eISSN: 2378-315X


Research Article Volume 12 Issue 5
1 Department of Pharmacology and Toxicology, College of Pharmacy, Taif University, Saudi Arabia
2 Pediatric Emergency medicine consultant, Head of pediatric ER, Alhada Armed Forces Hospital, Saudi Arabia
3 College of Pharmacy, Taif University, Saudi Arabia
4 College of Pharmacy, Umm Al-Qura University, Saudi Arabia
Correspondence: Khadeejah Alsolami, Department of Pharmacology and Toxicology, College of Pharmacy, Taif University, Saudi Arabia
Received: November 01, 2023 | Published: November 21, 2023
Citation: Alsolami K, Alharthi MA, Al-harthi SS, et al. Socio-demographic and environmental factors impacting asthma exacerbations in children in Taif city, Saudi Arabia. Biom Biostat Int J. 2023;12(6):156-163. DOI: 10.15406/bbij.2023.12.00399
Background Asthma is a chronic inflammatory disorder of the airways resulting in episodic reversible obstruction of the airways leading to breathlessness, tightness, chest, cough and wheezing. Children with bronchial Asthma lifestyles are disrupted to various extents based on bronchial Asthma severity. School-aged children with asthma experience more hospitalizations, more school absenteeism, academic underachievement, decreased overall activity, and disruption of family functioning compared to healthy classmates. The incidence of asthma has increased considerably in the last few years. Aims: The aim of this study was to assess the role of associated sociodemographic and environmental risk factors in the severity of school-aged children's asthma in Taif, Saudi Arabia, for providing care to a child. Methodology: In a case-control cross-sectional study, the incidence and severity of asthma symptoms were carried out through well-designed questionnaires distributed during the period from April to May 2023 according to 11 standardized methods of population-based survey protocols. Results: The incidence frequency of bronchial asthma was (51.09%). The highest incidence rate of asthma was reported among the age group of 8-10 having a percentage of 36% followed by the age group of 10-12 (33.5%) and the age group 6-8 (30.5%) having the lowest incidence rate of asthma. Allergens and weather conditions were the most prevalent factors triggering severe and exacerbating childhood bronchial Asthma attacks. Conclusion Pediatric Asthma is one of the most common chronic pediatric chest inflammatory disorders. Consistently children with Asthma have lower life quality. Children with asthma can live safely after narrowing these factors. Physicians must promote to patients the necessary knowledge and care for effective self-management of the disease process and improve life quality. These results offer sufficient information regarding the incidence rate and severity of asthma symptoms, asthma management, and related risk factors for Saudi Arabian health authorities to scale up surveillance initiatives, control, and high-impact treatments.
Keywords: bronchial Asthma, chronic bronchial Asthma, socio-demographic risk factors, cross-sectional study
The most common chronic illness in children is bronchial asthma (BA), which is often develops early in infancy,1,2 and defined by repeated attacks with Common asthma complaints including wheezing, coughing and shortness of breath. The incidence rate of asthma in early childhood has considerably increased recently in several nations around the world.2,3
There are presently 235 million asthma sufferers worldwide, which puts significant pressure on the world's healthcare systems, according to the World Health Organisation (WHO).4 In several countries, it has been determined what percentage of children under the age of six have asthma.5,6 Asthma in the family, being a man, having a significant infection in the first two years of life, and smoking are a few more risk factors for developing asthma as a child.7,8 Repetitive BA symptoms are frequently signaled by sleep issues, daytime weariness, decreased activity levels, and absences from school and work.9
Increase the bronchial asthma severity by being subject to environmental agent’s irritation conditions, including an increase in urban residential lifestyles and more developed industrial areas.10 Socioeconomic status, traffic air pollution, pollen, cold weather and indoor mold essentially trigger severe bronchial asthma in children between the ages of three and six.11 In addition, non-adherence to therapy, concurrent allergic rhinitis, and disease duration of more than two years with asthma were risk factors for uncontrolled severe bronchial asthma in children.12
The Saudi Initiative for Asthma (SINA) group was established in 2008 by the Saudi Thoracic Society to address the issue of the rising incidence rate of asthma in the nation. Its main objective is to update management guidelines for medical professionals who treat Saudi residents with asthma.
In Saudi Arabia, the Saudi Thoracic Society observed the rising incidence rate of asthma among Saudi residents.13 More than 2 million people suffer from asthma making it one of the most prevalent chronic diseases in the country and the incidence rate has shown an increasing trend recently.14
Al-Dawood's15 study, showed that school-aged children have a 9.5% incidence rate of asthma. A cross-sectional study comparing the incidence rate of asthma among Saudi schoolchildren in Yanbu (an industrial city) to Al-Furash and Al-Gafur (two non-industrial towns) showed a higher incidence rate of asthma (13.9%) in Yanbu than in those two towns (8%).16
The review of the literature on the asthma incidence rate in Saudi Arabia indicated that very limited information about the asthma incidence rate is available for the Taif region. Hence, the current study was an attempt to fill this gap by assessing the incidence rate of childhood asthma, and the role of associated sociodemographic and environmental risk factors on asthmatic severity and symptoms among asthmatic diagnosed and health control children aged 6 to 12 years: a retrospective cross-section study in the Taif region of Saudi Arabia, which can help health care programs to provide evidence-based health interventions.
Study subjects
A cross-section cohort study: The case-control study was conducted using an electronic medical questionnaire to estimate the incidence rate of BA among 6-12 school-aged children according to the International Study of Asthma and Allergies in Children (ISAAC) questionnaire method at schools, hospitals, and public clubs in Taif region, between February and April 2023 were included in this study validation.
Observational descriptive medical records of 2012 individual respondents: 1028 (51.09%) reported a bronchial asthma diagnosis children (cases group) are compared with other participants who are asthmatic free (non-asthmatic health control group). The socio-demographic, environmental characteristics and health-related risk factors of the respondent’s asthmatic and the health control of the respondents' Children were evaluated. In case-control study cohort studies, it is easier for investigators to establish a clear temporal relationship between exposure and outcome.
The chi-square test
The Chi-square test is often used in experimental work where the data consist of frequencies or counts. The most common use of the test is probably with categorical data such as gender, level of education, etc. The test can also be used in experiments designed to assess the effect of inoculation in immunizing people against disease and in clinical trials involving drugs.
The test is frequently employed to determine if there is an association between variables. When the word association is used in the statistical sense, a comparison is implied. A p-value less than or equal to 0.05 means the existence of significance. That means there is an association between the “group” and the variable tested. Otherwise, if the p-value is greater than 0.05 we say that the test is not significant (NS). That means there is no association between the “group” and the variable tested.
Descriptive questionnaires were filled out on 2012 participant’s populations among school-aged children and descriptive data were collected from several different hospitals, universities and clubs in Taif region. Out of the 2012 individual respondents, the incidence rate frequency of bronchial asthma was 1028 (51.09%) reported a bronchial asthma diagnosis and 984 (48.91) participants were non-asthmatic children (heath control).
Demographic characteristics of the respondents' children
The incidence rate of bronchial asthma in different age groups was represented in (Figure 1A) and indicated that the highest incidence percentages of asthmatic respondents, 370 (36%), followed by 344 (33.5%) and 314 (30.5%) respectively, and were aged (8-10 years), (10-12 years) and (6-8Years) respectively, while, 314 (30.5%), 370 (36%), and 344 (33.5%) percentages of non-asthmatic respondent's belonged to (6-8Years), (8-10 years) and (10-12 years) age groups respectively. According to sex groups of studied populations (Figure 1B), The obtained data show a significant relationship between bronchial asthma and gender, the p-value is <0.00001, indicating that, the male group represents 530 (51.6%) and 406 (41.3%) of asthmatic and non-asthmatic children’s respectively, as compared with female group were represent 498 (48.4%) and 578 (58.7%) of asthmatic and non-asthmatic children’s respectively.
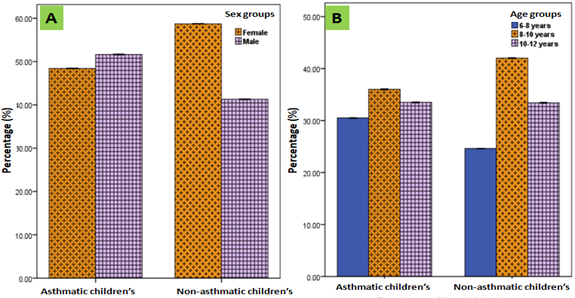
Figure 1 Incidence frequency of bronchial asthma in the study population according to age and sex groups.
The demographic characteristics of the respondents' children were represented in (Table 1), which shows that the incidence rate of bronchial asthma among the participants residing in rural and urban communities, 241 (23.4%) and 787(76.6%) respectively had asthma, as compared with 284 (28.9%) and 700 (71.1%) in rural and urban communities respectively. The obtained data show that most asthmatic children were Saudis, and the incidence rate of bronchial asthma 904 (87.9) and 774 (78.7%) were observed in children’s Asthmatic and Non-asthmatic Saudi children’s respectively, compared with 124 (21.1%) and 210 (21.3%) in Asthmatic and Non-asthmatic non-Saudis children’s respectively. No significant relationship between asthma incidence and month of birth. The high incidence rate of asthma, 970 (94.4%) was noticed among Primary school aged education compared with 58 (5.6%) Illiterate children, while almost half of the participants 480 (46.7%) had a family monthly income of 5000-10000 SR, but 343 (33.4%) had a family monthly income greater than 10000 SR. 528 (52.3%) of participants had a crowding index of fewer than six persons in family size, 447 (43.5%) of the respondents' father education status of asthmatic children’s were advanced graduated (above level), and 490 (47.7%) of the mothers educational status were advanced graduated, followed by 384 (37.4%), and 303 (29.5%) were secondary graduated of father and mother educational status respectively as compared with 361 (36.7%) and 414 (42.1%) respondents, advanced graduated father and mothers education status of non-asthmatic children’s respectively. About 300 (29.2%), and 291 (29.6%) of the respondent's mothers of asthmatic and non-asthmatic children respectively were housewives (Table 1).
|
Variable |
Asthmatic children's (No=1028) |
Non-asthmatic children's (No=984) |
Total No. (No=2012) |
Pearson (DF) |
p-value |
|||
|
|
No. |
(%) |
No. |
(%) |
No. |
(%) |
||
|
Month of birth |
||||||||
|
April-to-September |
481 |
46.8% |
527 |
53.6% |
1008 |
50.1% |
8.9404 (1) |
0.002789 |
|
October-to-March |
547 |
53.2% |
457 |
46.4% |
1004 |
49.9% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Nationality |
||||||||
|
Saudi |
904 |
87.9% |
774 |
78.7% |
1678 |
$3.4% |
30.601 (1) |
<0.00001 |
|
Non-Saudi |
124 |
21.1% |
210 |
21.3% |
334 |
16.6% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Child education |
||||||||
|
Illiterate |
58 |
5.6% |
68 |
6.9% |
126 |
6.3% |
1.1706 (1) |
0.2793 |
|
Primary school |
970 |
94.4% |
916 |
93.1% |
1886 |
93.7% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Residence |
||||||||
|
Rural |
241 |
23.4% |
284 |
28.9% |
525 |
26.1% |
7.3751 (1) |
0.006613 |
|
Urban |
787 |
76.6% |
700 |
71.1% |
1487 |
73.9% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Family size |
||||||||
|
Under six |
538 |
52.3% |
322 |
32.7% |
$60 |
42.7% |
95.932 (2) |
<0.00001 |
|
Six-to-eight |
331 |
32.2% |
367 |
37.3% |
698 |
34.7% |
||
|
Above eight |
159 |
15.5% |
295 |
30% |
454 |
22.6% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Income |
||||||||
|
Under 5K (low income) |
205 |
19.9% |
165 |
16.8% |
370 |
18.4% |
6.7158 (2) |
0.03481 |
|
5K to 10K (medium income) |
480 |
46.7% |
441 |
44.8% |
921 |
45.8% |
||
|
Above 10K (high income) |
343 |
33.4% |
378 |
38.4% |
721 |
35.8% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Father education |
||||||||
|
Illiterate |
66 |
6.4% |
35 |
3.6% |
101 |
5.0% |
32.126 (3) |
<0.00001 |
|
Primary |
131 |
12.7% |
200 |
20.3% |
331 |
16.5% |
||
|
Secondary |
384 |
37.4% |
388 |
39.4% |
772 |
38.4% |
||
|
Advanced |
447 |
43.5% |
361 |
36.7% |
SOS |
40.2% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Mother education |
||||||||
|
Illiterate |
85 |
8.3% |
58 |
5.9% |
143 |
7.1% |
20.849 (3) |
0.000113 |
|
Primary |
150 |
14.6% |
211 |
21.4% |
361 |
17.9% |
||
|
Secondary |
303 |
29.5% |
301 |
30.6% |
604 |
30.0% |
||
|
Advanced |
490 |
47.7% |
414 |
42.1% |
904 |
44.9% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Type of employment |
||||||||
|
Government employee |
181 |
17.6% |
122 |
12.4% |
303 |
15.1% |
0.00003 |
|
|
Housewife |
300 |
29.2% |
291 |
29.6% |
591 |
29.4% |
28.565 (5) |
|
|
Military |
91 |
8.9% |
137 |
13.9% |
228 |
11.3% |
||
|
Private sector employee |
185 |
18% |
156 |
15.9% |
341 |
16.9% |
||
|
Student |
193 |
18.8% |
223 |
22.7% |
416 |
20.7% |
||
|
Other |
78 |
7.6% |
55 |
5.6% |
133 |
6.6% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
Table 1 Demographic characteristics of the respondent’s children aged 6-12 years
*The Pearson Chi-square test (
)of independence (DF); the confidence interval (CI), using p-value in the range of 0.05-0.001: *, p-value<0.05; **, p-value<0.01; ***, p-value<0.001
The frequency of different environmental characteristics of the respondents' children as shown in (Table 2), the high asthmatic attack rate in asthmatic children 585 (56.9%) was observed in the winter season of asthmatic children as compared with 13 (1.3%) in non-asthmatic children’s. Hospital attendance frequency of 888 (86.4%) was reported in asthmatic children, and 906 (88.1%) of asthmatic children were living in well-lit and aired houses compared with 740 (75.2%) in the non-asthmatic health control group. Regarding the effect of asthma on the children, 736 (71.6%) reported living in a house without birds/animals with fur at home, compared with 551 (56%) of the healthy control group who reported living with birds/animals with fur at home.
|
Variable |
Asthmatic children's (No.= 1028) |
Non-asthmatic children's No. = 984) |
Total No. No. = (2012) |
Pearson (DF) |
p-value |
||||
|
|
No. |
(%) |
No. |
(%) |
No. |
(%) |
|
|
|
|
Season for asthma exacerbation |
12.228 (3) |
0.006641 |
|||||||
|
Autumn |
140 |
13.6% |
1 |
0.1% |
141 |
7.0% |
|||
|
Spring |
176 |
17.1% |
3 |
0.3% |
179 |
8.9% |
|||
|
Summer |
127 |
12.4% |
9 |
0.9% |
136 |
6.8% |
|||
|
Winter |
585 |
56.9% |
13 |
1.3% |
598 |
29.7% |
|||
|
Non-asthmatic |
- |
- |
958 |
97.4% |
958 |
47.6% |
|||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
|||
|
Hospital attendance |
|||||||||
|
Yes |
888 |
86.4% |
700 |
71.1% |
1588 |
78.9% |
681.61 (1) |
<0.00001 |
|
|
No |
140 |
13.6% |
284 |
28.9% |
424 |
21.1% |
|||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
|||
|
Suitable air and sun at home |
|||||||||
|
Yes |
55.607 (1) |
<0.00001 |
|||||||
|
No |
906 |
88.1% |
740 |
75.2% |
1646 |
81.8% |
|||
|
122 |
11.9% |
244 |
24.8% |
366 |
18.2% |
||||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
|||
|
Birds/animals with fur at home |
52.403 (1) |
<0.00001 |
|||||||
|
Yes |
292 |
28.4% |
433 |
44% |
725 |
36.0% |
|||
|
No |
736 |
71.6% |
551 |
56% |
1287 |
64.0% |
|||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
|
|
|
Table 2 Environmental risk factors of the respondents' children aged 6-12 years
*The Pearson Chi-square test (
) of independence (DF); the confidence interval (CI), using p-value in the range of 0.05-0.001: *, p-value<0.05; **, p-value<0.01; ***, p-value<0.001
Regarding data on health-related risk factors shown in (Table3), a low significant effect of Family history of bronchial asthma was observed in asthmatic children’s family, 520 (50.6%) without a family history of asthma, the family history, 197 (19.2%) was reported of children; mostly among their mothers, followed with 150 (14.6%) in fathers of asthmatic children’s, where both parents were 144 (14%) of asthmatic children’s were with family history with asthma. Regarding environmental asthma triggers, the most frequent allergens 405 (39.4) of asthmatic diagnosed children reported food allergies compared with 243 (24.7%) in non-asthmatic health control. Among asthmatic respondents, 315 (30.6%), and 46 (4.5%), fathers and mothers were smoking respectively, as compared with 231 (23.5%) and 121 (12.3%), fathers and mothers of health control respectively.
|
Variable |
Asthmatic children's (No.= 1028) |
Non-asthmatic children's (No. = 984) |
Total No. (No. = (2012) |
Pearson |
p-value |
|||
|
|
No. |
(%) |
No. |
(%) |
No. |
(%) |
|
|
|
Family history |
||||||||
|
Both parents |
144 |
14% |
99 |
10.1% |
243 |
12.1% |
55.34 (1) |
<0.00001 |
|
Father only |
150 |
14.6% |
105 |
10.7% |
255 |
12.7% |
||
|
Mother only |
197 |
19.2% |
120 |
12.2% |
317 |
15.8% |
||
|
Grandparent |
12 |
1.2% |
- |
- |
12 |
0.6% |
||
|
Relatives |
2 |
0.2% |
- |
- |
2 |
0.1% |
||
|
Siblings |
1 |
0.1% |
- |
- |
1 |
0.0% |
||
|
Sister |
1 |
0.1% |
- |
- |
1 |
0.0% |
||
|
None |
520 |
50.6% |
660 |
67.1% |
1180 |
58.6% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Food allergy |
||||||||
|
Yes |
405 |
39.4% |
243 |
24.7% |
648 |
32.2% |
49.099 (1) |
<0.00001 |
|
No |
623 |
60.6% |
741 |
75.3% |
1384 |
67.8% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Smoking status |
||||||||
|
Both are smokers |
47 |
4.6% |
141 |
14.3% |
188 |
9.3% |
21.626 (1) |
<0.00001 |
|
Father is a smoker |
315 |
30.6% |
231 |
23.5% |
546 |
27.1% |
||
|
Mother is a smoker |
46 |
4.5% |
121 |
12.3% |
167 |
8.3% |
||
|
None is a smoker |
620 |
60.3% |
491 |
49.9% |
1111 |
55.2% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
|
|
Table 3 Health-related risk factors of the respondents' children aged 6-12 years
*The Pearson Chi-square test (
) of independence (DF); the confidence interval (CI), using p-value in the range of 0.05-0.001: *, p-value<0.05; **, p-value<0.01; ***, p-value<0.001
Regarding the effects of severe asthma on asthmatic children in (Table 4), the most reported severe symptom was 729 (70.9%), 654 (63.6%), 601 (58.5%) of severe cases were reported Shortness of breath, Chest tightness and Cough respectively among patients, as compared a low frequency of symptoms attack health control, 16 (1.6%), 15 (1.5%0, and 11 (1.1%) were Chest tightness, Shortness of breath and Cough symptoms respectively. The highest frequency of asthmatic attacks in the patients' group, 299 (29.1%), and 266 (25.9%) were reported as twice a month and once a month respectively, compared with low-frequency asthmatic attack percentage, 49 (5%), 40 (4.1%), and 36 (3.7%) were noticed at once, three, and twice per month frequency in non-asthmatic group.
|
Variable |
Asthmatic children's (No. = 1028) |
Non-asthmatic children's (No. = 984) |
Total No. (No. = (2012) |
Pearson x2 |
p-value |
|||
|
|
No. |
(%) |
No. |
(%) |
No. |
(%) |
|
|
|
Shortness of breath |
729 |
70.9% |
15 |
1.5% |
744 |
37.0% |
1035.8 |
<0.00001 |
|
Chest tightness |
654 |
63.6% |
16 |
1.6% |
670 |
33.3% |
867.11 |
<0.00001 |
|
Cough |
601 |
58.5% |
11 |
1.1% |
612 |
30.4% |
778.44 |
<0.00001 |
|
Phlegm |
315 |
30.6% |
5 |
0.5% |
320 |
15.9% |
339.08 |
<0.00001 |
|
Wheeze |
459 |
44.6% |
9 |
0.9% |
468 |
23.3% |
536.3 |
<0.00001 |
|
Vomiting |
8 |
0.8% |
0 |
0% |
8 |
0.4% |
5.8487 |
0.01559 |
|
Nocturnal asthmatic attacks |
787 |
76.6% |
75 |
7.6% |
862 |
42.8% |
972.81 |
<0.00001 |
|
Frequency of attacks |
||||||||
|
Once a month |
266 |
25.9% |
49 |
5% |
315 |
15.7% |
57.419 |
<0.00001 |
|
Twice a month |
299 |
29.1% |
36 |
3.7% |
335 |
16.7% |
||
|
Three times a month |
200 |
19.5% |
40 |
4.1% |
240 |
11.9% |
||
|
Four or more per month |
120 |
11.7% |
69 |
70% |
189 |
9.4% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
|
|
Table 4 Asthma-related symptoms of the respondents' Children aged 6-12 years
*The Pearson Chi-square test () of independence (DF); the confidence interval (CI), using p-value in the range of 0.05-0.001: *: p-value<0.05; **: p-value<0.01, ***: p-value<0.001.
When exploring the social effects of bronchial asthma (Table 5), 320 (31.1%), 293 (28.5%), and 236 (23%) the most school absenteeism frequency was reported at three, two and four absenteeism days per month respectively in asthmatic children’s, as compared with 270 (27.4%), 262 (26.6%), and 249 (25.3%) school absenteeism frequency were reported three, one and two absenteeism days per month respectively in health control groups, 818 (79.6%) reported significant effects for asthma on activity/performance in asthmatic children’s, as compared with 10 (1%) in the healthy control group. And about 628 (31.9%) asthmatic respondents regularly had flu vaccine for many years, and 744 (72.4) took a medicine, 584 (56.8%) of them took inhalers drugs, 332 (32.3%) were taking oral medications. Good personal hygiene 668 (67.9%) and 924 (89.9%) were observed in health control and asthmatic children’s groups respectively. 590 (57.4%) and 639 (62.2%) of asthmatic cases were engaged in exercise and engaged in social activities respectively. The most barrier against engagement in social activities was fear of peer criticism in 372 (36.2%) asthmatic cases.
|
Variable |
Asthmatic children’s (No. = 1028) |
Non-asthmatic children’s (No. = 984) |
Total No. (No.= (2012) |
Pearson χ² |
p-value |
|||
|
|
No. |
(%) |
No. |
(%) |
No. |
(%) |
|
|
|
Absenteeism |
||||||||
|
One day per month |
179 |
17.40% |
262 |
26.60% |
441 |
21.90% |
24.961 (3) |
0.00002 |
|
Two days per month |
293 |
28.50% |
249 |
25.30% |
542 |
26.90% |
||
|
Three days per month |
320 |
31.10% |
270 |
27.40% |
590 |
29.30% |
||
|
Four days or more per month |
236 |
23% |
203 |
20.60% |
439 |
21.80% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Effect on activity/performance |
||||||||
|
Yes |
1937.9 |
<0.00001 |
||||||
|
No |
818 |
79.60% |
10 |
1% |
828 |
41.20% |
||
|
Non-asthmatic |
210 |
20.40% |
9 |
0.90% |
219 |
10.90% |
||
|
- |
- |
965 |
98.10% |
965 |
48.00% |
|||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Flu vaccine |
||||||||
|
Every year |
321 |
31.20% |
367 |
37.30% |
688 |
34.20% |
33.671 |
<0.00001 |
|
Some years |
328 |
31.90% |
372 |
37.80% |
700 |
34.80% |
||
|
Never |
379 |
36.90% |
245 |
24.90% |
624 |
31.00% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Taking medications? |
||||||||
|
Yes |
744 |
72.40% |
973 |
0.60% |
1717 |
85.30% |
1968.6 |
<0.00001 |
|
No |
284 |
27.60% |
6 |
- |
290 |
14.40% |
||
|
Not on medications (non-asthmatic) |
- |
- |
973 |
98.90% |
973 |
48.40% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Type of medications |
||||||||
|
Inhalation |
584 |
56.80% |
6 |
0.60% |
590 |
29.30% |
1964.6 |
<0.00001 |
|
Oral medication |
332 |
32.30% |
6 |
0.60% |
338 |
16.80% |
||
|
Injectable medication |
98 |
9.50% |
97 |
195 |
9.70% |
|||
|
All above |
11 |
1.10% |
- |
- |
11 |
0.50% |
||
|
No medication |
3 |
0.30% |
- |
- |
3 |
0.10% |
||
|
Not on medications (non-asthmatic) |
- |
- |
972 |
98.80% |
972 |
48.30% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Personal hygiene |
||||||||
|
Good |
924 |
89.90% |
844 |
85.80% |
1768 |
87.90% |
7.5919 |
0.005863 |
|
Poor |
104 |
10.10% |
140 |
14.20% |
244 |
12.10% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Engagement in exercise |
||||||||
|
Yes |
590 |
57.40% |
668 |
67.90% |
1258 |
62.50% |
23.18 |
<0.00001 |
|
No |
438 |
42.60% |
316 |
32.10% |
754 |
37.50% |
||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Engagement in social activities |
||||||||
|
Yes |
170.42 |
<0.00001 |
||||||
|
No |
639 |
62.20% |
862 |
87.60% |
1501 |
74.60% |
||
|
389 |
37.80% |
122 |
12.40% |
511 |
25.40% |
|||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
||
|
Cause for non-engagement |
||||||||
|
Cardiac disease |
||||||||
|
Epilepsy |
1 |
0.10% |
0 |
0% |
1 |
0.00% |
60.057 |
<0.00001 |
|
Fear of asthmatic attacks |
1 |
0.10% |
0 |
0% |
1 |
0.00% |
||
|
Fear of peer criticism |
372 |
36.20% |
18 |
1.80% |
390 |
19.40% |
||
|
Isolation |
166 |
16.10% |
43 |
4.40% |
209 |
10.40% |
||
|
No interest |
1 |
0.10% |
2 |
0.20% |
3 |
0.10% |
||
|
No cause |
9 |
0.90% |
4 |
0.40% |
13 |
0.60% |
||
|
6 |
0.60% |
1 |
0.10% |
7 |
0.30% |
|||
|
Total |
1028 |
100% |
984 |
100% |
2012 |
100% |
|
|
Table 5 Asthma-related social and school effects of the respondents' Children aged 6-12 years
*The Pearson Chi-square test (
) of independence (DF); the confidence interval (CI), using p-value in the range of 0.05-0.001: *: p-value<0.05; **: p-value<0.01, ***: p-value<0.001.
The respondents' population sex groups included 936 (46.52%) male participants population; 530 (51.6%) out of 936 were diagnosed with an asthmatic disease and 406 (41.3%) non-asthmatic health control group, While the female participants represent 1076 (53.48%) of studied population: 498 (48.4%) out of 1076 diagnosed with the asthmatic disease and 578 (58.7%) of non-asthmatic health control group.
Worldwide, 1-2% of children and adults suffer from asthma (Masoli et al., 2004).17 The incidence rate varies greatly between countries due to environmental factors, BA is one of the most prevalent chronic diseases in KSA, and local reports imply that it is becoming more prevalent, addition to utilizing various measurements (Al-Ghamdi et al., 2008).18 The incidence frequency and percentage of bronchial asthma were 1028 (51.09%) reported a bronchial asthma diagnosis was higher than that found in Riyadh (9.28%) and Dammam (3.59%) A Bener et al.19 Our result was also higher than that found in Bener et al.,20 who found that the incidence frequency of asthma in Yanbu, Saudi Arabia was 13.9%. The highest incidence rate of asthma was reported among the age group of 8-10 having a percentage of 36% followed by the age group of 10-12 (33.5%) and the age group 6-8 (30.5%) having the lowest incidence rate of asthma.
According to the Saudi Initiative for Asthma 2016, based on studies and data from the previous three decades, the total prevalence of BA among adults in KSA was estimated to be 8 to 25%.21 BA is one of the most prevalent chronic diseases in KSA, and local reports imply that it is becoming more prevalent.18 According to the Saudi Initiative for Asthma 2016, based on studies and data from the previous three decades, the total prevalence of BA among adults in KSA was estimated to be 8 to 25%.18
The incidence rate of physician-diagnosed asthma was reported to be 25% in 2004, which was the highest value in the last 30 years.13,23 Due to the globalisation and urbanisation of Saudi society, exposure to environmental agents like tobacco, dust, allergies, and sandstorms as well as changes in dietary practises, epidemiological research undertaken over the past three decades in the KSA has shown an increased incidence rate of BA.24,25
According to a recent survey on asthma control in KSA, just 5% of patients had their condition under control, while the numbers for patients who had it only partially or not at all were 31 and 64%, respectively.13,24,25
Our results agree with their result where half of the participants 46% from low-income families. The incidence rate of bronchial asthma among the participants residing in rural and urban communities was 241(23.4% and 787 (76.6%) in rural and urban communities respectively. According to Asher et al.,26 study, children from low-income families are more likely to experience asthma symptoms than children from high-income families. Children from low-income families had an asthma incidence frequency of 19.1%, compared to 8.2% for children from high-income households, and 14.4%, compared to 9.0% for children from low-income households in low-income nations.
The incidence rate of bronchial asthma 909 (87.9%) and 774 (78.7 %) were observed in children in asthmatic and nonasthmatic Saudi children respectively compared with 124 (21.1%) and 210 (21.3 %) in asthmatic and non-asthmatic non-Saudis children respectively. However, the majority of participants 1460 (85.9%) were Saudi while only 205(12.1%) were non-Saudi. The asthma rate was significantly higher among Saudi children 14.4 % than non-Saudi (5.9%) on this point Youssef et al.,27 found a higher rate of allergic disease among Saudi children than non-saudi. The high asthmatic attack rate in asthmatic children 585 (56.9%) was observed in the winter season of asthmatic children as compared with 13 (1.3 %) in non-asthmatic children's inside most of the asthmatic children participating in this study visited a family doctor once per season 51.4 % in the last 6 months while 14.0% of children have seen their doctor once per month 11% have mentioned that they visited their doctor once per 3 months. Although Al-Dawwod15 found that 65.2% of children in Alkhobar City have visited a hospital emergency service in the present academic year compared to 34.8 % of asthmatic school boys have used such services.
Regarding the effect of asthma on children 736 (71.6%) reported living in a house without birds and animals with fur at home though Al-Dawwod15 found a positive link between asthma and the presence of pets at home if you stay together with pets animals there are possibilities of getting Asthma. Here children have the highest risk of having asthma because both mother and father smoke. Regarding the effects of severe asthma on asthmatic children, the most reported severe symptom was 729 (70.9%), 654 (63.6%), and 60(58.5%) Of severe cases were reported shortness of breath chest tightness, and cough respectively among patients and a low frequency of symptoms attack health control 16 (1.6 %), 15 (1.5%) and 11(1.1) were chest tightness, shortness of breath and cough symptoms respectively although some results revealed that cough was the most frequently occurred symptoms 33.7% among asthmatic children. Difficulties in breathing were ranked the second common symptom at 21% while wheezing among children in Riyadh was 7.9% 12.13% and 11.86 respectively. The highest frequency of asthmatic attacks in the patient's group, 209 (29,1%) and 255 (25.9%) was reported as twice a month and once a month respectively, and low-frequency asthmatic percentages of 49(5%), 40 (4.1 %) and 36 (3.7%) were noticed at once, there and twice per month frequency in the nonasthmatic group. Although some parents have been asked about the frequency of their children suffering from asthma symptoms in the past 6 months, one of the respondents 33% indicated that their asthmatic children had asthma symptoms once per season while 25% of children mentioned that their children did not experience asthma last 6 months. Asthmatic children that experienced symptoms more frequently (once per month) constitute 16%. Regarding the effects of asthma on school absenteeism,320(31.1),293(28.5%), and 256 (23%) were the most school absenteeism frequency reported at their two and four absenteeism days per month respectively in asthmatic children however some participants found that asthmatic children did not absent from their schools in a past academic year, while the remaining (44%) were absent from school at varying levels through Al-Dawwod15 reported that the mean period of school absenteeism (13.6 = 3.4) in the academic year among asthmatic school children in Alkhobar city. Regarding asthma treatment 628 (31.9%) of asthmatic respondents regularly had flu vaccine for many years, 744 (72.4) took medicine, 584 (56.8%) of them took inhalers drugs,332 (32.35%) took oral medications, and the other 58.8 % of participants used inhalation bronchodilator the treatment of asthma while 200% of asthmatic children used syrup s0 the finding of this study was of diagnosis of asthma, about half 48.1% of children suffer from asthma symptoms were diagnosed less than 1 year from the start of the present study. Here, the researcher found that 590 (57.4%) and 639 (62.2%) of asthmatic cases were engaged in exercise and engaged in social activities respectively. And the most barrier against engagement in social activities was fear of peer criticism 372 (36.2) of asthmatic cases. However, Moamary et al.,14 found that exercise stimulated wheeze in 57.4% of school children in Riyadh. And Matsumoto et al.,28 found that a 6-week swimming program has a protective role against exercise-triggered asthma. Exercise-stimulated asthma could be due to a change in osmolarity of the lining fluid of the airways, possibly due to heat and water loss to the inspired air. However the exact mechanism is still not fully understood, and thus, further studies should be carried out to investigate such a mechanism. Hospital attendance frequency of 888 (86.4%) was reported in asthmatic children, and 906 (88.1%) of asthmatic children were living in well-lit and aired houses.
Asthma is still a highly prevalent chronic disease that contributes to the national and global burden of disease. Furthermore, Saudi Arabia is one of the largest countries in the Middle East, characterized by multiple factors associated with asthma, such as diverse geographical features, climates, rich social norms, and cultural aspects.
Regular monitoring and periodic reporting of the incidence frequency and severity of asthma symptoms and their related risk factors will provide reliable information for health authorities to improve health care and develop asthma control and prevention interventions.
The authors declare that there are no conflicts of interest.
This research would not have been possible without the efforts of my dear students throughout the work.
The researchers would like to acknowledge the Deanship of Scientific Research, Taif University for funding this work.

©2023 Alsolami, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
2 7