Advances in
eISSN: 2377-4290


Case Report Volume 15 Issue 2
Department of Ophthalmology and Visual Sciences, Medical College of Wisconsin, USA
Correspondence: Alexandra J Beachnau, OD, FAAO, Department of Ophthalmology and Visual Sciences, Medical College of Wisconsin, Milwaukee, WI, USA
Received: June 15, 2025 | Published: July 2, 2025
Citation: Strombeck TJ, Beachnau AJ. Asymptomatic bilateral optic disc edema associated with newly diagnosed celiac disease: a case report. Adv Ophthalmol Vis Syst. 2025;15(2):55-58. DOI: 10.15406/aovs.2025.15.00486
Background: This report discusses a case of bilateral optic disc edema associated with celiac disease which resolved after many months of a gluten-free diet.
Case report: A 3-year-old white male, recently diagnosed with celiac disease, presented to our eye clinic for comprehensive exam after referral from plastic surgery due to craniosynostosis. Ophthalmic exam detected optic disc edema. Additional testing ruled out pseudo-papilledema, cranio- cephalic disproportion, and venous sinus thrombosis as the cause of the optic disc edema. After many months on a gluten free diet the optic disc edema resolved.
Conclusion: This case highlights one of the extra-intestinal manifestations of celiac disease and showcases the importance of screening eye exams for all patients with systemic diseases that have ophthalmic implications such as celiac disease and craniosynostosis.
Keywords: celiac disease, craniosynostosis, idiopathic intracranial hypertension, optic disc edema
Celiac disease is an autoimmune disorder in which genetically predisposed people have a reaction to the ingestion of gluten that leads to damage in the small intestine. It is a chronic condition which can result in malabsorption of nutrients into the body. Celiac disease is estimated to affect approximately 1% of the population.1 Extra-intestinal manifestations of celiac disease are now well established. Neurological manifestations can include ataxia, cognitive impairment, epilepsy, headache, and neuropathy.2 There are few reports in the literature detailing ophthalmic manifestations of celiac disease, including: nyctalopia, cataract, uveitis, vein occlusion, and neuro-ophthalmic manifestations.3 In this case report we present a patient with newly diagnosed celiac disease who was found to have bilateral optic disc edema. The optic disc edema resolved after many months of a gluten-free diet.
A 3-year-old white male was referred to our pediatric eye clinic by his plastic surgeon for comprehensive eye examination in the setting of craniosynostosis. The patient had a known prior history of Saethre- Chotzen syndrome, an autosomal dominant genetic condition characterized by coronal and/or metopic craniosynostosis, periorbital abnormalities, external ear anomalies, and midface abnormalities.4 This patient had metopic craniosynostosis for which he had undergone anterior cranial vault reconstruction with frontal orbital advancement two years prior. Incidentally, he was diagnosed with celiac disease 6.5 weeks before his visit to our eye clinic and had started a gluten free diet at that time. His family medical history was significant for maternal Saethre-Chotzen syndrome but was otherwise non-contributory. Notably he was in foster care. The patient and his foster family did not have any vision or neurologic concerns upon arrival.
Visual acuity without correction was 20/30 in the right eye and 20/40 in the left eye by blocked LEA symbols (LEA Test Intl. LLC, US). Pupils were equal, round, and reactive and were without an afferent pupillary defect. Confrontation visual fields were assessed with silent toys and were full in each eye. Extraocular motility was normal and there was no strabismus.
Stereopsis was assessed with the Lang Stereotest (Lang-Stereotest AG, Switzerland) and the patient appreciated 400 seconds of arc. Intraocular pressure was measured with iCare ® (iCare, Finland) and showed 21 mmHg in the right eye and 15 mmHg in the left eye. Anterior segment exam was unremarkable aside from downward slanting palpebral fissures. The patient was dilated with 1% cyclopentolate. Cycloplegic refraction showed moderate simple hyperopic astigmatism (+1.00+2.50x100 OD, +1.00+2.50x095 OS) for which glasses were recommended. The hyperopia was cut by one diopter since there was no esotropia. His best corrected visual acuity remained 20/30 in the right eye and 20/40 in the left eye.
Fundus exam revealed Frisen grade 3 optic disc edema in the right eye and Frisen grade 2 disc edema in the left eye (Figure 1).5 There was retinal blood vessel tortuosity noted bilaterally. There were no vitreous cell, and the remainder of the fundus exam was normal. When asked, the patient and his family denied symptoms of headaches, nausea, or vomiting.
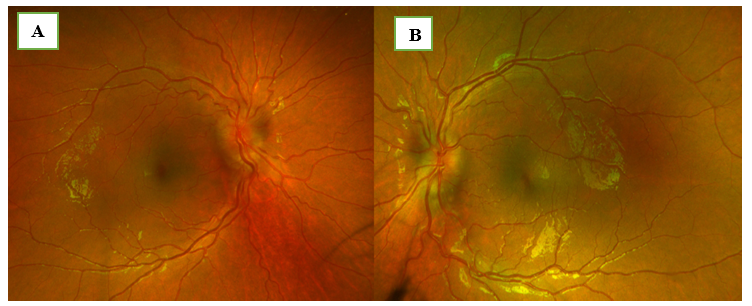
Figure 1 Fundus photography: Optos image of the right eye (A) with Frisen grade 3 optic disc edema and of the left eye (B) with Frisen grade 2 optic disc edema.
A B-scan was obtained and showed elevation of the optic discs consistent with optic disc edema but did not detect buried drusen. Optos imaging with fundus autofluorescence (Nikon Co Ltd, Japan) also did not detect buried drusen. A referral was made to neuro-ophthalmology, and an appointment was made with neurosurgery in 2 weeks. Unfortunately, the neurosurgery appointment had to be rescheduled due to the family having COVID-19 infection. Neurosurgery and plastic surgery decided to order magnetic resonance imaging (MRI) of the brain without contrast after the cancelled appointment, but the imaging was delayed due to the inability to obtain consent from the biological parents.
While awaiting consent to perform the magnetic resonance imaging, the patient was evaluated by neuro-ophthalmology. This examination confirmed moderate and diffuse bilateral optic disc edema. Notably, the patient remained asymptomatic. The magnetic resonance imaging was finally performed two months after the initial eye appointment. The imaging demonstrated posterior globe flattening bilaterally and prominent cerebral spinal fluid in the optic nerve sheaths, as well as evidence of the prior cranial vault reconstruction. The patient’s imaging did not suggest cranio-cephalic disproportion that could lead to increased intracranial pressure (ICP) given reassuring normal ventricle size. Therefore, neurosurgery ordered magnetic resonance venography (MRV) of the brain to evaluate for possible venous sinus thrombosis as the cause of optic disc edema. The magnetic resonance venography was unremarkable. Given the persistent concern for true optic disc edema rather than pseudo-edema, and evidence of increased intracranial pressure on magnetic resonance imaging, his neurosurgery team recommended that he undergo a period of intracranial pressure monitoring to assess for elevated intracranial pressure. After several months of delay, due to challenges in obtaining consent for the procedure, the patient underwent surgery to place a Camino intracranial pressure monitor (Natus Medical, US). No cerebral spinal fluid was drained or lost during placement of the device.
His intracranial pressure was monitored as an inpatient for two days until the device was removed. The intracranial pressure monitoring device registered an initial intracranial pressure of 24 mmH2O. Two days of monitoring showed a normal baseline of approximately 10 mmH2O. However, multiple transient “spikes,” many above 25 mmH2O were registered. The patient remained asymptomatic during the “spikes.” Historically intracranial pressure was considered elevated when higher than 18 mmH2O in prepubertal children.6 More recent evidence supports the use of 25 mmH2O to define elevated intracranial pressure in this population.7 Neurosurgery did not believe this represented elevated intracranial pressure and advised continued monitoring in the eye clinic (Figure 2).
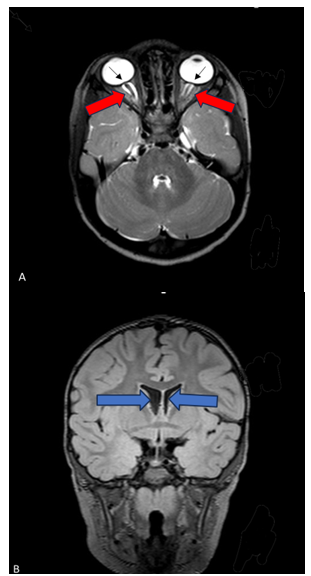
Figure 2 MRI imaging Axial 3D T-2 weighted MRI image depicting posterior globe flattening (black arrows) bilaterally and prominent cerebral spinal fluid in the optic nerve sheaths (red arrows) (A). Coronal 3D FLAIR MRI image demonstrating normal ventricle size (blue arrows) (B).
The patient returned to the eye clinic two weeks after the removal of the intracranial pressure monitor. His best corrected visual acuity tested with blocked LEA symbols was 20/50 in the right eye and 20/40 in the left eye. The remainder of his entrance testing and his anterior segment exam was unremarkable.
Intraocular pressure with iCare® tonometry was 20 mmHg in the right eye and 19 mmHg in the left eye. After dilation with 1% cyclopentolate the optic disc edema was found to be improving and was graded as 1 on the Frisen scale in each eye. Therefore, the decision was made to monitor closely without intervention given the significant improvement.
Four months later the patient presented to neuro-ophthalmology for follow-up. His acuity with pinhole testing was 20/40 in his right eye and 20/25 in his left eye. His pupils were equal and reactive without an afferent pupillary defect. Dilated fundus examination showed resolution of the optic disc edema in the right eye and minimal residual optic disc edema in the left eye.
The patient returned to the pediatric eye clinic three months after his exam with neuro- ophthalmology, which was approximately one year after his initial presentation. His best corrected visual acuity with blocked LEA symbols was 20/30 in his right eye and 20/25 in his left eye. His pupils were equal and reactive without an afferent pupillary defect. Intraocular pressure was measured as 19 mmHg OD and 17 mmHg OS with iCare® tonometry. The anterior segment exam was unremarkable. Dilation and cycloplegia were obtained with 1% cyclopentolate. A stable simple hyperopic astigmatic refractive error was found (plano+2.75x090 OD, +0.25+2.25x090 OS); new glasses were not advised, however, continued full time glasses wear was recommended. Dilated fundus exam showed flat, pink, optic discs with mildly indistinct nasal disc margins bilaterally. A small (0.05) cup was present in each eye. This was felt to represent resolution of the optic disc edema. Repeat exam approximately one year later showed continued stability. Best corrected visual acuity was 20/30 in the right eye and 20/25 in the left eye. Pupils were equal and reactive without an afferent pupillary defect. Anterior segment was unremarkable. Posterior segment exam after dilation with 1% cyclopentolate revealed flat, pink, optic discs with small cups (0.05) bilaterally and mildly indistinct nasal disc margins in each eye (Table 1).
|
Time point |
Event / visit |
Key findings & actions |
|
Initial visit (Age 3) |
Pediatric Eye Clinic |
History of Saethre-Chotzen syndrome; prior cranial vault reconstruction |
|
Recent diagnosis of celiac disease (6.5 weeks prior) |
||
|
VA: 20/30 OD, 20/40 OS (uncorrected) |
||
|
Moderate hyperopic astigmatism → glasses recommended |
||
|
Frisen grade 3 optic disc edema OD, grade 2 OS |
||
|
No buried drusen (Optos and B-scan) |
||
|
Referral to neuro-ophthalmology & neurosurgery |
||
|
~2 Weeks later |
Neuro-ophthalmology Evaluation |
Confirmed bilateral optic disc edema |
|
Patient asymptomatic |
||
|
MRI ordered but delayed due to parental consent issues |
||
|
2 Months after initial visit |
Brain MRI |
Posterior globe flattening bilaterally |
|
Prominent CSF in optic nerve sheaths |
||
|
Ventricles normal (no craniocephalic disproportion) |
||
|
MRV of the brain ordered |
||
|
4 Months after Initial Visit |
Brain MRV |
MRV was unremarkable |
|
Neurosurgery recommended ICP monitoring due to persistent concern for true edema |
||
|
5 1/2 Months after initial visit |
ICP Monitor Placement (Camino device) |
Initial ICP: 24 mmH2O |
|
Baseline ICP: ~10 mmH2O |
||
|
Transient spikes >25 mm H2O noted |
||
|
Patient remained asymptomatic |
||
|
Neurosurgery concluded no sustained elevated ICP |
||
|
6 Months after initial visit |
Pediatric Eye Clinic Follow-up |
VA: 20/50 OD, 20/40 OS (corrected) |
|
Frisen grade 1 edema OU (improving) |
||
|
No intervention; decision to monitor |
||
|
10 Months after initial visit |
Neuro-ophthalmology Follow-up |
VA: 20/40 OD, 20/25 OS (pinhole) |
|
Disc edema resolved OD, minimal residual OS |
||
|
1 Year after initial visit |
Pediatric Eye Clinic Follow-up |
VA: 20/30 OD, 20/25 OS (corrected) |
|
Refractive error stable |
||
|
Discs flat and pink with 0.05 cup OU |
||
|
Mild nasal disc margin indistinctness |
||
|
2 Years After Initial Visit |
Final Follow-up |
VA: 20/30 OD, 20/25 OS |
|
Discs remained flat and stable |
||
|
No evidence of active edema |
||
|
Mild nasal margin indistinctness persisted |
Table 1 Timeline summarizing key clinical evaluations, imaging, and outcomes for a 3-year-old male with Saethre-Chotzen syndrome presenting with bilateral optic disc edema
At initial presentation it seemed possible that this case represented pseudo-papilledema given the lack of symptoms and previous successful cranial vault remodeling for his craniosynostosis.
After ocular imaging failed to detect buried drusen and supported true optic disc edema, alternatives had to be entertained. While craniosynostosis seemed the most obvious culprit, neurosurgery felt this was less likely because the patient had already undergone cranial vault remodeling. Magnetic resonance imaging and intracranial pressure monitoring provided evidence that the disc edema was not attributable to the craniosynostosis. Additional imaging with magnetic resonance venography ruled out venous sinus thrombosis, a potential cause of elevated intracranial pressure and disc edema. After an extensive workup the cause of the bilateral optic disc edema remained elusive.
Buried disc drusen can be difficult to detect in young children. Fundus autofluorescence, although convenient for detecting more superficial drusen, can miss deeply buried drusen because the overlying tissue blocks autofluorescence.8 Even B-scan, long considered the gold standard in buried disc drusen detection, can miss deep and uncalcified drusen.9 Enhanced depth imaging (EDI) on Spectralis Optical Commuted Tomography (Spectralis OCT), now commonly considered to be the new gold standard, can detect buried drusen that are uncalcified, but this imaging can be difficult to obtain in very young children.10,11
Fortuitously, examination a short time after the intracranial pressure monitor was removed showed significant improvement in the disc edema. Since the patient received no intervention designed to decrease intra-cranial pressure or treat the optic disc edema directly, one must consider that his change to a gluten-free diet and improved nutritional status could be the factor that resulted in resolution of the disc edema. There are several case reports of optic disc edema and idiopathic intracranial hypertension associated with celiac disease in the literature. In two cases, idiopathic intracranial hypertension and papilledema were detected concurrently with the diagnosis of celiac disease. Treatment in both these cases included acetazolamide and a gluten free diet. The optic disc edema resolved with treatment and did not recur after cessation of the acetazolamide.12,13 In two other cases, idiopathic intracranial hypertension was detected and determined to have been caused by vitamin A deficiency. The vitamin A deficiency was later determined to have been caused by celiac disease. Those cases were treated with vitamin A supplementation and a gluten-free diet. In each case the optic disc edema resolved without known recurrence.14
Optic disc edema can be associated with vitamin A, B1 (thiamine), and B12 (cobalamin) deficiencies.15 Although vitamin levels were not checked for this patient, a small prospective study found vitamin B12 deficiency to be common (41%) in untreated celiac disease. They also found vitamin B12 values normalized after initiation of a gluten free diet.16 Another study found vitamin A and vitamin B12 deficiency to be present in 7.5% and 19% of newly diagnosed celiac patients respectively.17 Interestingly when looking at our patient’s growth curve, his height was at the third percentile for his age prior to starting the gluten-free diet and caught up to the 37th percentile approximately two years after starting the gluten free diet.
This case represents bilateral optic disc edema associated with newly diagnosed celiac disease. After an extended period of a gluten-free diet, the optic disc edema resolved. No other treatments, medications, or modifications were made that would otherwise explain the resolution of the optic disc edema.
This case highlights one of the rare, but important, extra-intestinal manifestations of celiac disease and showcases the importance of screening eye exams for patients with systemic ocular risk factors like craniosynostosis and celiac disease. No identifiable health information was included in this case report.
The authors thank Heather Stiff, MD and John Conto, OD, Dipl. AAO for their guidance in editing this report.
The author declares that there are no conflicts of interest.
None.

©2025 Strombeck, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.