eISSN: 2373-6372


Review Article Volume 16 Issue 2
1Richard Semelka Consulting, PLLC, USA
2Department of Radiology, Hospital da Luz, Portugal
Correspondence: Richard Semelka, MD, Richard Semelka Consulting, PLLC, 3901 Jones Ferry Road, Chapel Hill, NC, USA
Received: March 20, 2025 | Published: April 4, 2025
Citation: Semelka RC, Ramalho M. Pancreas. Abnormalities observed in splanchnic inflammatory syndrome and (splanchnic) metabolic syndrome. Gastroenterol Hepatol Open Access. 2025;16(1):51-53. DOI: 10.15406/ghoa.2025.16.00607
This review describes pancreas abnormalities observed in the Splanchnic Inflammatory Syndrome and the (Splanchnic) Metabolic Syndrome. We report herein the development of fatty change of the pancreas and describe our qualitative assessment of severity, and also report our opinion that cystic change also is a common response to general inflammation in the splanchnic system.
The Splanchnic Inflammatory Syndrome (SIS) represents the imaging findings apparent in organs in the splanchnic system that arise in the setting of diffuse inflammation. The hallmark features are inflammatory changes of segments of the upper digestive tract coupled with hepatosteatosis, the entry and exit points of the splanchnic system.1,2 The clinical picture of this constellation of findings includes diseases ranging from leaky gut to irritable bowel syndrome to the (splanchnic) Metabolic Syndrome.1
Prior reports have focused on other organs in the splanchnic system that show abnormalities due to this pan inflammation, including the digestive tract,1 the liver,2 the gallbladder and biliary tree,3 and the mesentery.4 Solid organs in the splanchnic system respond to inflammation in a consistent pattern. Fatty change is the most common response of the liver to inflammation,2 hence it is reasonable to assume that this would also occur with the pancreas. Pancreatic cysts have over the recent two decades been reported as a common finding in the pancreas. There has been uncertainty whether this observation reflects that current MR systems and techniques are better at defining small cysts than previously possible, or whether pancreatic cysts have become more common in the general population.5 This review describes findings observed in the pancreas in the setting of the Splanchnic Inflammatory Syndrome/ Metabolic Syndrome.
Two principal abnormalities in the pancreas are pancreatosteatosis and cystic changes, which can be graded in severity. The following is the subjective grading that we have devised:
Pancreatosteatosis (fatty pancreas, FP)
Regional fatty replacement of the pancreas is common. The most common form is fat deposition in the posterior head of the pancreas, sparing the neck, body, and tail.5 Care must be taken to not describe fat in the head as a pancreatic mass, which is easy and commonly done on CT. Demonstration on in-phase/out-of-phase paired images shows that the focus is iso-intense to slightly brighter with the pancreas on in-phase and dark on out-of-phase. This differential fat deposition arises because the posterior head and the remainder (neck, body, and tail) of the pancreas are embryologically separated during fetal development, so they have separate vascular supply. The association between regional fat deposition of the head and SIS is currently unclear.
Pancreatic cysts
Cystic lesions in the pancreas that are not congenital and not secondary to pancreatitis may be due to the SIS. Cysts range in size from 3mm to 2 cm and vary in number and location. The Intraductal Papillary Mucinous Neoplasm (IPMN) family of lesions also may arise in this setting. The correlation between the size, number, type of cysts, and the severity of SIS has not yet been established.
Other pancreatic lesions
It is probable that other disease processes in the pancreas may also arise secondary to SIS. These include acute and chronic pancreatitis and pancreatic ductal carcinoma. Presently, there is insufficient experience to establish the relationship.
The SIS was initially reported in a research study that examined for associated findings in the splanchnic system observed in subjects with fatty liver.2 In that report, the correlation with inflammatory changes in the upper digestive system was extremely high, seen in 98 of the 100 subjects studied. Additional findings affecting other organs in the splanchnic system were described, including gallbladder and mesentery. In that report, fatty pancreas was described in 23 subjects and pancreatic cysts in 15.
It should be no surprise that the pancreas should respond with a fatty change in the presence of prolonged low-grade inflammation, as this is the process observed with the liver. A prior study describing the (Splanchnic) Metabolic Syndrome reported a relatively common occurrence of fatty pancreas.1 This is what we are describing herein. Furthermore, this report provides a grading system for fatty changes in the pancreas. We should note that we rarely describe the presence of minimal fatty change in imaging reports and only do so in the setting where it may fit with the particular clinical picture. Hence, we only describe fatty change if it is at least mild. We have also observed that beyond the age of 75, mild fatty change is extremely common, so we rarely mention it in this group. Complete fatty replacement of the pancreas is virtually always due to Cystic Fibrosis6,7 and is not seen in SIS. Since that initial research report, further clinical experience with attention drawn to the splanchnic organs, 5-min delayed pronounced enhancement of the jejunal serosa was a feature observed in the setting of these small pancreatic cysts. The serosal enhancement we interpreted represents that jejunal inflammation had extended beyond the jejunal wall. It should be noted that this same late serosal enhancement was present in cases of mesenteric panniculitis. Interestingly, mesenteric panniculitis and pancreatic cysts did not seem to have a high correlation with each other. This may suggest that mesenteric panniculitis traps inflammation and represents a barrier hampering inflammation from extending to the pancreas (Figure 1-3).
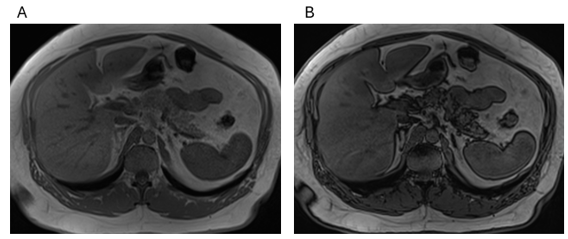
Figure 1 Moderate fat infiltration. Axial T1 Dixon GRE: In-Phase (A), Out-of-Phase (B) images. Fat interdigitations are deeper and broader in thickness than observed in mild changes. Note that several lobules of pancreatic parenchyma exhibit a loss of signal (darkness) on out-of-phase images consistent with direct fatty deposition.
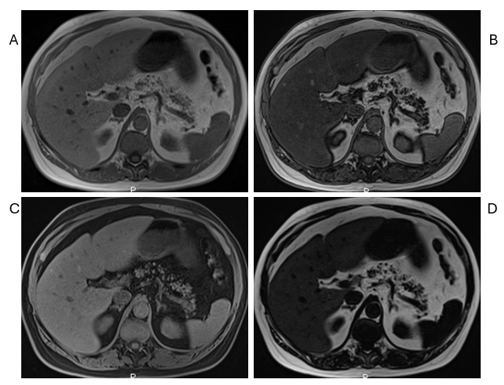
Figure 2 Severe fat infiltration. Axial T1 Dixon GRE: In-Phase (A), Out-of-Phase (B), Fat Sat (C), and Fat only (D) images. Severe pancreatic steatosis appears subjectively as the total fat content of the pancreas to be approximately 75% of the gland.
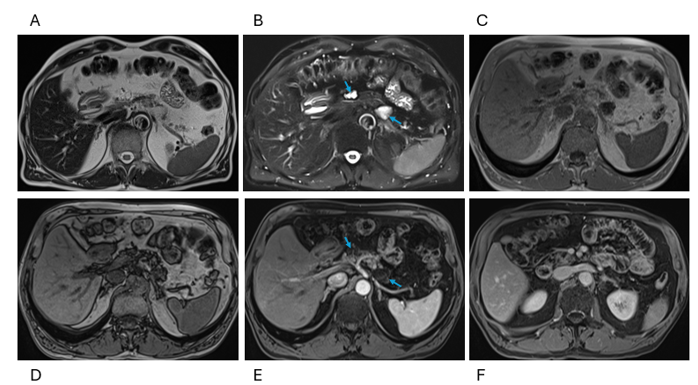
Figure 3 Pancreatic cysts. Axial T2 HASTE (A), T2 HASTE Fat Sat (B), T1 Dixon GRE In-Phase (C), Out-of-Phase (D), arterial phase (E), and interstitial phase (F) images. Note that cysts are not as well shown on T2 nonfat sat images (A) as cysts and Fat are both bright. Small cysts are best shown as small bright foci on snapshot T2 weighted fat sat images (arrow, B). T1 IP / OP imaging shows moderate steatosis, early pancreatic enhancement is normal, and cysts remain dark (arrows, E). In the 5-minute post-contrast images (F), the adjacent jejunum shows late prominent enhancement and late enhancement of the serosal surface.
To date, we have not attempted to draw a clinical correlation between the severity of disease in SIS in subjects with varying sizes and numbers of cysts and IPMNs. That said, it stands to reason that a greater number and complexity of cysts should reflect a greater severity and/or duration of inflammation. The association with acute and chronic pancreatitis is at present uncertain. Of greatest interest/concern is the level of association and possible causation with pancreatic ductal carcinoma. It is well established that chronic inflammation shows strong causation for several malignancies, including the pancreas.3, 8-10 The intention of this report, and earlier reports of the SIS and inflammation of individual organs and tissues, is to draw attention to these findings for other investigators to look into and extend the depth and breadth of knowledge. Until recently, it has been felt that there are no imaging findings in several upper digestive system conditions, such as leaky gut and irritable bowel syndrome. However, this reflects a couple of reasons: 1) the unfamiliarity with radiologists in recognizing these present findings, and 2) that it has not been common practice to perform 5-minute post-contrast T1 weighted gradient echo imaging. This data set has been invaluable to show the increased enhancement of inflammation. We are convinced that the basic concept of Splanchnic Inflammatory Syndrome is correct. What remains to be investigated is the frequency of its occurrence in association with multiple other inflammatory and neoplastic conditions in the Splanchnic system.
In conclusion, this report describes and categorizes the severity of fatty pancreas in SIS and the frequent presence of pancreatic cysts.
None.
None.

©2025 Semelka, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.