Advances in
eISSN: 2377-4290


Case Report Volume 15 Issue 2
University of the Philippines, Manila
Correspondence: Joyce Cassandra D. Ferma, O.D, LPU - St. Cabrini School of Health Sciences Inc. (College of Optometry), University of the Philippines, Amaris Homes, Molino 4, Bacoor City, Cavite, Manila, Tel (046) 537-5700
Received: April 08, 2025 | Published: June 3, 2025
Citation: Ferma JCD. Ectopia lentis and high astigmatism as ocular indicators of marfan syndrome in a 16-year-old male. Adv Ophthalmol Vis Syst. 2025;15(2):40-41. DOI: 10.15406/aovs.2025.15.00483
This case focuses on a 16 years old male patient who was recently diagnosed with Marfan syndrome after his first comprehensive eye exam. Ocular manifestation like ectopia lentis, high amount of astigmatism and irregular cornea has been recorded in this case. The importance of careful oculo-visual examination and possible management options in such patients are highlighted.
Keywords: ectopia lentis, vision, marfan syndrome, hypoplastic
Marfan's syndrome, a systemic genetic disorder affecting connective tissue, manifests through a wide array of degenerative changes across multiple organ systems, encompassing the skeletal, ocular, cutaneous, pulmonary, abdominal, neurological, and cardiovascular systems. The syndrome's etiology is most traced to abnormalities or mutations within the fibrillin-1 gene, which is located on chromosome band 15q15-21.1 In the context of the ocular system, fibrillin assumes a critical role as a major structural component of the zonules, which are responsible for maintaining the crystalline lens in its correct position.2 The weakening of the zonular fibers, often due to abnormalities or mutations in the FBN1 gene (which encodes fibrillin-1), results in the displacement of the crystalline lens—a condition known as lens subluxation.3 While this subluxation can occur in various directions (superior, inferior, nasal, or temporal), studies have shown that approximately 80% of syndromic cases, particularly those associated with Marfan syndrome, demonstrate a superotemporal displacement of the lens.
Ectopia lentis is a major ocular criterion for definitive diagnosis of Marfan's syndrome. Other minor features include increased axial length, flat corneal curvature,4 fluttering of the iris (iridodonesis) and hypoplastic iris or ciliary muscle causing decreased miosis (Figure 1).5
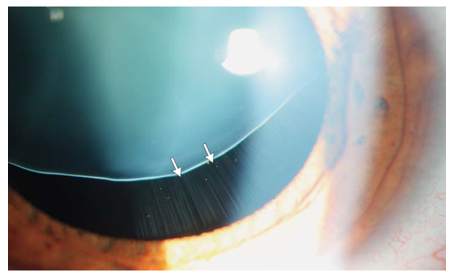
Figure 1 Ectopia Lentis in a patient with MFS with stretching of the zonular fibers (arrows).6
Marfan Syndrome is a condition associated with a shortened life expectancy, mostly due to aortic dissection. This complication often occurs before the age of 40 years.7 It is important to take note that once a patient is diagnosed with this condition, a cardio evaluation is a must to check if there is associated heart problems.
A sixteen-year-old male presented himself to the optical clinic for comprehensive eye examination last October 1,2022 with a chief complaint of blurring of vision at far. Vision on right eye was worse that his left eye, which was noticed 1 week prior to consultation. On physical examination, the patient appeared tall and thin, with long, slender fingers (arachnodactyly).
On ocular examination, his uncorrected visual acuity is 20/200 on both eyes, improving to 20/30 in the left eye, while the right eye had a visual acuity of 20/60 and pinhole acuity of 20/40.
During retinoscopy, patient’s red reflex seems irregular and additional testing for corneal topography has been requested due to the limitation of the clinic’s facility. Both subjective and objective testing reveals that the patient has high astigmatism. His subjective refraction is -1.25 = - 6.00 X 175 on his right eye while Plano = -6.00 x 5 on his left eye was recorded.
Patient was referred to seek ophthalmologist consult (refractive specialist) to rule out certain eye condition that might be affecting the vision.
The patient came back after few days for glasses prescription prescribed by the ophthalmologist. His mother mentioned how their check up went through. He first visited a pediatric specialist, then later referred for both refractive and retina specialist (ophthalmologist). He undergone series of test from corneal topography, to dilated fundus exam and fluorescein angiography. Cornea seems flat and irregular in curvature, and there are areas of retina that needs to undergo laser procedure to limit the risk of retinal tears and detachment.
Under slit lamp examination using 90 D, an ectopia lentis was observed on both eyes. Zonules are still intact with the lens.
Additional information for the patient’s history was reported by his mother regarding his appearance at birth. He was born with pigeon like chest in which the sternum (breastbone) protrudes, or sticks out, more than usual.
Flat cornea was observed on the patient's corneal topography and biometry, as indicated by low keratometry (K) readings of 36.92 D and 38.71D on his right eye while (K) readings of 37.5 D and 39.50 D on his left eye.
Ocular manifestations like ectopia lentis, flat cornea and high refractive prescription are some of the most common clinical pearl for Marfan syndrome.
For Treatment and Management
Marfan syndrome presents unique challenges for optometrists, primarily due to its systemic nature and the variability of its ocular manifestations. Refractive assessments in these cases can be particularly complex, as lens subluxation often leads to fluctuating or inconsistent refractive findings. Consequently, visual acuity may not significantly improve, even with optimal refractive correction, underscoring the importance of a thorough and individualized approach to care.
In children and adolescents with Marfan syndrome, ectopia lentis and iris transillumination defects are hallmark ocular features. Myopia is frequently observed, along with reductions in corneal curvature, central corneal thickness, and overall visual acuity.8
Eyeglasses are typically the initial approach used to improve visual clarity in cases of lens subluxation.4 In my patient’s case, the ophthalmologist advised prescribing optical correction due to the presence of mild lens subluxation observed during the ocular examination.
Patients require mandatory monitoring every three to six months to assess the progression of lens subluxation, detect any retinal changes, and evaluate for additional ocular abnormalities, such as angle structure anomalies, due to the increased risk of angle-closure glaucoma.
Surgical intervention for lens dislocation is indicated when optimal corrected visual acuity cannot be achieved, particularly in cases where there is a risk of amblyopia in pediatric patients; when the lens has dislocated posteriorly into the vitreous cavity or anteriorly (with or without secondary glaucoma); when there is an impending complete dislocation; or when complications such as lens-induced glaucoma, uveitis, or cataract are present.4
Marfan syndrome is a predominantly autosomal dominant condition with a reported incidence of 1 in 5,000 individuals.9 This case highlights the importance of recognizing the ocular manifestations of Marfan syndrome—particularly ectopia lentis, flat cornea, and high astigmatism—as key diagnostic indicators. Given the potential impact on a patient’s vision and quality of life, eye care practitioners must have a thorough understanding of the visual and structural implications of Marfan syndrome, which is essential for effective clinical management.
Additionally, because Marfan syndrome is a systemic disorder with potentially life-threatening cardiovascular complications, optometrists and ophthalmologists play a critical role in initiating timely referrals to cardiology and genetic counseling. Their involvement in a multidisciplinary care team helps ensure early diagnosis, ongoing surveillance, and comprehensive management, ultimately improving both visual and overall health outcomes for affected patients.
None.
The author declares that there are no conflicts of interest.
None.

©2025 Ferma. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.