo-colonic) |
Small Bowel (multiple) |
Small Bowel (only) |
Anal fistula |
Colectomy |
Endoscopically Evaluable/Therapy Candidate |
|
|
Total (130) |
N=59 (45%) |
32% |
31% |
5% |
22% |
10% |
95% |
|
GENDER |
|||||||
|
Male |
n=37 (54%) |
24% |
34% |
5% |
27% |
8% |
95% |
|
(n=68) |
|||||||
|
Female (n=62) |
N=22 (35%) |
45% |
23% |
5% |
14% |
13% |
95% |
|
RACE |
|||||||
|
AA |
N=44 (48%) |
32% |
27% |
5% |
27% |
9% |
95% |
|
(n=92) |
|||||||
|
Non-AA (n=38) |
N=15 (39%) |
33% |
40% |
7% |
7% |
13% |
93% |
Table 2 Surgery in Patients Prior to Diagnosis and Treatment of Crohn’s Disease
Inflammation
Since inflammation as defined by serum levels of C-Reactive Protein (CRP) is a readily measured value in most patients with CD, it was used to define initial inflammation as well as to assess impact of therapy over time (Table 1 & Figure 1). AA patients had higher CRP early in their disease as compared to non-AA patients (36 mg/L vs 16 mg/L). When improvement of CRP over at least 1 year of treatment was assessed in patients using matched pair analysis, both AA and non-AA patients improved in individual CRP (Figure 1). While on average patients had an improvement in CRP while on therapy, as defined by pair wise analysis, a significant number of patients still failed to approach the average normal baseline level of 5 mg/L. With respect to race, AA patients were less likely to achieve normal levels as compared to non-AA patients.
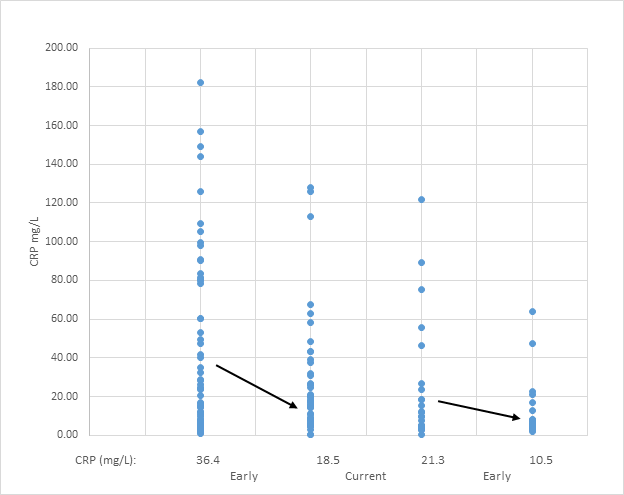
Figure 1 Race and Inflammation by C-reactive Protein in Response to Therapy. C-Reactive Protein (CRP) levels (mg/L) are plotted for individual matched patients as a function of earliest visit vs most recent visit for patients on therapy for at least 1 year. There were 74 AA and 27 non-AA who qualified for inclusion in the analysis. The average value at earliest assessment was higher for AA as compared to non-AA (See table 1 for all patients at earliest value). The arrows represent the average which declines on therapy. The statistical significance of the decline as defined by the paired t test for matched variables of AA patients is p=0.0002 and for non-AA p=0.074. Normal CRP is defined as <10 meaning most patients on treatment were still elevated as compared to normal.
While fecal calprotectin can be used as a non-invasive marker for inflammation, it was rarely assessed in our population (AA= 21; non-AA= 3) and only three of the values were for AA patients prior to treatment initiation (Table 1). In the few patients who were evaluated at any time during their treatment, the average was 289 ug/mg for AA and 123 ug/mg for non-AA. While this suggests the majority had inflammation as defined by levels higher than our normal range of 10-60, the increased inflammation for AA and males was not statistically different due primarily to the low numbers of patients who had fecal calprotectin values available in the EMR.
Endoscopy: Initial and mucosal healing
There were no differences in disease severity as defined by endoscopy with respect to race, but males were more likely to have severe Crohn’s disease (Table 3). Severe disease patients at the time of early endoscopy were more likely to have surgery prior to treatment. Inflammation as defined by elevated C-reactive Protein (CRP) was highest for severe patients as compared to patients with less severe disease. With respect to medical therapy response as defined by mucosal healing, 97 patients (97/136= 71%) had an endoscopic assessment available for review at their early GI visits and 78 had a repeat endoscopy. Repeat endoscopies had an average time of 7 years apart and only 23 (30%) were within even 5 years. Patients with the most severe disease at early visit were more likely to have a worsening of disease on therapy (54%) as compared to mild (31%) and moderate (15%). With respect to therapy and endoscopic improvement, patients with worsening disease were more likely to be on biologic and combination therapy than healing or stable patients (Figure 2).
|
Mild Disease at Entry |
Moderate Disease at Entry |
Severe Disease at Entry |
|
|
Race |
|||
|
AA (n= 71) |
37% |
30% |
34% |
|
Non-AA (n=26) |
35% |
31% |
35% |
|
Gender |
|||
|
Male (n=52) |
34% |
23% |
46% (p=0.023) |
|
Female (45) |
42% |
38% |
20% |
|
Surgery |
|||
|
All Surgery |
41% |
31% |
78% (p=0.0036) |
|
Anal Fistula Surgery |
3% |
0% |
33% (p=0.0004) |
|
Laboratory Results |
|||
|
Inflammation (C Reactive Protein) |
24 mg/L |
26 mg/L |
52 mg/L (p=0.021) |
|
Initial Disease Severity and Subsequent Endoscopic Improvement |
|||
|
Mucosal Healing |
40% |
30% |
30% |
|
Stable Disease |
47% |
32% |
21% |
|
Worsening of Disease |
31% |
15% |
54% |
Table 3 Endoscopic Assessment of Mucosal Disease Severity and Improvement
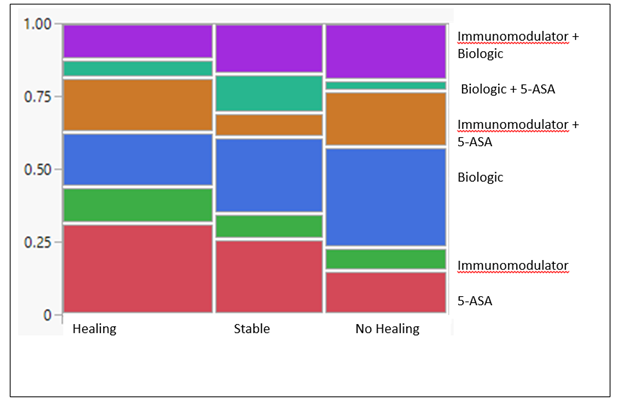
Figure 2 Current Crohn’s Disease Therapy and Endoscopic Change. CD patients with two endoscopic evaluations at least 1 year apart were assigned one of three changes in endoscopic appearance as compared to initial endoscopy (Healing, Stable, or Worsening). There was no therapy that statistically dominated the healing patients as compared to Stable and Worsening, although 5-ASA was less likely to be seen in patients with no Healing.
Racial disparities in therapy
There was racial disparity with respect to the earliest recorded therapy which was most likely to be aminosalicylate (5-ASA) drugs and less likely to be anti-TNF biologics, for AA as compared to non-AA (Figure 3a, p<0.005). When the dates of earliest therapy were grouped into similar numbers of patients, it was possible to evaluate whether therapeutic options were different in recent as compared to earlier time periods (Figure 3b). As shown in Figure 3b, 5-ASA dominated initial treatment in all time periods and early biologic use continued to be more likely in non-AA patients. A switch from earliest therapy could be evaluated for 50 patients where data was available for at least a 3 year follow up (Figure 4). The change in therapy was mainly a decrease in 5-ASA (79% to 8%) and an increase in biologics (12% to 42%). Both AA and non-AA patients showed this trend which bodes well for a reduction in racial disparity over time in patients where a change in therapy could be evaluated. Overall, 75% of CD patients had a change in therapy within 3 or more years after initial therapy. The data set is limited since most of our patients (65/132= 50%) had no follow up (34) or less than 4 years of treatment data (31).

Figure 3 Race and Class of Therapy for Crohn’s Disease. a) Earliest therapy for CD by class of therapy and race. The use of 5-ASA more frequently in AA as compared to non-AA was significantly different (p<0.005). b) Change in initial therapy as a function of year of initiation and race. The dominance of 5-ASA as initial therapy, especially in AA was consistent and more often used for AA as compared to non-AA. There was a trend for a decrease in 5-ASA use but was more pronounces in non-AA as compared to AA.
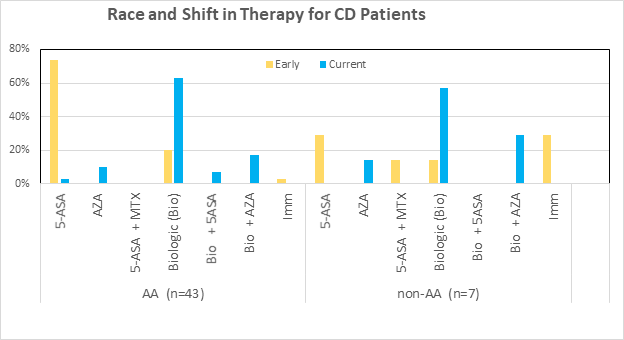
Figure 4 Race and Shift in Therapy for Crohn’s Disease Patients. Change in therapy for patients with at least 3 years between visits between 2018 and 2020. The data is presented as early therapy vs recent therapy for patients seen prior to 2020. There was a switch to biologics due to poor performance of the dominant 5-ASA initial therapy regardless of race.
To provide updated assessment of current therapy in compliant and well followed patients, we assessed the hypothesis that patients would be switched to biologic therapy if they continued to follow up. We identified patients with a GI visit between 2021 and 2024 and who had a prior therapy visit in the database. As shown in figure 5 although most patients started initially on 5-ASA (see Figure 3), patients with a post 2020 visit were likely to shift to therapy containing a biologic (32/36=89%). While 67% of recent patients were receiving anti-TNF biologics, significant numbers of 2nd generation therapeutics (primarily anti-integrins and anti-IL-12/23) were also in use.
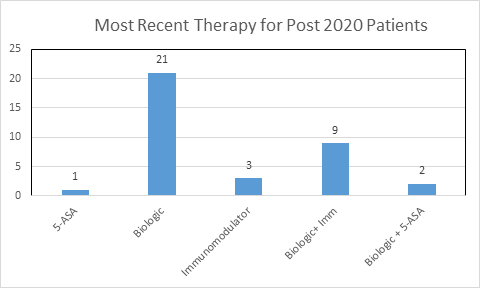
Figure 5 Most recent therapy for patients seen post 2020. There were 36 CD patients initially treated prior to 2021 and who had at least one subsequent visit post 2020. Switching to a biologic with or without an immunomodulator was the dominant therapy as compared to the early patients where 5-ASA was the dominant therapy.
Impediments to care
To assess the issue of potential impediments to care (poor follow-up, lack of compliance and insurance issues), we identified 126 patients with adequate data to evaluate socioeconomic and racial disparity (Table 4). The most significant observation was that AA patients with CD were less likely to be compliant as compared to non-AA (50% vs 84%). They were also more likely to have an insurance impact on treatment (24% vs 8%). When the % of patients with Medicaid were evaluated by race, AA were more likely to be on Medicaid as compared to non-AA patients (80% vs 56% p<0.005). When socioeconomic status by Zip code defined median income was evaluated by race, AA patients had a lower income ($37,000 vs $70,000, p=0.001). When income and compliance regardless of race was evaluated, it was not different ($50,000 vs $44,000, p=0.32). This was also true when race was eliminated for insurance effect on compliance and the class of CD therapy. When subjected to multivariate nominal logistic analysis, race remained the only significant factor in compliance (last column in Table 4).
|
Compliant with no Insurance Issues |
Insurance Impact |
Non-compliant |
p value (Pearson univariate) |
P value (Multivariate Nominal Logistic Fit) |
|
|
Race (AA)(n= 90) |
50% |
24% |
25% |
P=0.003 |
P=0.0086 |
|
Race (non-AA)(n=36) |
84% |
8% |
8% |
||
|
Gender (Male)(n=70) |
58% |
21% |
21% |
P=0.81 |
P=0.045 |
|
Gender (Female) (n=56) |
62% |
18% |
20% |
||
|
Insurance |
|||||
|
Medicaid (n=99; 73%) (AA= 80%; non-AA= 56%)* |
56% |
20% |
24% |
P=0.64 |
P=0.63 |
|
Medicare (n=16; 12%) (AA=10%; non-AA 11%) |
70% |
23% |
7% |
||
|
Other(n=21; 15%) |
68% |
21% |
21% |
||
|
Median Income |
|||||
|
<30 K (n=26) |
46% |
31% |
23% |
P=0.16 |
P=0.32 |
|
31-34K (n=22) |
59% |
9% |
32% |
||
|
35-40K n= 25) |
52% |
24% |
24% |
||
|
41-59K (n=32)_ |
66% |
25% |
9% |
||
|
> 60K (n=21) |
76% |
5% |
19% |
||
|
CD Therapy |
P=0.35 |
P=0.14 |
|||
|
5-ASA (n=34) |
56% |
15% |
29% |
||
|
Immunomodulator (n=12) |
58% |
42% |
0% |
||
|
Biologic (n=35) |
63% |
20% |
17% |
||
|
5-ASA+ Immunomodulator (n=18) |
61% |
17% |
22% |
||
|
5-ASA + Biologic (n=8) |
50% |
13% |
37% |
||
|
Immunomodulator + Biologic (n=15) |
73% |
20% |
7% |
Table 4 Demographics, Insurance, Socioeconomic Status (Income by Zip code) and therapy for CD
* Indicates that AA are significantly more likely to be on Medicaid for their insurance as compared to non-AA (p<0.005).
The management of patients with Crohn’s Disease can be complex, and thus it is imperative to understand the epidemiology of these patients, especially with respect to potential racial disparities. In our predominantly AA outpatient general GI clinic there is an opportunity to evaluate racial differences which may not be apparent in clinical trials where non-AA patients are the dominant population. We found that surgery prior to diagnosis was more likely in AA patients compared to non-AA patients and that for many patients it was the first diagnosis of CD. Males were more likely to undergo surgery compared to females. One study similarly found an increase in CD-related surgery in African American patients compared with non-AA.18 Conversely, other studies report minimal difference in need for surgery among different races while others reported increased need for surgery in non-AA compared with African Americans, Hispanics, or Asians.19-22 This was confirmed in a recent meta-analysis by Booth et al. addressing surgery utilization where they also found conflicting observations and concluded that multiple factors outside of race were more significant than race itself with respect to surgical decisions.22 Regardless of the issue related to race, an important finding of our study was that most surgical interventions regardless of race in our population were for ileo-colonic disease that would have been detected if patients had undergone appropriate endoscopic assessment prior to surgery. Such a finding would then ideally be followed by treatment and perhaps the potential to avoid surgical procedures. This showcases one of the many barriers our patient population (and other urban populations) faces regarding receiving timely and appropriate diagnostic care and thus the potential to prevent surgery due to severe disease progression. With respect to the issue of surgery post treatment, it was rare as compared to the number of patients who had surgery as their initial diagnosis of CD. Thus, surgical management plays a minimal role in our patients who are being treated for their CD, suggesting therapeutic intervention is effective in our general GI clinic population.
With respect to racial differences in manifestation of CD, the most dramatic finding in our data set was inflammation as defined by CRP. While CRP is not specifically diagnostic of CD, it is typically followed in CD patients to assess for disease activity in conjunction with endoscopic findings, with a decline or improvement in CRP indicating successful therapy. Even though AA patients had statistically significant elevation at the earliest visit compared to non-AA, both populations had a decline in CRP when measured at least 1 year after therapy initiation. While a decline did occur in most patients, AA patients still failed to achieve levels that were similar to that of treated non-AA patients. It is unclear what the clinical relevance of statistically significant difference in baseline CRP in AA patients compared to non-AA patients is, however, it may suggest more severe disease at initial presentation. One of the clearest deficiencies with respect to assessing inflammation in the clinic population was the lack of fecal calprotectin measurements. CRP and fecal calprotectin are typically ordered at the same time; however, there are barriers with collecting fecal calprotectin in comparison to CRP. CRP is easily obtained via blood work and can be done prior to leaving the clinic visit, but majority of patients are unable to provide a stool sample for fecal calprotectin at the time of office visit, and face barriers in returning to clinic when they are finally able to provide a stool sample. Thus, because of the lack of objective data regarding fecal calprotectin, it was not being used as a criterion for treatment response in the population as opposed to CRP, despite this being the standard of care. This highlights one of many challenges that patients in an urban population face when being treated for CD.
While mucosal healing is recommended to define response to therapy, its utility in a general GI practice has not been fully investigated. Regarding endoscopic mucosal assessment, there were no differences in disease severity comparing different races, despite the difference in inflammation as defined by CRP. There was, however, noted to be more severe disease in males compared to females. Consistent with multiple observations, patients who had severe disease at initial endoscopic assessment were more likely to fail to improve with initial therapies. The most striking observation was that only 30% of patients had a repeat colonoscopy in less than 5 years. Based on the medical record reviews, it is not clear why there is a failure to follow most patients on a more frequent basis. Thus, our data does not speak directly to the issue that physicians in a general GI clinic are not utilizing endoscopic assessment for monitoring disease status and determining therapeutic efficacy. While this could create a barrier in delivering quality healthcare to our already vulnerable patient population, the fact that patients who are compliant with their visits and are being followed by patient reported health assessment were switched to biologics may mediate this issue. Yet evaluated, however, is the issue of following those patients who are now on biologics (and represent most CD patients in our clinic) with respect to how frequently the switch to a 2nd generation biologic is needed.
Interestingly, our data showed that aminosalicylates were more likely to be used as earliest therapy in African American patients compared to non-African American patients. The management of Crohn’s disease has changed tremendously over recent years, as newer and more efficacious therapies have been developed. Our data set regarding earliest therapy is more consistent with older therapies such as aminosalicylates. The racial disparity in early treatment of patients with Crohn’s disease was striking and driven by an increased ratio of 5-ASA use to biologics in AA as compared to non-AA. Somewhat unexpected was that this disparity with respect to earliest therapy was true regardless of when the therapy was initiated between 2012 and 2020. Racial disparity diminished in the patients with a visit post 2020 as they were shifted from 5-ASA to biologics. Yet to be evaluated is whether patients first seen in 2021-2024 receive biologics as first line therapy for their IBD.
While this may not reflect current therapy in use in 2024, even as late as 2020, 5-ASA was utilized in significant numbers of patients with AA being more likely to have it as first line therapy than non-AA. The argument could thus be made that even as late as 2020, some sort of step-up therapy (5-ASA to immunomodulators to biologics) was still the dominant practice for patients with CD in our practice. It is unclear why this was the case throughout the years this study was done; however, given the variety of healthcare obstacles our patient population face could have played a factor. Socioeconomic issues facing our patients could include the lack of insurance or subsidized insurance via Medicaid Advantage Plans created barriers to prescribing newer, more expensive medications. As demonstrated in the income and insurance studies, our population, especially the AA cohort, had state subsidized Medicaid advantage plans and lived-in low-income areas. While the data is not sufficient to completely implicate medical insurance payer as the main reason, a closer evaluation of the issue of Medicaid approval of biologic therapy as a first line approach needs further evaluation. Also not assessed what the subtle impediment related to the hassles of prior authorization for biologics in IBD treatment. Regardless, the earliest therapy practices should have changed accordingly to guidelines and transitioned to biologics rather than aminosalicylates, corticosteroids, and immunomodulators.
Overall, our study found significant racial differences using our predominately African American general gastroenterology urban clinic population. We found that AA patients were more likely to require surgery especially when evaluated prior to diagnosis and treatment. They also had more inflammation as defined by elevated c-reactive protein and were more likely to be started on aminosalicylates as compared to biologics or immunomodulators for initial therapy. Race was also a dominant reason for compliance and socioeconomic changes as compared to non-AA patients. While the significant AA population has provided an opportunity to evaluate diversity, the improvement in the use of biologics in the patients see for post 2020 visits and the need to focus on improved compliance of our patients bodes well for the patients in similar settings.
This project was supported in part by an Investigator Initiated Grant (NOPRODIBD4001) from Janssen Scientific Affairs to Milton G Mutchnick and Paul H Naylor.
This study involves human participants and was approved by the Wayne State University Institutional Review Board (IRB # 082215M1E). The study did not use animal subjects.
There was no conflict with respect to other authors on the manuscript.
There was no input from the public with respect to the study and manuscript generation as this was a retrospective IRB approved study and the data collection and analysis was via the experiences team at the medical center.
Angy Hanna- Acquisition of data, analysis, interpretation of data, drafting the article.
Paul Kim- Acquisition of data and manuscript review.
Jing Wang- Acquisition of data and manuscript review.
Jasdeep Bathla- Acquisition of data and manuscript review.
Danielle Paradela- Acquisition of data and manuscript review.
Neel Patel- Acquisition of data and manuscript review.
Maryam Haider- Acquisition of data and manuscript review.
Erica StLawrence- Acquisition of data and manuscript review.
Yechiel Mor- Acquisition of data and manuscript review.
Bashar Mohamad- Data evaluation and manuscript review.
Paul Naylor- Conception and design of the study, analysis and interpretation of data, revising manuscript critically for important intellectual content, final approval of the version to be submitted.
Milton Mutchnick- Conception and design of the study, interpretation of data, revising manuscript critically for important intellectual content.

©2025 Hanna, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.